|
|
|
Indian Pediatr 2018;55:315-318 |
 |
Second Dose of Scorpion
Antivenom in Children with Indian Red Scorpion (Mesobuthus
tamulus) Sting Envenomation
|
|
Anitha Abimannane, Ramachandran Rameshkumar,
Ponnarmeni Satheesh and Subramanian Mahadevan
From Division of Pediatric Critical Care, Department
of Pediatrics, Jawaharlal Institute of Postgraduate Medical Education
and Research (JIPMER), Puducherry, India.
Correspondence to: Dr Ramachandran Rameshkumar
Department of Pediatrics, Jawaharlal Institute of Postgraduate Medical
Education and Research (JIPMER), Puducherry-605 006, India.
Email:
[email protected]
Received: January 10, 2017;
Initial review: April 10, 2017;
Accepted: January 23, 2018.
Published online: February 09, 2018.
PII:S097475591600110
|
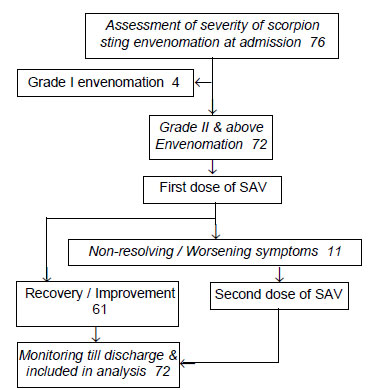
Objective: To study the effect of the second dose of scorpion
antivenom in children with non-resolving or worsening scorpion sting
envenomation. Methods: 72 children aged
£12
years with scorpion sting envenomation grade 2 and above were enrolled.
61 received the first dose of three vials of antivenom at admission
(group A). Children with persistent/worsening envenomation within 6
hours received the second dose (group B). The time required for
resolution of autonomic symptoms, myocardial dysfunction, predictors of
the second dose and side effects were studied. Results: The mean
time taken for resolution of autonomic symptoms were comparable in Group
A and B (4.1 vs. 5.3 h, P=0.4), and of myocardial
dysfunction was shorter in Group A (10.8 vs. 37.6 h, P=0.02).
On regression analysis, abnormal echocardiography at admission was found
to be a significant predictor of the second dose (OR=27.6, 95% CI,
4.7–162.5; P=<0.001). Conclusion: Children with severe
scorpion sting envenomation with abnormal echocardiography may require a
higher dose of scorpion antivenom. Trial registration:
CTRI/2015/03/005652.
Keywords: Autonomic dysfunction, Myocardial dysfunction,
Poisoning.
|
|
S
corpion sting envenomation is
a commonly
encountered emergency and preventable cause
of morbidity and mortality [1,2]. Symptoms
range from local pain to myocardial dysfunction and respiratory failure
in Mesobuthus tamulus sting envenomation, an important Indian
species [3,4].
In the management of scorpion sting envenomation, the
efficacy of Scorpion antivenom (SAV) has been shown in many studies
[2,5,6]. The current dose of SAV used in children is primarily based on
studies in the adult population [2,5]. Even after the use of 30 mL of
SAV, few children may deteriorate [5,7]. Antivenom, when injected
intravenously, binds to the venom and facilitates its excretion [8-10].
Subsequently, a concentration gradient of venom between the vascular
compartment and the peripheral tissue compartment facilitates the
redistribution of venom from peripheral tissues to the vascular
compartment from where the antivenom moderates further excretion of
venom [8-10]. The dose of SAV required seems to be related to the
severity of envenomation, but has not been well researched. The purpose
of this study was to describe the effect of the second dose of SAV in
children with non-resolving envenomation.
Methods
This prospective study was undertaken in the
Pediatric Critical Care Unit in a tertiary hospital in Puducherry
between April 2015 and July 2016. Approval was obtained from the
Institute Ethics Committee.
All children £12
years presenting with definite scorpion sting (red scorpion was seen by
bystanders/brought the killed scorpion or identified it on pictures) or
unknown bite with features of grade 2 and above scorpion sting
envenomation were included [2,5]. Grading of clinical features was done
as follows: Grade-1: local pain and reaction at the sting site,
without systemic involvement; Grade-2: Signs and symptoms of
autonomic storm characterized by parasympathetic or sympathetic
overactivity; Grade-3: Evidence of myocardial dysfunction
diagnosed when any one of the following were observed.
(a) Heart failure or cardiomegaly-
Clinically or by echo without previous heart disease (b) Required
an inotrope (³
5µg/kg/min of dobutamine or dopamine)/ hypotension with cold peripheries
(cold shock); Grade-4: Hypotension with warm peripheries
(warm shock) /Multiorgan dysfunction involving more than
two-organ.
All children showing envenomation-Grade 2 and above
were administered the first dose of three vials (30 mg) of SAV, i.e.,
a single 30 mL dose of monovalent M. tamulus antivenom (Haffkine
Biopharma, Mumbai) in 100 mL of normal saline, which was infused
intravenously over one hour. All children received oral prazosin (30
µg/kg/dose), and it was repeated every three hours until the extremities
were warm as per the assessment of treating team.
A second dose of three vials (30 mL) of SAV was
administered in case of persistence of an autonomic storm or worsening
to higher grades of envenomation within 6 hours of the first dose.
Children with myocardial dysfunction showing improvement in ejection
fraction or on a tapering dose of inotropes were not treated with the
second dose. The decision to administer the second dose of SAV was taken
by the treating team after documenting the eligibility criteria.
Clinical and biochemical data and investigations (CPK-MB, Troponin-I,
12-lead electro-cardiography (ECG) and echocardiography (ECHO) were
performed at admission, and six-hourly till recovery.
The patients were divided into Group-A (received 30
mL SAV) and Group-B (received 60 mL SAV) to determine the predictors of
the second dose of SAV. Continuous data, if normally distributed, was
compared by Student t test and, if non-normally distributed, was
compared by Mann-Whitney U test and proportions with chi-square test
(Fisher exact test if cell frequencies were small). Multivariate binary
regression analysis (backward: conditional method) with predefined
clinical variables was done to find out the predictors of the second
dose, and model fit was assessed with Hosmer and Lemeshow test. All
tests were two-tailed and P value <0.05 considered as
statistically significant. SPSS 20.0 software and Epi Info 7 was used
for data analysis.
Results
Seventy-six children with scorpion sting envenomation
were assessed for eligibility, and 72 were enrolled (Fig. 1).
Baseline characteristics, investigations, and intervention are
described in Table I. Cold peripheries (94.4%) and
Sweating (69%) were the most common symptoms observed. One child
in Group-A required mechanical ventilation for 6 hours for pulmonary
edema at admission due to excessive fluid administration at an outside
hospital.
 |
|
Fig. 1 Study flow chart.
|
TABLE I Baseline Characteristics at The Time of Enrollment into The Study
|
Variables |
Group A |
Group B |
P value |
|
(n=61) |
(n=11) |
|
|
Age* (mo)
|
45.8 (23.3,74.2) |
49.0 (24.1,7) |
0.91 |
|
Males
|
40 |
9 |
0.29 |
|
Grade at admission
|
|
|
|
|
Grade 2 |
49 (80.3) |
2 (18.2) |
< 0.001 |
|
Grade 3 |
11 (18) |
7 (63.6) |
|
|
Grade 4 |
1 (1.6) |
2 (18.2) |
|
|
Prazosin received outside
|
30 (49.2) |
10 (91) |
0.01 |
|
Vomiting
|
39 (63.9) |
6 (54.5) |
0.55 |
|
Sweating
|
59 (96.7) |
10 (90.9) |
0.39 |
|
Salivation
|
36 (59) |
6 (54.5) |
0.78 |
|
Priapism
|
30 (49.2) |
7 (63.6) |
0.69 |
|
Cold peripheries
|
57 (93.4) |
11 (100) |
0.38 |
|
Myocardial dysfunction |
12 (19.7) |
9 (81.8) |
< 0.001 |
|
Inotrope
|
10 (16.39) |
10 (90.90) |
<0.001 |
|
Hypertension
|
26 (42.6) |
4 (36.4) |
1.00 |
|
Hypotension
|
2 (3.3) |
2 (18.2) |
0.10 |
|
ECG abnormal
|
51 (83.6) |
11 (100) |
0.14 |
|
ECHO abnormal
|
12 (19.6) |
9 (81.8) |
< 0.001 |
|
Elevated CPK-MB
|
42 (68.8) |
9 (81.8) |
0.38 |
|
Elevated Troponin-I
|
12 (19.7) |
8 (72.7) |
<0.001 |
|
All values in n (%) except *median (IQR); SAV:Scorpion
antivenom; ECG: Electrocardiogram; ECHO: Echocardiography; CPK:
Creatine phosphokinase.
|
Eleven children with persistent/worsening symptoms at
the end of six hours received the second dose of SAV. The time taken for
the resolution of autonomic symptoms was similar between the two study
groups. Time take for normalization of ECG, ECHO, myocardial
dysfunction, and discharge was longer in Group-B as compared to Group-A
(Table II). No mortality was found in this study. By
multivariate logistic regression analysis, among the parameters included
(age, gender, time to the first dose prazosin and SAV, abnormal ECHO and
ECG), abnormal ECHO at admission significantly predicted the need for
the second dose (OR 27.6, 95% CI 4.7 to 162.5, R 2
=0.420, P=<0.001).
TABLE II Time (hours) to Resolution of Autonomic Symptoms, Myocardial Dysfunctions and
Outcome Measures in The Study Participants
|
Outcome |
All patients (n=72) |
Group A (n=61) |
Group B (n=11) |
Mean difference (95% CI) |
P value |
|
Sweating |
2.3 (1.3) |
2.9 (1.1) |
3.0 (2.7) |
-0.10 (-2.6 to 2.4) |
0.924 |
|
Salivation |
2.3 (1.4) |
2.09 (1.0) |
4.2 (3.9) |
-2.2 (-11.8 to 7.5) |
0.442 |
|
Priapism
|
3.5 (1.5) |
3.6 (1.2) |
2.8 (2.9) |
0.8 (-2.8 to 4.4) |
0.580 |
|
Cold peripheries |
4.1 (2.2) |
3.9 (1.1) |
5.3 (4.9) |
-1.4 (-4.9 to 2.1) |
0.390 |
|
Blood pressure |
3.9 (3.3) |
3.6 (3.1) |
5.7 (4.3) |
-2.1 (-5.4 to 1.2) |
0.201 |
|
Autonomic symptoms
|
4.2 (2.1) |
4.1 (1.1) |
5.3 (4.8) |
-1.2 (4.8 to -2.3) |
0.452 |
|
ECG abnormalities |
12 (13.9) |
8.6 (10.8) |
28.5 (16.2) |
-19.9 (-31.1 to -8.8) |
0.002 |
|
ECHO abnormalities |
17.4 (23.3) |
5.01 (3.4) |
31.2 (28) |
-32.2 (-52.2 to -12.2) |
0.002 |
|
Myocardial dysfunction |
22.5 (26.2) |
10.8 (19) |
37.6 (27.5) |
-26.7 (-48.4 to -5.1) |
0.019
|
|
Hospital stay |
64.4 (24.1) |
57.1 (15.3) |
104.7 (24.6) |
-47.7 (-58.7 to -36.6) |
<0.001 |
|
ECG: Electrocardiogram; ECHO: Echocardiography. All values
are expressed in mean (SD) in hours unless otherwise indicated.
P value by Welch’s t-test. |
Six (8%) of children had allergic reactions to SAV
(itching and rash; 4 during the first dose and 2 during the second
dose). In Group-A, two children developed hypotension along with rash
and managed by stopping SAV, fluid bolus, adrenaline, hydrocortisone,
and antihistamine. The premedication with intravenous chlorpheniramine
and H2 blocker (Ranitidine)
were given to all children, which prevented major reactions to SAV in
subsequently enrolled children.
Discussion
In this study, we documented efficacy of a
second dose of SAV in a subset of children with Indian red scorpion
sting envenomation who did not improve after the first dose. Abnormal
echocardiography at admission predicted the need for the second dose of
SAV.
This was only an exploratory study, and there was no
comparison arm to determine the efficacy of the second dose of SAV.
Moreover, the SAV used was only against Mesobuthus tamulus;
whether the results can be extrapolated to other scorpion species needs
to be studied further. The delay in recovery after two doses of SAV
could be due to two reasons; one is the severity of envenomation, delay
in giving the antivenom or insufficient amount of antivenom. Hence, it
is important to neutralize the venom in both vascular and the tissue
compartment; with a higher dose of SAV, this can be considered with
reasonable certainty, consistent with findings from other studies [6,9].
This would mean that children with severe envenomation might benefit
from 60 mL of SAV as the first dose at admission or an early
administration of the second dose of SAV (another 30 mL).
We conclude that children with severe scorpion sting
envenomation with abnormal echocardiography may require a higher dose of
SAV, and an initial dose of 60 mL of SAV at admission may be more
beneficial. The efficacy and safety of higher and repeated doses need to
be confirmed by controlled trials.
Acknowledgements: Mrs S Raja Deepa (JIPMER
Campus, Puducherry, India) for data entry and editing of the manuscript;
Mr. Rakesh Mohindra (Punjab University, Chandigarh, India) and Ms.
Thenmozhi M (CMC, Vellore, India) for helping with the statistical
analysis; and Ms. Harpreet Kaur (Punjab University, Chandigarh, India),
and Mrs Neelima Chadha (Tulsi Das Library, PGIMER, Chandigarh, India)
for helping with medical literature search.
Contributors: RR,SM: conceptualized the study,
contributed to review of literature and critically reviewed the
manuscript; AA: collected the data, reviewed the literature and drafted
the first version of manuscript. PS: contributed to review of literature
and performed the echocardiography. All authors were involved in the
management of the patients, and approved the final version of
manuscript.
Funding: JIPMER intramural research grant.
Competing interest: None stated.
|
What This Study Adds?
•
Abnormal echocardiography at
admission is a significant predictor of the requirement of
the second dose of SAV.
|
References
1. Chippaux J-P, Goyffon M. Epidemiology of
scorpionism: a global appraisal. Acta Trop. 2008;107:71-9.
2. Bawaskar HS, Bawaskar PH. Efficacy and safety of
scorpion antivenom plus prazosin compared with prazosin alone for
venomous scorpion (Mesobuthus tamulus) sting: randomised open
label clinical trial. BMJ. 2011;342:c7136.
3. Mahadevan S. Scorpion sting. Indian Pediatr.
2000;37:504-14.
4. Bawaskar HS, Bawaskar PH. Scorpion sting: update.
J Assoc Physicians India. 2012;60:46-55.
5. Pandi K, Krishnamurthy S, Srinivasaraghavan R,
Mahadevan S. Efficacy of scorpion antivenom plus prazosin versus
prazosin alone for mesobuthus tamulus scorpion sting envenomation in
children: A randomised controlled trial. Arch Dis Child. 2014;99:575-80.
6. Natu VS, Kamerkar SB, Geeta K, Vidya K, Natu V,
Sane S, et al. Efficacy of anti-scorpion venom serum over
prazosin in the management of severe scorpion envenomation. J Postgrad
Med. 2010;56:275-80.
7. Kumar PM, Krishnamurthy S, Srinivasaraghavan R,
Mahadevan S, Harichandrakumar KT. Predictors of myocardial dysfunction
in children with Indian red scorpion (Mesobuthus tamulus) sting
envenomation. Indian Pediatr. 2015;52:297-301.
8. Hammoudi-Triki D, Ferquel E, Robbe-Vincent A, Bon
C, Choumet V, Laraba-Djebari F. Epidemiological data, clinical admission
gradation and biological quantification by ELISA of scorpion
envenomations in Algeria: effect of immunotherapy. Trans R Soc Trop Med
Hyg. 2004;98:240-50.
9. Sevcik C, D’Suze G, Díaz P, Salazar V, Hidalgo C,
Azpúrua H, et al. Modelling Tityus scorpion venom and antivenom
pharmacokinetics. Evidence of active immunoglobulin G’s F(ab’)2
extrusion mechanism from blood to tissues. Toxicon. 2004;44:731-41.
10. Ghalim N, El-Hafny B, Sebti F, Heikel J, Lazar N, Moustanir R,
et al. Scorpion envenomation and serotherapy in Morocco. Am J Trop
Med Hyg. 2000;62:277-83.
|
|
|
 |
|

