|
|
|
Indian Pediatr 2020;57:
362-364 |
 |
B-type Natriuretic peptide Levels and Outcome in Children
With Severe Acute Malnutrition With Co-morbidity
|
|
Dhilip Kumar and Sunil Kumar Rao*
Department of Pediatrics, Institute of Medical Science, Banaras
Hindu University,
Varanasi, Uttar Pradesh, India.
Email:
[email protected]
|
|
We studied the ability of B-type
natriuretic peptide (BNP) in predicting mortality among 86
in-patients with severe acute malnutrition presenting with
co-morbidity, and found that cut-off level of BNP
≥201 pg/mL in Receiver operating
characteristics curve [AU-ROC 0.96 (95% CI 0.92,1.003,
P<0.0001)] had high discriminative ability to distinguish
between survivors and non-survivors.
Keywords: Cardiac failure, Mortality,
Under-nutrition.
|
|
Pneumonia presenting with
respiratory failure is associated with heart failure, even in healthy
children without cardiac risks, and high mortality [1]. However, risk of
mortality and cardiac morbidity is further increased in pneumonia
occurring in children with severe acute malnutrition (SAM).The accuracy
of diagnosing heart failure in children with presenting with respiratory
distress is difficult clinically, as signs of heart failure are subtle
and mimic the features of SAM. Prior studies revealed increased levels
of BNP in pneumonia complicated with heart failure which returned to
lower levels with control of heart failure [2,3]. However, there is
paucity of data on BNP levels in children with SAN with pneumonia.
Present study, aims to identify levels BNP that predict mortality in
children with SAM with co-morbidities.
This case-control study
was conducted from September, 2016 to May, 2018 in a tertiary care
hospital in Northern India. Consecutive children, aged 6 to 60 months
fulfilling the WHO criteria of SAM were enrolled as cases [4]. Age- and
sex-matched children of age group 6 to 60 months with weight for
length/height >1SD, and mid upper arm circumference >13.5 cm and without
pitting edema were recruited as controls from well-baby clinic of the
department of pediatrics. The study was approved by the Institutional
ethics committee, and informed consent was obtained from the parents
before the study. Detailed history, clinical examination,
socio-demographic varia-bles, anthropometry, laboratory results,
diagnosis and outcome were recorded on pre-designed form.
Co-morbidity was defined as presence of one or more additional
conditions co-occurring in SAM children. Tachypnea was defined as
respiratory rate >50/minute in 6-12 months children and more than
40/minute in children 13-60 months. Tachycardia was defined as pulse
rate >160/minute in children up to one year and more than 140/minute in
children 13-60 months [4]. Clinical heart failure was defined as the
presence of tachycardia, tachypnea, triple rhythm, tender hepatomegaly
and engorged jugular veins [5]. Biochemically heart failure was defined
as BNP levels >300 pg/mL [6]. Investigations included arterial blood gas
analysis, serum electrolytes, calcium, serum albumin, blood sugar, X-ray
chest, and any other as per indication. The Alere Triage Cardio 3 panel
was used to estimate levels of BNP in SAM children and age- and
sex-matched healthy children as per manufacture’s guidelines.
For
sample size calculation, we measured BNP levels in 16 children with SAM
and found that mean (SD) BNP level was 22.6 (25.27) and ranged from 1.8
to 103 pg/mL. Considering £100 pg/mL as normal levels, and assuming 20%
increase in BNP levels in SAM children with co-morbidity, with power of
study as 90% and with alpha error of 0.05, a sample size of 75 SAM
children with SAM was required.
Data were analyzed by using SPSS
(version 16.0). The Receiver operating characteristic (ROC) curve
analysis was performed to obtain the area under the curve (AUC) as well
as the recommended cut-off point. Sensitivity, specificity, positive
predictive value, and negative predictive value was calculated.
Of the 86 children (65.1% males), the mean (SD) age of study population
were 28.8 (15.2) months and edematous children constitute 60.4% of
cases. Thirty-two (37.2%) presented with tachycardia, 53 (61.6%)
tachypnea, 31 (36%) with hypoxia (SpO2 <90%), and 18 (20.9%) with
hypotension. The co-morbidities were pneumonia 52 (60.4%), acute
diarrhea 54 (62.7%), and meningitis 18 (20.9%). Nine (10.4%) children
died and rest were discharged from hospital. SAM children dying in
hospital were more likely to have tachycardia and hypotension (P<0.001).
Among those dying in hospital, 7 presented with septic shock and 9 had
pneumonia with diarrhea. Of the 86 children, 32 had BNP levels >100pg/mL
and among increased BNP levels, 25 children had tachycardia. The median
(IQR) value of BNP in SAM children was 88 (31,117.5) pg /mL, in healthy
control children it was 14 (11.23, 18.62) pg/mL and in SAM children
without co-morbidity it was 14.5 (11.3, 25.18) pg/mL. There was no
difference observed in median (IQR) BNP levels between edematous and
non-edematous children [87 (26,111) vs 88 (28,109), P=0.69]. There was a
significant difference in BNP levels between children who survived and
those died, with respect to edema, tachycardia, tachypnea, and hypoxia
(Table I). AU-ROC curve revealed a cut-off levels of BNP ³ 201 pg/mL to
discriminate between survivors and non-survivors and this value had
sensitivity of 100%, specificity of 90.9%, positive predictive value of
56.2%, negative predictive value of 100%, and accuracy of 91.8%. AU-ROC
curve was 0.96 (95% CI 0.92, 1.003, P<0.001) (Fig. 1).
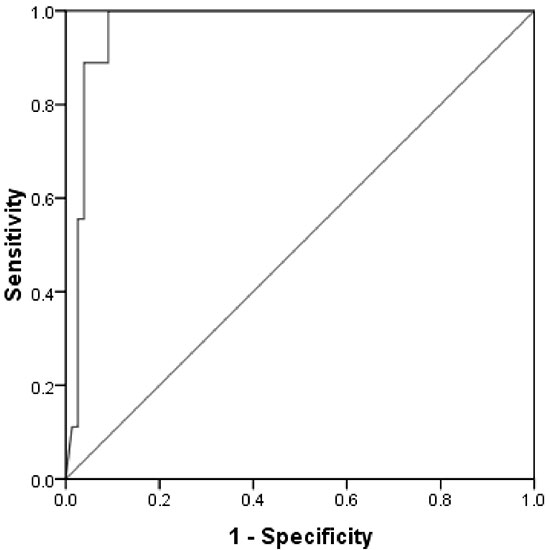 |
| Fig.1 Receiver
operating characteristic curve for BNP levels to predict
the death of hospitalized children with SAM. The area
under the curve was 0.96 (95% CI, 0.92 to 1.003,P<0.001)
for a level of ³201 pg/mL. |
Among clinical signs tachycardia had area under curve,
0.88 (95% CI 0.76, 1.002, P<0.001), revealing a cut-off levels
of BNP ³201 pg/mL to discriminate between survivors and
non-survivors and this value had sensitivity of 100% and
specificity of 69.6%.
The main finding of the present
study is that BNP levels increase significantly in pneumonia
with heart failure in children with SAM, and a cut-off levels
³201 pg/mL has the ability to differentiate between surviving
children and those dying in hospital. Similar observations have
been reported previously [2,7]. The increased levels of BNP in
pneumonia with heart failure are because of stimulation of
sympathetic nervous system, pro-inflammatory cytokines, and
further compounded by cardiac dysfunction [8]. There was no
difference between healthy controls and children with SAM
without co-morbidity, signifying that increased BNP levels may
be because of co-morbidity in children with SAM. The present
study showed that early clinically recognizable parameters like
tachycardia in heart failure and shock has good discriminative
ability to differentiate between survivors and non-survivors at
cut-off levels of BNP ³201 pg/mL. Echocardiography demonstrated
cardiac dys-function correlates with BNP levels, and a cut-off
level ³140 pg/mL in children with moderate heart failure is
associated with a higher risk for death [9]. A single BNP cutoff
value of 100 pg/mL had of an accuracy of 83% for differentiating
cardiac dyspnea from non-cardiac dyspnea in adults [10].
However, in children, a single BNP assay prior to treatment with
values >550 ng/L may indicate the presence of CCF in a child
with pneumonia, this might be because of lower age group in
study cohort by Sadoh, et al [7], as age has impact on BNP
levels. In the present study, lower cut-off of BNP to predict
mortality may be because of least variability of BNP levels in
age group of 1- 5 years.
We had few limitations in our
study, as we could not correlate the levels of BNP with
ventricular functions of heart and the cardiac mass. Our study
in an Indian setup, adds to the growing evidence all over the
world that in inconclusive clinical state of heart failure in
pneumonia, subtle features of heart failure and the BNP levels
³201 pg/mL with tachycardia in SAM children warrants the
clinicians to suspect and manage heart failure appropriately.
Contributors: DK: acquisition of data, analysis and
interpretation; SKR: concept, design, drafting of the
manuscript, critical analysis.
Funding: None; Competing
interest: None stated.
REFERENCES
1. Nimdet K, Techakehakij W. Congestive heart failure in
children with pneumonia and respiratory failure. Pediatr Int.
2017;59:258-64.
2. Hu D, Liu Y, Tao H, Gao J. Clinical
value of plasma B-type natriuretic peptide assay in pediatric
pneumonia accompanied by heart failure. Expt Therap Med.
2015;10:2175-79.
3. Osarogiagbon OW, Sadoh WE.
Socioeconomic and socio-demographic determinants of BNP values
in children with pneumonia in Benin city. Australasian Med J.
2017;10:432-8.
4. World Health Organization and the
United Nations Children’s Fund (2009).WHO child growth standards
and the identification of severe acute malnutrition in infants
and children. A Joint Statement. Available from:
http://www.who.int/maternal_child_adolescent/documents/9789241598163/en/.
Accessed September 14, 2019.
5. World Health
Organization. Management of severe malnutrition: A manual for
physicians and other senior health workers. World Health
Organization, WHO: 1999. Available from:
https://apps.who.int/iris/handle/10665/41999. Accessed
September12, 2019.
6. Obonyo N, Brent B, Olupot-Olupot P,
van Hensbroek MB, Kuipers I, Wong S, et al. Myocardial and
haemodynamic responses to two fluid regimens in African children
with severe malnutrition and hypovolaemic shock (AFRIM study).
Crit Care. 2017;21:103-16.
7. Sadoh WE, Osarogiagbon WO.
Role of Brain natriuretic peptide assay in identifying children
with pneumonia complicated by congestive cardiac failure. Annals
of Health Research. 2018;4:182-8.
8. Yetkin O,
Hacievliyagil SS, Gunen H. Assessment of B-type natriuretic
peptide in patients with pneumonia. Int J Clin Pract.
2008;62:488-91.
9. Auerbach SR, Richmond ME, Lamour JM,
et al. BNP levels predict outcome in pediatric heart failure
patients: Post hoc analysis of the Pediatric Carvedilol Trial.
Circ Heart Fail. 2010;3:606-11.
10. Maisel AS,
Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al.
Rapid measurement of B-type natriuretic peptide in the emergency
diagnosis of heart failure. N Engl J Med. 2002;347:161-67.
|
|
|
 |
|

