|
|
|
Indian Pediatr 2021;58:363-366 |
 |
Analysis of Young
Infant Deaths Using Verbal Autopsies and Accuracy of Verbal
Autopsy Tool in Chennai, India
|
|
R Usha Devi, S Mangala Bharathi
and J Kumutha
From Department of Neonatology, Institute of Child Health and
Hospital for Children, Madras Medical College, Chennai, India.
Correspondence to: Dr Mangala Bharathi S, Professor, Department of
Neonatology, Institute of Child Health and Hospital for Children, Madras
Medical College, Egmore, Chennai 600 008, India.
Email:
[email protected]
Received: January 01, 2020;
Initial review: February 26, 2020;
Accepted: January 15, 2021.
|
Objective: To identify medical and
non-medical factors associated with young infant deaths using verbal
autopsies and to evaluate the validity of state verbal autopsy tool in
identifying medical causes. Design: Descriptive study to
report factors associated with young infant deaths, and diagnostic
accuracy study of the verbal autopsy tool. Results:
Prematurity related illnesses were the major contributors to mortality.
Deliveries were predominantly in health care facilities (99%); lower
maternal education (11.2%), lesser birth spacing (80%), and higher birth
order (7.5%) were other factors noted. Verbal autopsy questionnaire had
a diagnostic accuracy of ³95%
in identifying major causes of death (kappa value 0.8-1.0).
Conclusion: Current state verbal autopsy tool is valid in
identifying causes of death.
Keywords: Infant mortality, Newborn death, Still birth,
Janani suraksha yojna.
|
|
I ndia contributes to
22% of the global burden of under-5 deaths and nearly half of it
are neonatal deaths [1,2]. Routine registration systems do not
provide all information on causes of death and the contributory
factors. This affects strategy planning as well as
implementation of programs [2,3]. In such situations, detailed
child death review using verbal autopsy tool will be of great
help. Lack of a standardized verbal autopsy instrument and
administration methods are key challenges that remain unresolved
[4].
This study was conducted to identify factors
associated with young infant deaths using State verbal autopsy
questionnaire as a tool, and to evaluate its accuracy in
determining major causes of death.
METHODS
All young infant deaths (<2 months) between
April, 2013 to March, 2015 within Chennai Corporation zones were
included in the study. Investigation of these deaths was done
using State verbal autopsy forms. Maternal characteristics
recorded comprised of socio-demographic, pregnancy and delivery
details. Infant characteristics comprised of gender, birth
weight, gestational age, age at death, place of death and cause
of death. For neonatal deaths and post neonatal deaths, there
were set of questions under each cause of death (as per ICD-10
classification). Depending upon the answers, one of the major
causes was selected. The tool was used by field workers. They
were provided a structured training for two weeks where each
question in the tool and possible responses were discussed.
Clinical summaries of babies were collected
from health posts near their residence. Clinical diagnosis was
considered as the gold standard. The disease pathology which led
to deterioration of the baby and death was taken as main cause
of death. For home deaths, diagnosis on arrival to hospital or
in death certificate was taken.
Statistical analyses: We used descriptive
statistics to describe baseline variables. Diagnostic test was
used to estimate sensitivity, specificity, positive predictive
value and negative predictive value of verbal autopsy tool
taking hospital diagnosis as gold standard. Kappa statistics was
used to study agreement between verbal autopsy and clinical
diagnosis at different time periods after death [5]. We used
statistical software package SPSS version 13.0 for analyses.
RESULTS
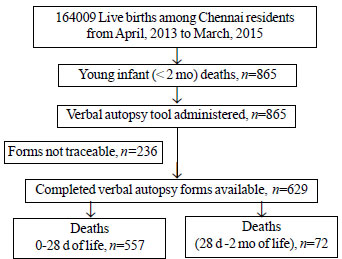
Of 164009 live births during the study
period, there were 865 young infant deaths, accounting for a
mortality rate of 5.2 per 1000 live births. Of these, we could
access only 629 records (Fig. 1), 319 in 2013-14, and 310
in 2014-15.
 |
|
Fig. 1 Flow diagram of the
study.
|
Consanguinity was noted in 20% of these
babies. Most mothers (95%) had
³3 antenatal
visits. 193 (31%) mothers had some antenatal illness, pregnancy
induced hypertension (14.1%) being the most common followed by
anemia (6.4%) and diabetes (5.9%).
Two third of the babies were low birthweight.
More than 99% of the deliveries were institutional. Among the
neonatal deaths, care was sought within 24 hours of identifying
illness in majority (75%) (Table I). Most of the babies
who died were preterm (55%) with 11.5% being extremely low
birthweight. The single most important cause assigned was
asphyxia (27%) followed by respiratory distress syndrome (20%),
sepsis (17%), congenital malformations/surgical cases (15%),
extreme prematurity (9%), heart disease (6%) and multiple
congenital anomalies (3.5%).
Table I Delivery Characteristics, Health Seeking Behavior, Access to Health Facilities and
Analysis of Home Deaths (N=629)
| Characteristics |
No (%) |
| Normal delivery |
354 (56.2) |
|
Place of deliverya |
|
| Level 1 |
86 (13.7) |
| Level 2 |
46 (7.3) |
| Level 3 |
497 (79) |
| Maturity |
|
| £28 wk |
84 (13.4) |
| 28-37 wk |
264 (42) |
| >37 wk |
281 (44.6) |
| Birthweight |
|
| <1 kg |
72 (11.4) |
| 1-1.5 kg |
119 (18.9) |
| 1.5-2.5 kg |
209 (33.3) |
| >2.5 kg |
229 (36.4) |
| Illness recognized by parents |
58(9.2) |
| Duration of illness prior to
seeking care |
|
| <24 hr |
187 (29.8) |
| 1-3 d |
155 (24.6) |
| >3 d |
287 (45.6) |
|
Health seeking behavior |
|
| Yes |
609 (96.8) |
| Transport mode (n=144) |
|
| 108 neonatal |
102 (70.8) |
| 108 general |
10 (6.9) |
| Private ambulance |
22 (15.2) |
| Travelling time (n = 144) <1 h |
89 (61) |
Analysis of home deaths (n=50)
Birthweight |
|
| <1.5 kg |
2 (4) |
| 1.5-2.5 kg |
14 (28) |
| >2.5 kg |
34 (68) |
| Postnatal age at death |
|
| <7 d |
9 (18) |
| 7-28 d |
25 (50) |
| >28 d |
16 (32) |
| Female |
30 (60) |
| Cause of death |
|
| Sudden infant death syndrome (SIDS) |
29 (58) |
| Aspiration |
15 (30) |
| Data represented as
no. (%); a home delivery in 1. |
According to verbal autopsy tool, asphyxia
(32%) was the single major cause of death followed by sepsis and
respiratory distress (17% each), congenital anomalies (8%) and
heart disease (6%); 10% of deaths were attributed to prematurity
alone. Around 30% of neonatal deaths happened within 24 hours of
life. There were 50 home deaths (5.7% of total deaths), 66% of
which happened between 6 PM and 6 AM (Table I).
Diagnostic accuracy of verbal autopsy tool in
identifying major causes of death was more than 95%. In the
diagnosis of prematurity, positive predictive value was low
(77%). Verbal autopsy tool had good agreement in all the major
causes with kappa values ranging from 0.82-0.90 (Table II).
Table II Accuracy of Verbal Autopsy Tool Compared With the Gold Standard (N=629)
| Diagnosis |
Sensitivity |
Specificity |
AUC |
Kappa |
| Birth asphyxia n=171 |
94.2% (89.5-97.2) |
96.9% (94.9-98.3) |
0.96 (0.94- 0.97) |
0.9 (0.86-0.94) |
| RDS + MAS n=137 |
82.5% (75.1-88.4) |
99.2% (97.9-99.8) |
0.91 (0.88-0.94) |
0.86 (0.81-0.91) |
| Neonatal sepsis n=108 |
90.7% (83.6-95.5) |
97.5% (95.8-98.7) |
0.94 (0.91- 0.97) |
0.87 (0.82-0.92) |
| Prematurity n=55 |
92.7% (82.4-98.0) |
97.4% (95.7-98.5) |
0.95 (0.92- 0.99) |
0.82 (0.75-0.90) |
| Values in measure (95%
CI); Pooled diagnostic accuracy was 92.2%. and Kappa of
0.90 (0.87-092); AUC: Area under the curve, RDS:
Respiratory distress syndrome, MAS: Meconium aspiration
syndrome. |
Only 21.9% of the verbal autopsy tool had
been administered within 14 days of death 21.4% were done
between 14 and 30 days and 32.9% after 30 days (maximum time of
administration, 360 days). Date was not mentioned in 24% of the
questionnaires. The sensitivity, specificity, positive, negative
predictive values and kappa agreement in our study was equally
good across various timeframes. However, the positive predictive
value for the diagnosis of prematurity was low and kappa
agreement for the same was moderate (Supp. Table I).
DISCUSSION
High institutional deliveries noted in the
study can be attributed to government programs providing
financial assistance to pregnant women like Janani Suraksha
Yojana (JSY) and Janani Shishu Suraksha Karyakaram (JSSK)
[6,7].
Majority of deaths happened in the first
three days after birth, similar to other studies [8,9], which is
directly related to antenatal, intra partum and immediate
neonatal care. Health-seeking behavior of the parents has
undergone a marked improvement when compared to previous studies
[10]. Access to transport has signi-ficantly increased because
of 108 neonatal services, which has helped in timely
stabilization and treatment. In the Million Death Study, the
major causes of death were prematurity, neonatal infections and
birth asphyxia [11]. Prematurity-related illnesses were the
major contributors in our study as well.
In many studies, the diagnosis of asphyxia is
collated into the prematurity complications, if gestation is
less than 34 weeks [12]. Currently, most studies based on verbal
autopsy assign a single underlying cause of death [13]. However,
some experts have suggested that this may not be the most
appropriate strategy and multiple causes of deaths should be
considered [14].
As a survey methodology, there is reason to
believe that recall bias may affect the validity of verbal
autopsy. WHO recommends that, after a period of mourning, the
verbal autopsy be conducted as soon as possible, and recalls of
more than one year should be interpreted with caution [15]. We
found good agreement at different periods of administration and
thus every effort should be made to fill the questionnaire even
if 14 days have elapsed since death.
Limitations of the study include lack of
separate set of questions in this tool for marking cause of
death as prematurity or respiratory distress syndrome, and its
inability to assign more than one cause of death. Missing verbal
autopsy forms could also have influenced the results of the
study. The limitations of medical records as a gold standard
needs to be recognized as case records may be incomplete and
relevant investigations may be missing.
We found State verbal autopsy tool valid in
identifying most of the common medical causes of young infant
deaths. We recommend incorporating this verbal autopsy tool even
in hospital death audits to capture significant non-medical
contributing factors.
Ethics Clearance: Institutional ethics
committee Madras Medical College, Chennai; No. ECR/
270/Inst./TN/2013/No.10012017, dated January 3, 2017.
Contributors: UDR: design of
study, data collection, data analysis, interpretation,
manuscript writing and draft preparation; MBS: data
interpretation, design, critical editing and draft preparation;
KJ: data interpretation, design, critical editing and draft
preparation. All the authors contributed to drafting of the
manuscript and approved the final version of the manuscript.
Funding: None; Competing interests:
None stated.
|
WHAT THIS STUDY ADDS?
•
The State verbal autopsy has a good accuracy in
ascertaining causes of death and also brings out the
improvement in non-medical factors, health care services
and health-seeking attitude over the years.
|
REFERENCES
1. Black RE, Morris SS, Bryce J. Where and
why are 10 million children dying every year?
Lancet.2003;361:2226-34.
2. Lawn JE, Cousens S, Zupan J, Lancet
Neonatal Survival Steering Team. 4 million neonatal deaths:
when? Where? Why? Lancet. 2005;365:891-900.
3. Lawn JE, Wilczynska-Ketende K, Cousens SN.
Estimating the causes of 4 million neonatal deaths in the year
2000. Int J Epidemiol. 2006;35:706-18.
4. Thatte N, Kalter HD, Baqui AH, Williams
EM, Darmstadt GL. Ascertaining causes of neonatal deaths using
verbal autopsy: current methods and challenges. J Perinatol.
2009;29:187-94.
5. Viera AJ, Garrett JM. Understanding
interobserver agreement: The kappa statistic. Fam Med.
2005;37:360-3.
6. Lim SS, Dandona L, Hoisington JA, James
SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a
conditional cash transfer programme to increase births in health
facilities: An impact evaluation. Lancet. 2010;375:2009-23.
7. Tripathi N, Saini SK, Prinja S. Impact of
Janani Shishu Suraksha Karyakram on out-of-pocket expenditure
among urban slum dwellers in northern India. Indian Pediatr.
2014;51:475-7.
8. Baqui AH, Darmstadt GL, Williams EK, et
al. Rates, timing and causes of neonatal deaths in rural India:
Implications for neonatal health programmes. Bull World Health
Organ. 2006;84:706-13.
9. Bapat U, Alcock G, More NS, Das S, Joshi
W, Osrin D. Stillbirths and newborn deaths in slum settlements
in Mumbai, India: A prospective verbal autopsy study. BMC
Pregnancy and Childbirth 2012;12:39.
10. Bhandari N, Bahl R, Taneja S, Martines J,
Bhan MK. Pathways to infant mortality in urban slums of Delhi,
India: implications for improving the quality of community- and
hospital-based programmes. J Health Popul Nutr. 2002;20:148-55.
11. Million Death Study Collaborators,
Bassani DG, Kumar R, Awasthi S, et al. Causes of neonatal and
child mortality in India: A nationally representative mortality
survey. Lancet. 2010;376:1853-60.
12. Soofi SB, Ariff S, Khan U, et al.
Diagnostic accuracy of WHO verbal autopsy tool for ascertaining
causes of neonatal deaths in the urban setting of Pakistan: A
hospital-based prospective study. BMC Pediatr. 2015;15:144.
13. Edmond KM, Quigley MA, Zandoh C, et al.
Diagnostic accuracy of verbal autopsies in ascertaining the
causes of stillbirths and neonatal deaths in rural Ghana.
Paediatr Perinat Epidemiol. 2008;22:417-29.
14. Anker M. The effect of misclassification
error on reported cause-specific mortality fractions from verbal
autopsy. Int J Epidemiol 1997;26:1090-6.
15. Manual for the training of interviewers on the use of the
2016 WHO VA instrument. World Health Organization; 2017.
|
|
|
 |
|

