|
|
|
Indian Pediatr 2019;56: 299-303 |
 |
Comparison of Open and
Laparoscopic Appendectomy in Children: A 5-year Single Center
Experience
|
|
Zenon Pogorelic 1,2,
Mia Buljubasic2,
Tomislav Susnjar1,
Miro Jukic1, Tina
Poklepovic Pericic3
and Ivo Juric1,2
From 1Department of Pediatric Surgery,
University Hospital of Split; 2University of Split, School of
Medicine; and
3Department of Research in Biomedicine and Health, University
of Split, School of Medicine; Croatia.
Correspondence to: Dr Zenon Pogorelic, Department of
Pediatric Surgery, University Hospital of Split, Spinciceva 1, 21000
Split, Croatia.
Email: [email protected]
Received: December 14, 2017;
Initial review: May 01, 2018;
Accepted: December 31, 2018.
.
|
|
Objective: To compare the
outcomes of treatment in children with acute appendicitis between
laparoscopic and open surgical approaches.
Design: Retrospective study.
Setting: Division of Pediatric
Surgery at a tertiary-care hospital in Croatia between January 2012 to
December 2016.
Patients: 834 children [median
(IQR) age 13 (11,15)] who underwent appendectomy; 301 in the
laparoscopic group and 533 in the open group.
Main outcome measures:
Postoperative complications, duration of hospitalization, re-operation,
and the quantity of analgesics used.
Results: The median length of
hospital stay was 3 days in laparoscopic group compared to 6 days in
open group (P<0.001). The amount of analgesics used was lower in
patients with laparoscopic appendectomy compared to patients who
underwent open procedure (P=0.042). Significantly higher number
of wound infections was recorded in the open group (n=21; 3.9%)
compared to laparoscopic group (n=3; 1%) (P=0.014). The
frequency of re-operation in both groups was equal (1.3%). The median
duration of surgery was shorter in the group of patients with
laparoscopic appendectomy compared to the open approach (30 vs.
45 min; P<0.001). In five-year period, the proportion of
laparoscopic appendectomies increased by 21.5%.
Conclusion: Laparoscopic
appendectomy was safe and effective in children. Advantages of
laparoscopic approach were shorter hospital stay, lower number of wound
infections and lower usage of analgesics.
Keywords: Appendicitis, Complications,
Surgery, Treatment.
|
|
A
cute appendicitis is the most common surgical
condition in children and has a high rate of morbidity in children [1].
There are two possible operative approaches: laparoscopic, and the
classic approach, i.e. open appendectomy [1]. Nowadays, three
quarters of the appendices are removed laparoscopically [2]; however,
the efficacy and superiority of the laparoscopic appendectomy has been
under debate. The data favor laparoscopic appendectomy resulting in
shortened hospital stay, lesser postoperative pain, quicker overall
recovery, and lower rates of wound infections [3,4]. Laparoscopic
appendectomy over open appendectomy also benefits in a better
visualization and identification of other abdominal pathologies that can
mimic acute appendicitis [1,2]. However, several retrospective
investigations, randomized studies and meta-analyses which compared the
open and laparoscopic appendectomy have yielded mixed results [3-7].
We compared treatment outcomes of laparoscopic versus
open approach in children with acute appendicitis within a five-year
period.
Methods
Data of all children and adolescents (age 0-18 y) who
underwent appendectomy because of suspected acute appendicitis between
January 1, 2012 and December 31, 2016 in the Department of Pediatric
Surgery, at University Hospital of Split, Croatia, were included in the
study. Ethics Committee of University Hospital of Split approved the
study. Exclusion criteria were: patients with incomplete medical
documentation and the patients where another pathological cause was
found during the exploration of abdominal cavity. The case records of
all included children were retrospectively reviewed. Based on approach
used for appendectomy, the patients were divided into two groups: the
first group included patients who underwent a laparoscopic appendectomy,
while the second group included patients who underwent open
appendectomy. The choice of procedure was based on operating surgeon
preference. All surgeries were performed in emergency settings. The
following parameters were recorded for each patient: demographic data
(age, sex, Body mass index); preoperational laboratory tests (white
blood cell count, C-reactive protein); clinical data (duration of
symptoms, body temperature and local findings); treatment outcomes
(duration of surgery, hospital stay, number of re-operations);
intraoperative and postoperative complications; and need for analgesia
(quantity of analgesics). Preoperatively, all patients underwent a
clinical examination and laboratory analysis. ALVARADO score and
Pediatric appendicitis score were calculated in all patients [8]. In
most of the patients, abdominal ultrasonography was performed.
Open appendectomy: The patient was placed in
supine position. Modified Lanz incision was used. After opening of the
peritoneum, appendix was identified and pulled through the incision.
Mesoappendix was skeletonized in ante-grade fashion from tip to base
using absorbable suture (Vycril 3/0, Ethicon, Cincinnati, Ohio, USA).
The appendix was tied at the base and removed. Exposed mucosa at the
stump was cauterized. Stump inversion was performed by string
suture-knot.
Laparoscopic appendectomy: The patient was placed
in supine position, combined with the Trendelenburg position and left
lateral position. A Veress needle was introduced through 5-mm
supraumbilical incision and CO 2
was insufflated at a pressure of 8-12 mm Hg depending on patients’ age
and bodyweight. After achieving pneumoperitoneum through the same
incision, 5-mm trocar was introduced and a 5-mm scope was used.
Laparoscopic appendectomy was performed using a three-trocar technique
with a combination of 5- and 10-mm trocars. The mesoappendix was
dissected with either a harmonic scalpel (Ultracision, Ethicon
Endo-surgery, Cincinnati, OH, USA) or thermal fusion technology (MiSeal,
Microline, Beverly, Massachusetts, USA). Appendiceal base was secured
using endoloop (Vycril Endoloop-0, Ethicon Endo-surgery, Cincinnati,
Ohio, USA) or polymeric clips (Ligating Clips XL, Grena, Brentford, UK).
Each specimen was retrieved inside a disposable specimen retrieval bag (Ecosac
EMP 70, Espiner Medical Ltd.) through 10-mm trocar.
Antibiotics were used only in cases of perforated
appendicitis, or in cases when intraoperative perforation occurred. The
combination of gentamicin (3-6 mg/kg) and metronidazole (7.5 mg/kg) was
most commonly used.
In postoperative period, oral or intravenous
analgesics were used only on patient demand. Paracetamol (10-15 mg/kg)
or ibuprofen (10 mg/kg) were usually used. Pain assessments, including
patients’ self-reported pain intensity scores, was obtained and
documented at least once during every 12-hour shift, before pain
management interventions, and within one hour after the administration
of an analgesic. All documented pain intensity scores were extracted
from the patients’ medical records. Substantial pain was defined as mean
pain scores greater than four on a scale of zero to 10 in two or more of
the six-hour postoperative time intervals.
Criteria for discharge in children with uncomplicated
appendicitis included the adequate postoperative intake and pain
control. Similarly, children with complicated appendicitis were
considered ready for discharge once they had met the same criteria but
also had resolution of fever and return of normal white blood cell
count.
The outcome measures for comparison were the
postoperative complications, duration of hospitalization, percentage or
re-operations, and the quantity of analgesics demanded by the patients.
The intraoperative complications included access-related complications
such as organ lesions, thermal damage of intra-abdominal organs, and
intraperitoneal bleeding. Postoperative complications included wound
infection, bleeding, bowel obstruction, postoperative ileus and abscess
formation. The duration of surgery and the patients’ subjective
assessment of fitness after the operation were also compared in two
groups.
Statistical analysis: The data were analyzed
using the Microsoft Excel for Windows Version 11.0 (Microsoft
Corporation) and SPSS 19.0 (IBM Corp, Armonk, NY) software programs.
Distributions of quantitative data were described by means and standard
deviations, or medians and ranges, whereas absolute rates and
percentages were used to describe categorical data. Differences in
median values of quantitative variables between the groups of patients
were tested with Mann–Whitney U test. The chi-square test was used for
the statistical analysis of the categorical data. All values of P<0.05
were considered to indicate statistical significance.
Results
A total number of 855 patients underwent appendectomy
for suspected appendicitis during the study period. Twelve patients were
excluded from the study because they met one or more exclusion criteria.
Finally, 834 (62% males) patients with median age of 13 (IQR 11, 15)
years, and median BMI of 20 (IQR 18, 22) kg/m 2
were included in the study. Laparoscopic appendectomy was performed in
36% (n=316) and open appendectomy in 64% (n=533) patients.
An analysis of the patient data showed that there was
a significant statistical difference between the groups with respect to
age (P=0.025), body temperature (P<0.001) and
vomiting frequency (P=0.012). There were no significant
differences between the two groups regarding demographic data (age and
BMI), preoperative laboratory values (white blood cell count and
C-reactive protein level), or clinical data (duration of symptoms,
nausea and local clinical findings) (Table I).
TABLE I Baseline Characteristics of Patients Undergoining Appendectomy
|
Laparoscopic |
Open method |
|
method (n=301) |
(n=533) |
|
Age, y |
13 (13, 15) |
12 (9, 15) |
|
Male sex, n (%) |
175 (58) |
343 (64) |
|
BMI, kg/m2 |
20 (18, 22) |
19 (17, 22) |
|
*Leukocytes (x109/L) |
14.3 (11.3, 17.5) |
14.6 (11.3, 18.4) |
|
#CRP (mg/dL) |
22.4 (6.2, 54.9) |
23.9 (5.6; 55.6) |
|
Duration of symptoms (h) |
20 (12, 30) |
24(17, 48) |
|
*Body temperature, ºC |
37.3 (37.0, 37.7) |
37.1 (36.8, 37.5) |
|
Nausea, n (%) |
247 (82) |
438 (82) |
|
Vomiting, n (%) |
155 (52) |
212 (42) |
|
Pain migration to lower right quadrant of abdomen, n (%) |
241(80) |
431(81) |
|
Localized pain, n (%) |
244(81) |
451(85) |
|
All values in median (IQR) unless stated otherwise;
*P<0.001; #Preoperative values. |
TABLE II Treatment Outcomes of Children who Underwent Appendectomy
|
Laparoscopic method (n=301) |
Open method (n=533) |
|
Treatment outcomes |
|
|
|
*#Duration of surgery, min |
30 (25,45) |
45 (40,60) |
|
#*Hospital stay, d |
3 (3,4) |
6 (6,8) |
|
Reoperation, n (%) |
4 (1.3) |
7 (1.3) |
|
‡Complications, n (%) |
9 (1) |
32 (6) |
|
*Quantity of analgesics, n |
1 (0,3) |
1 (1,2) |
|
*Values in median (IQR); #P<0.001; ‡P<0.05. |
TABLE III Comparison of the Postoperative Compli-cations Depending on the Surgical Approach
|
Complication (n,%) |
Laparoscopic |
Open method |
|
|
method (n=301) |
(n=533) |
|
#Wound infection |
3 (1) |
21 (3.9) |
|
Intra-abdominal abscess |
5 (1.7) |
9 (1.7) |
|
‡Dehiscence |
1 (0.3) |
1 (0.2) |
|
Ileus |
0 |
2 (0.4) |
|
*Bleeding incision |
1 (0.3) |
0 |
|
#Total |
10 (3.3) |
33 (6.2) |
|
#P<0.05; *from operative incision; ‡of appendiceal stump. |
The median duration of surgery was 15 minutes shorter
in laparoscopic group (P<0.001) (Table II). The
median hospital stay was 3 days shorter in laparoscopic group compared
to open group (P<0.001) (Table II). Among the 834
patients included in the study, 41 (4.9%) postoperative complications
were recorded (P=0.031); 9 (1%) in laparoscopic and 31 (6%) in
open group (Table II). Wound infection rate was higher in
patients who underwent open appendectomy in relation to those who
underwent a laparoscopic appendectomy (P=0.014). The frequency of
other complications (intra-abdominal abscess, dehiscence of appendix
stump, ileus and operative incision bleeding) was comparable in both
groups (Table III). Most complications were treated
conservatively. A total of 11 patients required re-operation, 4 (1.3%)
patients in the laparoscopic group and 7 (1.3%) patients in the open
group.
Median quantity of analgesics used in postoperative
period was similar in both groups; though, somewhat lower quantity of
analgesics was used by patients who underwent laparoscopic appendectomy
in relation to the patients who underwent open appendectomy (P=0.042)
(Table II).
A histopathological analysis revealed a positive
diagnosis of appendicitis in 768 patients (96%). The analysis of all of
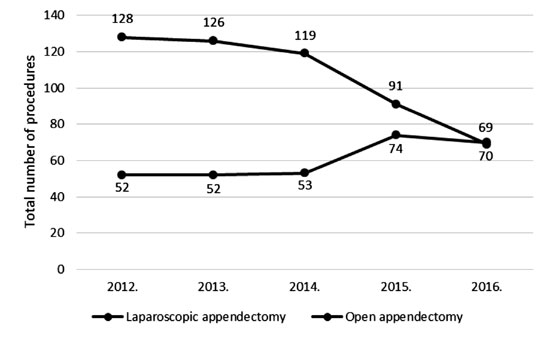
the appendectomies in 5-year period showed an increased frequency of
laparoscopic appendectomy from 28.9% to 50.4%, whereas a decline in open
appendectomies from 71.1% to 49.6% was recorded (Fig. 1).
 |
|
Fig. 1 Trend in use of surgical
approach for appendectomy.
|
Discussion
In this retrospective comparative study, we observed
that laparoscopic appendectomy in children was a safe and effective
surgical procedure with shorter duration of surgery and hospital stay,
and lesser frequency of complications and post-operative incisional
pain. Our results are in agreement with few other studies and
meta-analyses [3-7]. Our study also documented that the trend of
operative procedure in treating acute appendicitis has shifted in favor
of laparoscopic appendectomy at our institution. This concurs with the
earlier observations by Masoomi, et al. [5].
Retrospective nature and non-randomized comparison
are the main limitations of this study. As a higher proportion of cases
of laparoscopic appendectomy belonged to second half of our study
period, it is possible that some parameters improved because of general
improvement in healthcare services rather than because of the method of
surgery.
The length of hospitalization is an important factor
having a direct influence on patient management. The results of many
published studies also have shown that the length of hospitalization for
the patients who underwent laparoscopic appendectomy was significantly
shorter [5,7,9-12]. Postoperative complications are considered the best
method for evaluation for the safety of a particular procedure. The most
common complications of appendectomy are: wound infection,
intra-abdominal abscess, post-operative ileus and bleeding [9]. The
results of the meta-analysis performed by Wei, et al. [9] have
shown a lower complication rate in the patients who underwent
laparoscopic appendectomy. The rate of infection is lower in laparoscopy
because the inflamed appendix is pulled through a trocar, thus not
touching the abdominal wall. Visibility and magnification are much
better during laparoscopic procedure. Lower invasiveness of the
laparoscopic procedure, causing less damage to intestinal serosa, lowers
the adhesions-caused ileus rates [9]. Our study showed a statistically
significant lower rate of wound infection in patients who underwent
laparoscopic appendectomy. The frequency of other complications
(intra-abdominal abscess, appendix stump dehiscence, ileus and incision
bleeding) was similar in both groups. Similar results have been observed
in other published studies [5,9-11,13-15].
Most of studies recorded a longer duration of surgery
with laparoscopic approach than with open appendectomy [7,9-11,15]
whereas few studies reported similar or even shorter operating time with
laparoscopic approach [12-14]. Our study showed that the operating time
of the laparoscopic procedure was 15 minutes shorter than that of open
appendectomy. Better visualization during the laparoscopic approach and
the expertise of the operating surgeon are possible explanations for
shorter length of laparoscopic procedure. Also, device used for
skeletonization of mesoappendix and technique of securing of the
appendiceal stump in laparoscopic appendectomy may affect operating time
[2,16-20]. The incidence of thermal related injuries of the surrounding
tissues is significantly higher in laparoscopic surgery compared to the
open surgery, although in our study no case of thermal injury was
recorded [16,18-20]. Less postoperative pain, higher quality of life and
less amount of used analgesics is usually reported in patients who
underwent laparoscopic appendectomy [9,21]. In our study, the usage of
analgesics was similar in both groups; although, lower quantity of
analgesics was used in laparoscopic appendectomy patients.
In conclusion, laparoscopic appendectomy seems to be
a safe and effective procedure for children having appendicitis. It
results in less postoperative pain, and significantly reduces hospital
stay and postoperative wound infection. Duration of the surgery in hands
of experienced laparoscopic surgeon also may be lower in laparoscopic
appendectomy compared to open procedure.
Contributors: ZP: concept and design of the
study, analyzed the data; MB: collected the data and helped in data
analysis and drafting of the manuscript; TS: performed literature review
and drafted the manuscript; MJ: collected the data, drafted the
manuscript and revised manuscript critically; TPP: performed statistical
analysis of the data and contributed to manuscript writing; IJ:
supervised and revised manuscript critically for important intellectual
content. All authors approved the final version of manuscript and
agree to be accountable for authenticity and integrity of the work.
Funding: None; Competing interest: None
stated.
|
What Is Already Known?
• Open and
laparoscopic appendectomy are both safe but there has been a
controversy about which surgical procedure is the most
appropriate in children.
What This Study Adds?
• Laparoscopic surgery
for acute appendicitis in chidren seems to be superior to open
appendectomy in terms of length of hospital stay, rate of
postoperative wound infections and postoperative pain.
•
Duration of surgery in hands of
experienced laparoscopic surgery is shorter compared to open
surgery.
|
References
1. Stringer MD. Acute appendicitis. J Paediatr Child
Health. 2017;53:1071-6.
2. Pogorelic Z, Kostovski B, Jeroncic A, Susnjar T,
Mrklic I, Jukic M, et al. A comparison of endoloop ligatures and
nonabsorbable polymeric clips for the closure of the appendicular stump
during laparoscopic appendectomy in children. J Laparoendosc Adv Surg
Tech A. 2017;27:645-50.
3. Biondi A, Di Stefano C, Ferrara F, Bellia A,
Vacante M, Piazza L. Laparoscopic versus open appendectomy: A
retrospective cohort study assessing outcomes and cost-effectiveness.
World J Emerg Surg. 2016;11:44.
4. Çiftçi F. Laparoscopic vs mini-incision open
appendectomy. World J Gastrointest Surg. 2015;7:267-72.
5. Masoomi H, Mills S, Dolich MO, Ketana N,
Carmichael JC, Nguyen NT, et al. Comparison of outcomes of
laparoscopic versus open appendectomy in children: Data from the
nationwide inpatient sample (NIS), 2006–2008. World J Surg.
2012;36:573-8.
6. Faiz O, Blackburn SC, Clark J, Bottle A, Curry JI,
Farrands P, et al. Laparoscopic and conventional appendicectomy
in children: Outcomes in English hospitals between 1996 and 2006.
Pediatr Surg Int. 2008;24:1223-7.
7. Tan WJH, Pek W, Kabir T, Chan WH, Wong WK, Ong HS.
Clinical outcome and cost comparison between laparoscopic and open
appendicectomy. Ann Acad Med Singapore. 2014;43:464-8.
8. Pogorelic Z, Rak S, Mrklic I, Juric I. Prospective
validation of Alvarado score and Pediatric appendicitis score for the
diagnosis of acute appendicitis in children. Pediatr Emerg Care.
2015;31:164-8.
9. Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG,
et al. Laparoscopic versus open appendectomy for acute
appendicitis: a meta-analysis. Surg Endosc. 2011;25: 1199-208.
10. Ikeda H, Ishimaru Y, Takayasu H, Okamura K,
Kisaki Y, Fujino J. Laparoscopic versus open appendectomy in children
with uncomplicated and complicated appendicitis. J Pediatr Surg.
2004;39:1680-5.
11. Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X,
et al. Laparoscopic versus conventional appendectomy - a
metaanalysis of randomized controlled trials. BMC Gastroenterol.
2010;10:129.
12. Yau KK, Siu WT, Tang CN, Yang GP, Li MK.
Laparoscopic versus open appendectomy for complicated appendicitis. J Am
Coll Surg. 2007;205:60-5.
13. Cipe G, Idiz O, Hasbahceci M, Bozkurt S, Kadioglu
H, Coskun H, et al. Laparoscopic versus open appendectomy: Where
are we now? Chirurgia (Bucur). 2014;109:518-22.
14. Xiao Y, Shi G, Zhang J, Cao JG, Liu LJ, Chen TH,
et al. Surgical site infection after laparoscopic and open
appendectomy: A multicenter large consecutive cohort study. Surg Endosc.
2015;29:1384-93.
15. Tsai CC, Lee SY, Huang FC. Laparoscopic versus
open appendectomy in the management of all stages of acute appendicitis
in children: A retrospective study. Pediatr Neonatol. 2012;53:289-94.
16. Pogorelic Z, Katic J, Mrklic I, Jeroncic A,
Susnjar T, Jukic M, et al. Lateral thermal damage of mesoappendix
and appendiceal base during laparoscopic appendectomy in children:
Comparison of the harmonic scalpel (Ultracision), bipolar coagulation (LigaSure),
and thermal fusion technology (MiSeal). J Surg Res. 2017;212:101-7.
17. Rakic M, Jukic M, Pogorelic Z, Mrklic I, Klicek
R, Druzijanic N, et al. Analysis of endoloops and endostaplers
for closing the appendiceal stump during laparoscopic appendectomy. Surg
Today. 2014;44:1716-22.
18. Druzijanic N, Pogorelic Z, Perko Z, Mrklic I,
Tomic S. Comparison of lateral thermal damage of the human peritoneum
using monopolar diathermy, the Harmonic scalpel and the LigaSure. Can J
Surg. 2012;55:317-21.
19. Pogorelic Z, Perko Z, Druzijanic N, Tomic S,
Mrklic I. How to prevent lateral thermal damage on tissue using Harmonic
scalpel? Experimental study on pigs’ small intestine and abdominal wall.
Eur Surg Res. 2009;43:235-40.
20. Perko Z, Pogorelic Z, Bilan K, Tomic S, Vilovic
K, Krnic D, et al. Lateral thermal damage to rat abdominal wall
after harmonic scalpel application. Surg Endosc. 2006;20:322-4.
21. Liu Y, Cui Z, Zhang R. Laparoscopic versus open
appendectomy for diagnosed acute appendicitis in children. Indian
Pediatr. 2017;54:938-41.
|
|
|
 |
|

