|
|
|
Indian Pediatr 2020;57: 376-377 |
 |
Infantile Beri Beri: The Mizoram Experience
|
|
John Malsawma
Department of
Pediatrics, Synod Hospital, Durtlang, Mizoram, India.
Email:
[email protected]
|
|
In the land where the bamboo flowers, and where the population is
just over 10 lakhs, is the small North-Eastern state of Mizoram, from
where we would like to share our experience with infantile beriberi and
how we handled it.
In the last couple of years, from the months
of August-September to around February-March, we used to get very sick
infants aged mostly 6 weeks to about 3 to 4 months of age. The babies
usually came with complaints of lethargy, drowsiness, groaning, poor
feeding, sometimes with high shrill cries and sometimes with rapid
breathing – fever was noticeably absent. Most were hospital-born with
uneventful birth history. Their mothers had regular antenatal checkups
and were receiving iron/ folic acid and calcium tablets till before and
after delivery. All the babies were on exclusive breast feed. These
babies were mainly from low socio-economic status families.
At
first, our line of treatment was on the lines of infection/sepsis. But
in spite of giving all the best antibiotics and all supportive measures,
we kept losing these infants. When bird flu H1N1 cases were reported
from these South East Asia and India, we thought it might be a viral
cause and used Oseltamivir suspensions for such sick infants, but to no
avail. We contacted National Institute of Virolgy (NIV), Pune for
detailed virological analysis, but there was no response. Our diagnoses
for these infants varied from septicemia, viral encephalitis, right
heart failure (as echocardiographic findings showed pulmonary artery
hypertension, tricuspid regurgitation, and right heart dilatation) [1],
acute respiratory distress, shock etc as the final end stage
presentation. These deaths were an important component of the Infant
mortality rate (IMR) in Mizoram.
In December, 2014, having run
out of options, we started giving vitamin B-complex infusion (Vitneurin,
Beplex) along with the usual antibiotics and supportive care to these
infants. Following that practice, there was a dramatic change in the
outcome of these infants, and no more babies that came with these
symptoms died in our hospital after that period (Fig. 1).
We concluded that we were dealing with infantile beriberi, and giving a
bolus of thiamine infusion and seeing the clinical response is the best
diagnostic method [2].
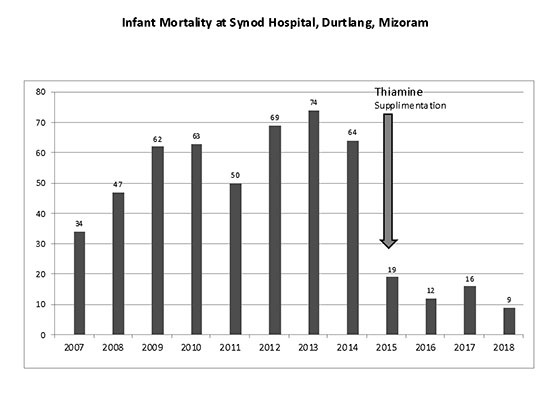 |
| Fig. 1 Infant
mortality at Synod Hospital, Durtlang before and after
routine thiamine supplementation in the post-partum
period. |
We presented our findings to the Department of Health
and Family Welfare of Mizoram (NHM) in Aizawl in March, 2015.
Convinced by our observations, a government order was issued for
all post-partum mothers to be given vitamin B complex tablets
from their time of delivery till their babies were six months of
age. These vitamin B complex tablets were to be dispensed from
the institution of delivery (District hospitals, PHCs, Sub
Centers) to last till their child’s first vaccination. Further,
vitamin B complex tablets were to be dispensed from sub- centers
on vaccination days.
The actions taken by the government
health authorities led to a marked decline in new cases of
infantile beriberi in the State of Mizoram. From 2015 onwards,
these cases just dried-up and the infant deaths dropped,
possibly also contributing to the lowering of infant mortality
rate of Mizoram.
Although, we did not find any
literature on universal B-complex supplementation for postpartum
mothers, it was better than waiting for infants to develop
beriberi.
We now know that thiamine deficiency is rampant
in Mizoram. These infants who died or came with the illness were
mostly low socio-economic families, the mothers were regular pan
chewers, and infants were on exclusive breast feeds. The risk of
beriberi is known to increase in individuals who consume a diet
high in thiaminase-rich foods (eg, raw freshwater fish or
shellfish, ferns), a diet high in anti-thiamine factors (eg,
tea, coffee, betel nuts), or both [3]. Since betel nuts cause
depletion in vitamin B1 stores and with a poor nutritional
intake, babies born to these mothers have a very poor chance of
survival. Breastfed infants whose mothers have thiamine
deficiency develop an infantile form of beriberi [4]. Providing
iron and calcium tablets to mothers does not help, if the mother
is thiamine-deficient [5].
Since supplementation for
pregnant women in India is only oral calcium, iron and folic
acid, it would be prudent to additionally provide vitamin B1, B6
and B12. This would go a long way in saving the lives of infant
born to thiamine-deficient mothers without additional
infrastructure and manpower inputs.
References
1. Jain SA, Kiran K, Krishna Kumar
R. Advances in pediatric cardiac emergencies. Indian J Pract
Pediatr. 2010;12:416.
2. Shivalkar B, Engelmann I, Carp
L. Shoshin syndrome: Two case reports representing opposite ends
of the same disease spectrum. Acta Cardiol. 1998; 53:195-9.
3. Vimokesant SL. Hilker DM, Nakornchai S, Rungruangsak
K, Dhanamitta S. Effect of betel nuts and fermented fish on the
thiamine status of Northeastern Thais. Am J Clin Nutr.
1975;28:1458-63.
4. Khounnorath S, Chamberlain K, Taylor
AM, Soukaloun D, Mayxay M, Lee SJ, et al. Clinically unapparent
infantile thiamine deficiency in Vientiane, Laos. PLoS Negl Trop
Dis. 2011;5:e969.
5. Mcgready R, Simpson JA, Cho T,
Dubowitz L, Changbumrung S, Böhm V, et al. Post-partum thiamine
deficiency in a Karen displaced population. Am J Clin Nutrition.
2001;74:808-13.
|
|
|
 |
|

