n medicine, a great deal of professional learning
occurs in the authentic work- environment, where residents learn on the
job, when they are exposed to real problems in daily practice [1]. One
of the outcomes of training during residency is to ensure that trainees
ultimately improve their patient-care practices. In order to achieve
this, residents must be able to evaluate their patient-care practices,
identify their strengths and deficiencies, and gather and critically
analyze scientific evidence. Having done this, they must be able to set
learning goals to offset their deficiencies and make feasible plans to
achieve them. The Accreditation Council for Graduate Medical Education
(ACGME) calls this competency Practice-based learning and improvement
(PBLI) [2,3]. The ACGME believes that assessment of these competencies
provide evidence of the effectiveness of the residency program and also
provide information to improve it further [4].Training in PBLI has also
been shown to lead to improved health outcomes in preventive care [5],
chronic disease management [6], and patient-safety [7].
The Medical Council of India (MCI) advocates that
postgraduate training should be competency-based and essentially
self-directed [8]. However, PBLI as a competency is not explicitly
stated in this document. There is also lack of expertise in teaching and
assessing PBLI in India. In teaching hospitals, the pressure of clinical
work often takes priority over resident-training. While residents are
expected to provide service, they must not be short-charged regarding
the quality of teaching. The prevailing scenario can be improved by
explicitly incorporating elements of PBLI in the residency training
curriculum.
Concept and Components
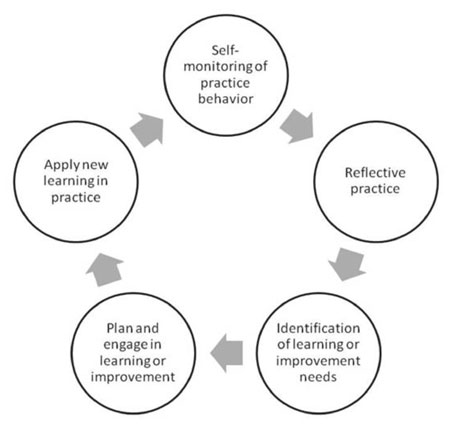
Practice based learning and improvement is best
described as a cyclical continuous process (Fig. 1) [9].
In an attempt to link education to quality of patient care, the ACGME
Outcome Project [10] defined eight constituent components under the core
competency of PBLI, which are summarized in Box 1.
 |
|
Fig.1 Cycle of practice-based learning
and improvement.
|
|
Box 1
ACGME Components of Practice-based Learning and Improvement
|
|
In order to acquire the core competency of practice-based
learning and improvement, the learner should be able to:
1. Identify strengths, deficiencies and
limits in one’s knowledge and expertise
2. Set learning and improvement goals
3. Identify and perform appropriate learning
activities for personal and professional development
4. Incorporate formative evaluation feedback
into daily practice
5. Systematically analyze practice and
implement changes to improve practice
6. Locate, appraise, and assimilate evidence
from scientific studies
7. Use technology to optimize learning and
health care delivery
8. Participate in the education of patients, families, fellow
students and other health care professionals.
Source: Swing SR. The ACGME outcome project:
retrospective and prospective. Med Teacher. 2007;29:648-54.
|
Defining Milestones
In a competency-based education and training system,
the unit of progression is ‘mastery’ of specific knowledge and skills
[11]. The ACGME has defined the levels of proficiency expected at each
learning level [12]. Milestones have been identified for each
competency, which describe the performance level of skills, knowledge or
behavior that a learner is expected to demonstrate at a certain level of
professional development [13]. Breaking down these competencies into
observable milestones is useful both to the learner and to the assessor
as they help in determining an individual learner’s trajectory from a
beginner to a proficient practitioner.
ACGME suggests writing five levels of milestones [14]
based on the Dreyfus model of skill development [15], as discussed in an
earlier paper [16]. Milestones have been defined specifically for
different clinical specialties [11]. For Pediatrics, milestones under
different components of PBLI have been defined in several ways [17-22].
Web Table I illustrates different milestones under each
competency and provides practical examples of these.
Each of these PBLI competencies are discussed in
detail below:
1. Identify strengths, deficiencies and limits in
one’s knowledge and expertise
Learners may be able to identify their deficiencies
and limits because they are either: Motivated by external threat of a
negative consequence; e.g. punishment, morbidity, bad grades; or
Motivated by external positive consequence; e.g. reward, good
scores in examination, praise from superior; or Intrinsically motivated
by reward: such as ease of work, comfort, satisfaction of learning; or
Intrinsically motivated to excel and acquire expertise.
Identification of gaps serves as a stimulus to
identify their strengths and limitations in performance, by working hard
to master skills against required standards. Kolb [23] suggests that
when learners perceive gaps in knowledge, skills and attitudes on
reflecting on their experiences, they tend to engage in active
experimentation like applying new strategies to learn further. Schon’s
model [24] talks of the importance of reflection either before
("reflection for action") or during ("reflection in action") or after a
particular action ("reflection on action"). This pushes learners to seek
new knowledge in ambiguous situations and incorporate new knowledge into
practice.
2. Set learning and improvement goals
Self-directed learning is a process in which
"individuals take initiative (with or without the help of others) to
diagnose their own learning needs, formulate goals, identify human and
material resources for learning, choose and implement appropriate
learning strategies and evaluate learning outcomes" [25]. This task
requires them to formulate both short-term and long-term learning and
improvement goals. Triggers to discovering new learning needs can be:
questions which arise during patient care, while reading, during
conversations with other peers or while attending formal academic
sessions. Self-directedness is influenced by factors such as motivation,
self-regulation and self-efficacy [26].
3. Identify and perform appropriate learning
activities for personal and professional development
Learners must be aware of their preferred learning
styles [23] and must have sufficient understanding of what they need to
learn (in terms of knowledge, skills, behavioral change). They also need
to know what instructional methods most effectively and efficiently
address their specific learning needs and where they can access these
resources. This may require considerable discussion, consultation and
trial-and-error before identification of strategies that work best for
them.
4. Incorporate formative evaluation feedback into
daily practice
Formative feedback intends to improve specific
aspects of a learner’s performance by offering insight into their
behavior, rather than offering a judgment on overall performance [27].
Learners must eventually learn not only to listen to feedback and
incorporate it into their practice, but also be proactive in seeking
feedback for improvement. In practice, a learner must be aware of his
limitations and must know when a situation requires him to summon help
from a superior without compromising the safety of a patient.
5. Systematically analyze practice using quality
improvement methods and implement changes
Residents are expected to be able to apply their
knowledge of desired standards of patient care, standard protocols,
evidence-based guidelines and principles of quality improvement in their
day-to-day practice. They need to imbibe reflective practice and learn
how to manage change. If individuals are not trained in reflective
practice, they may turn defensive, when shown evidence for their need to
improve. In early stages, their focus might be on individual patients.
However, in the long run, clinicians will need to shift their focus to
their teams and to the system [28]. This can be taught by integrating
residents in the team which is involved in the hospital’s quality
improvement programs [29]. For example, an effort to improve the care of
low birth weight babies should also include attention to the system –
like the process of recording weight, record keeping, training of nurses
and other care providers, provision of nutritional advice and
availability of educational material.
6. Locate, appraise, and assimilate evidence from
scientific studies related to health problems of patients
The amount of medical information is ever-increasing
and clinicians must learn strategies to search for the evidence and
apply it in their practice [30]. Confronted with uncertainty in a
clinical case, the learner must be able to actively question the
rationale of patient care. For example, ‘In this patient, what is the
best antibiotic we should be using? What is the evidence we have for
this decision?’
One cannot practice evidence-based medicine (EBM)
without being able to set improvement goals for oneself or without being
motivated to be a lifelong learner. The skills required to be learnt in
order to practice have been detailed previously [17].
The milestones which characterize learners in various
stages of development of this sub-competency are illustrated through
examples in Web Table I. Learning EBM needs a steep
learning curve and a methodical approach. Several authors suggest
introducing EBM to undergraduates when time constraints are less. These
skills can subsequently be strengthened through actual practice during
residency training.
7. Use information technology to optimize
learning and healthcare delivery
Information technology is now vital to the practice
of medicine. The availability of the internet, the adoption of hospital
information systems and electronic health records (EHR) and use of
technology such as tablets and smartphones to provide access to
information at the point of care have changed the way in which clinical
medicine is practiced [31]. Medical colleges also have invested majorly
in computers and internet access.
Acceptance of technology is affected by perceived
ease of use and perceived usefulness. Of these, the perceived ease of
use has a greater impact on behavior and early learners must overcome
this hurdle to adopt technology [32,33]. While training new learners it
is important to keep in mind the following factors which determine early
perceptions of ease of use of a new system [34]:
• Internal control: Characterized by one’s
own sense of savviness with technology.
• External control: Perception of support
from facilitators with use of the new technology.
• Intrinsic motivation: Characterized by
‘computer playfulness’ or intrinsic enjoyment in interacting with
the technology.
• Emotion: Computer anxiety or negative
reaction to use of computers.
8. Participate in the education of patients,
families, fellow students and other healthcare professionals
Patient-education requires several skills and
capabilities such as: knowledge about the disease process, counseling
skills, and interpersonal and communication skills. Learners must be
trained in carrying out interactive, two-way, patient-centered
counseling sessions, while paying special attention to the behavioral,
psychosocial and environmental attributes of health and disease [35,36].
They must be able to perform data gathering, educate the patient,
negotiate and resolve issues, and demonstrate empathy [37].
Strategies to Impart Training in PBLI
Teaching the competency of PBLI may require different
pedagogical strategies compared to those used to foster
clinical-reasoning skills or patient-interaction skills. The basic
principles of designing these strategies are to clearly define key
learning outcomes, identify potential workplace settings which can be
opportunistically used to impart PBLI competencies and select engaging
and learning-rich experiences. The developmental milestones enumerated
in Web Table I will be useful to identify the level of the
learner and build on previous learning.
Learners must be encouraged to use both formal and
informal approaches. Some of these approaches are: use of study groups
with peers, problem solving exercises, formal clinical rotations, online
modules (for knowledge); demonstrations, simulations, review of video
recording of learner, deliberate practice (for skills); and sharing real
life experiences in discussions, behavioral interventions, and
appropriate role models (for behavior). Deliberate practice involves
improving and extending the reach and range of skills which one already
possesses. Deliberate practice entails consider-able, specific and
sustained efforts to develop expertise in something which the learner
cannot do well [38].
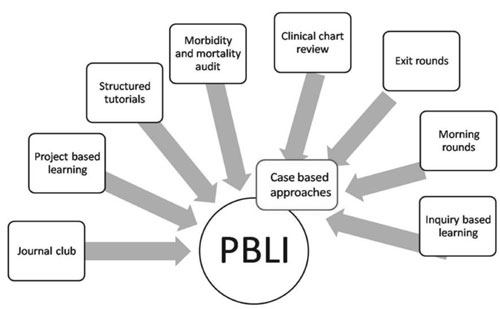
Literature has documented many teaching-learning
strategies ranging from small-group learning [39], workshops [40] to
project-based learning [41], which can help in fostering these behaviors
in learners. Many curricula and models have also been developed and
tested [42-44]. Some of the best documented instructional strategies for
cultivating PBLI behaviors in learners have been documented in the ACGME
project report [45] and are summarized in Fig.2. Some of
these instructional strategies are elaborated below:
 |
|
Fig.2 Teaching-learning strategies to
cultivate practice-based learning and improvement behaviors in
learners.
|
Case-based approaches
A case, problem or inquiry is used to stimulate
discussion and impart learning. Based upon the level and nature of
inquiry, residents’ discussion can be observed, analyzed, evaluated and
critiqued as it reflects their level of knowledge, skills, and
attitudes. Probing can divulge the existing status of knowledge as well
as resident’s ability to recognize learning gaps. Some of the case based
approaches are:
• Inquiry-based learning: This model helps
learners develop the habit of inquiry by asking questions. These
questions may be posed to themselves or to other learners in the
group, thus fostering self-directed and autonomous learning.
Learners not only try to search for the right answers, but also
identify the gaps in their learning as far as knowledge and skills
are concerned and help to address them. This can be in the form of
reciprocal peer questioning. The model works on the presumption that
if critical thinkers are good questioners, the reverse is also true.
This helps in promoting skills of critical analysis and appraisal
[46].
• Morning rounds: Cases providing learning
opportunities can be chosen and patient-care can be reviewed during
rounds, with residents and students being asked to prepare possible
queries about the case. To widen the areas of learning opportunities
and improving the patient-care, case audits and case-census can also
be assimilated into the whole exercise [47].
• Exit rounds: Exit rounds tap the
opportunity of learning provided by recently discharged patients.
Residents reflect on the learning they have while working with these
patients. This provides with an opportunity to improve their patient
care practices too. Besides being a learning exercise, exit rounds
offer attending physicians an opportunity to evaluate students’
learning and performances [48].
• Clinical-chart review: A chart review
involves a systematic analysis of what has been done in the course
of clinical care of a patient, and how this could have been done
better. Patient chart review can help residents in identifying the
areas where they need improvement; gaps in their patient care
practice, and help them in taking critical action to improve their
patient outcomes. This exercise improves self-assessment and
critical analytical skills [43].
Morbidity and mortality audit
A morbidity and mortality audit is a specific audit
that tends to review negative clinical outcomes. A bizarre audit finding
can act as a lead and can direct further investigation into practice
patterns [49]. The resident scrutinizes an morbidity and mortality case
in terms of his or her own practice behaviors, reflects on it, and uses
that to improve practice behavior [43,50]. The resident presents a
description of the case, reflections on what went wrong, and a list of
resources used to gain a better understanding of the case. Presenters
are expected to challenge themselves with self-queries like what they
would do differently and what they would have to learn in order to
improve. Clinical teachers rate residents in areas of practice analysis,
improvement opportunity, resources to support analysis, and action plan
[50].
Structured-tutorials
A case under a resident’s care, which generated
uncertainty either during evaluation or management or counseling and
which definitely requires some action is chosen. The resident discusses
the case with a facilitator. Then a Medline search is conducted by the
resident for relevant literature review. Again a meeting with
facilitator is conducted and a tutorial is prepared. The same is
presented to the group in a structured-manner, giving questioning
opportunities after every session [51]. By utilizing their own clinical
cases, the residents appreciate the need to learn, identify
learning-gaps, and improve by self-reflection on real life situations,
thus improving PBLI skills.
Project-based learning
Residents work with a facilitator to recognize an
area of their practice that needs improvement, plan a
project-intervention to improve upon that gap, execute the improvement,
and establish its efficacy of the implementation during next year. By
learning their own practice-gaps and improving upon by self-reflection,
and implementation of improvement-project, the residents inculcate PBLI
skills [52].
Journal clubs
The focus of journal clubs can be one specific skill
(such as how to use likelihood ratios, or how a search strategy is
developed), and then specific articles can be chosen to teach that
particular skill. Residents must eventually learn how to weigh the
strength of the scientific evidence and regular sessions on critical
appraisal of journal articles are most valuable for this purpose.
While PBLI needs to be explicitly included in the
postgraduate training program, it can be introduced early in the
undergraduate curriculum with Early clinical exposure (ECE); using
student electives to reinforce the value of evidence-based medicine; and
by allowing undergraduates to shadow patients in the clinics.
Assessment of PBLI Competencies
Assessment of PBLI as a whole is difficult as it
spans different roles of a scholar, professional, manager, communicator,
and lifelong learner. It is not possible to measure all competencies
with a single assessment tool. Lack of validated and reliable tools to
assess this competency compounds the problem. Dependable methods of
assessment must be developed. By defining milestones for each
competency, assessment criteria specify the level of achievement or
mastery expected at each stage. During assessment, the rate of progress
of the learner’s knowledge, skills and behavior on each competency must
be documented.
Assessment of PBLI involves longitudinal observation
of the learner demonstrating self-directed learning behaviors, during
multiple encounters [17]. One option to demonstrate improvement is to
use the same assessment tool at different points along the training,
provided that the tool is able to consistently distinguish between the
different levels of performance.
It is important to clarify what will be assessed, how
and when the assessment will be conducted and who will be responsible
for assessment. Assessment can both be formative as well as summative.
Some of the approaches which have been used to assess PBLI are detailed
below:
Portfolios: Residents in most institutes in
India, use pre-formatted logbooks as a popular means to document
learning experiences in patient care. These are seldom taken seriously
and scarcely provide opportunities of reflective behavior, feedback and
improvement in patient care. Portfolios are a compilation of one’s
professional work and achievements over a period of time and can be used
to assess progress. Self-reflection is the inherent characteristic of
any portfolio-linked learning and professional development, and that’s
where they differ from logbooks, which are merely a compilation of
record of one’s work [53]. Reviewing and analyzing a portfolio along
with a mentor is a good strategy for a resident to receive formative
feedback [54]. Portfolios can also be maintained electronically to track
learner progress. The flexibility, comprehensiveness and potential for
integration offered by use of portfolios makes it a top choice for
assessment of PBLI competencies [9].
Medical record review and Chart-stimulated recall:
Patient records are reviewed during one-on-one sessions with faculty in
formal or informal settings using standardized forms. The focus of the
review can be resident’s decision making, medications given, tests
ordered, impact of interventions and their comparisons with standard
patient care guidelines.
Performance ratings using checklists or global rating
forms: Global assessment of competencies using rubrics or
observation checklists may be other methods of demonstrating progress of
learners [2,13]. Rubrics must clearly show how the learner has moved to
a higher level of performance on each competency. Checklists are useful
when competencies can be broken down into specific behaviors or actions.
Each clinical encounter requires enlisting of determined standards
before assessment can be implemented. Both checklists and rubrics
require trained raters to assess completeness and correctness of each
outcome.
Procedure or case logs: Residents prepare
summaries of patient care experiences or procedures, which include both
clinical data as well as their reflections [2]. These logs are useful
for documentation of experiences and deficiencies, and can form part of
the portfolio. Review of these logs with a faculty can be used to assess
PBLI competencies.
Evidence-based medicine skill test: Some
residency programs use written or oral EBM skill tests to assess
knowledge of critical appraisal. Different abilities–such as formulating
well-structured clinical questions; performing advanced literature
searches; and assessing validity of evidence in published studies can be
tested. The EBM skill test can be conducted several times; once before
exposure to EBM curriculum and after that to record improvement in
learning. Sustainability of improved behavior can be also assessed with
EBM skill tests [55].
Other methods: Multiple choice questions,
oral examination, use of standardized patients, objective structured
clinical examination, work-place based assessment [56] like
mini-clinical evaluation exercise (mini-CEX), 360° assessment and direct
observation of procedural skills (DOPS), can be used for formative and
summative assessment of PBLI. During 360° assessment or multisource
feedback, residents receive structured feedback using standard forms
from their peers, faculty, nurses, other staff and patients who observe
their work on a day-to-day basis during patient care. Feedback maybe
gathered on different aspects of their performance such as team work,
professionalism, communication skills, management skills or decision
making. These assessment forms could form part of the educational
portfolio. In all these methods, direct observation of the learner in
the workplace is followed by opportunities for reflection when
constructive feedback is given by the faculty.
Role of Faculty and Faculty Development
While we cannot emphasize the role of faculty in
nurturing these skills enough, it must be said that strong institutional
leadership and support are the keys to the effective implementation of
these competencies. A rigid regulatory framework, shortage of faculty,
unenthusiastic or overworked faculty, or lack of resources are all
possible impediments to the successful functioning of this programme.
Faculty is required to guide and nurture learners to
be self-directed [57]. Faculty or supervisors will be required to assist
learners in envisioning long-term broader goals and then breaking them
down into more achievable feasible short-term goals within a given time
frame. It is important for faculty in each department to diagnose the
stage of self-directedness that the learner lies in, so that they can
facilitate their movement from a less advanced to a more advanced stage
[58].
Faculty must be made aware of the importance of
ensuring that students are trained and assessed for the competencies
under PBLI. Faculty sensitization and training will be required to
identify opportunities within the existing curriculum to incorporate
PBLI training, provide constructive formative feedback, documentation of
progress of milestones achieved by students in a longitudinal manner and
assessment of competencies of PBLI. Ownership must be shared by several
collaborators.
The development of expertise requires faculty who
have the patience to observe students in their day-to-day work, and who
have the capability of delivering constructive, and sometimes difficult
feedback to the learner. Feedback which comes from a supervisor who has
directly observed the learner is always more acceptable. To provide
optimal feedback, faculty need to articulate it in a simple manner and
provide clear messages, facilitate reflection and guide learners on how
to translate learning goals into action [59]. Faculty must also have the
ability to mentor, support and challenge learners in a manner that they
are driven to achieve the next milestone. For skill acquisition, it is
useful here to remember that there will be variations in how learners
progress and acquire more advanced skills [15]. They must be given
enough guidance, feedback, experience and practice to be comfortable
with newer technologies.
Conclusion
Residents must be provided with ample opportunities
to experience and practice their skills, in order to move towards
acquiring expertise and acquire the competencies under practice based
learning and improvement. It is important that they develop
self-awareness of their abilities, are able to reflect on their
proficiency and find avenues to pursue lifelong learning. Training and
assessment of PBLI skills should be a mandatory part of the postgraduate
curriculum and strategies to foster PBLI skills should be interwoven
within all phases of training. Availability of milestones makes this
process feasible enough to implement in practice.
1. Spencer J. Learning and teaching in the clinical
environment. Br Med J. 2003;326:591-4.
2. Hayden SR, Dufel S, Shih R. Definitions and
competencies for practice-based learning and improvement. Acad Emerg
Med. 2002;9:1242-8.
3. Varkey P, Karlapudi S, Rose S, Nelson R, Warner M.
A systems approach for implementing practice-based learning and
improvement and systems-based practice in graduate medical education.
Acad Med.2009; 84: 335-9.
4. Swing SR. Assessing the ACGME general
competencies: General considerations and assessment methods. Acad Emerg
Med. 2002;9:1278-88.
5. Paukert JL, Chumley-Jones HS, Littlefield JH. Do
peer chart audits improve residents’ performance in providing preventive
care. Acad Med. 2003; 78 (suppl 10):S39-41.
6. Sutherland JE, Hoehns JD, O’Donnell B, Wiblin RT.
Diabetes management quality improvement in a family medicine residency
program. J Am Board Fam Pract. 2001;14:243-51.
7. Parenti CM, Lederle FA, Impola CL, Peterson LR.
Reduction of unnecessary intravenous catheter use: Internal medicine
house staffparticipate in a successful quality improvement project. Arch
Intern Med. 1994;154:1829-32.
8. Medical Council of India. Post Graduate Medical
Education Regulations 2000. Available from:
http://www.mciindia.org/RulesandRegulations/PGMedical
EducationRegulations2000.aspx. Accessed July 17, 2016.
9. Lynch DC, Swing SR, Horowitz SD, Holt K, Messer
JV. Assessing practice-based learning and improvement. Teach Learn Med.
2004; 16: 85-92.
10. Swing SR. The ACGME outcome project:
retrospective and prospective. Med Teacher. 2007;29:648-54.
11. Sullivan RL. The Competency-based Approach to
Training. Strategy Paper No 1. JHPIEGO Corporation: Baltimore, Maryland;
1995. Available from: http://pdf.usaid.gov/pdf_docs/Pnacg569.pdf.
Accessed July 17, 2016.
12. Nasca T. The next step in the outcomes-based
accreditation project. ACGME Bull. 2008;2-4.
13. Swing SR, Beeson MS, Carraccio C, Coburn M, Lobst
W, Selden NR, et al. Educational milestone development in the
first 7 specialties to enter the next accreditation system. J Grad Med
Educ. 2013;5:98-106.
14. Holmboe ES, Edgar L, Hamstra S. ACGME: The
Milestones Guidebook; Version 2016. Available from:
https://www.acgme.org/Portals/0/MilestonesGuidebook. pdf. Accessed
July 17, 2016.
15. Dreyfus HL, Dreyfus SE. Mind over Machine. New
York, NY: Free Press; 1988.
16. Dhaliwal U, Gupta P, Singh T. Entrustable
professional activities: Teaching and assessing clinical competence.
Indian Pediatr. 2015; 52: 591-7.
17. Burke AE, Benson B, Englander R, Carraccio C,
Hicks PJ. Domain of competence: Practice-based learning and improvement.
Acad Pediatr. 2014; 14: S38-S54.
18. Hicks PJ, Schumacher DJ, Benson BJ, Burke AE,
Englander R, Guralnick S, et al. The pediatrics milestones:
conceptual framework, guiding principles, and approach to development. J
Grad Med Educ. 2010; 2:410-8.
19. American Board of Pediatrics and Accreditation
Council for Graduate Medical Education. The Pediatrics Milestone
Project. Available from: https://www.abp. org/abpwebsite/publicat/milestones.pdf.
Accessed July 17, 2016.
20. Englander R, Burke A, Guralnick S, Benson B,
Hicks PJ, Ludwing S, et al. The pediatric milestones: a
continuous quality improvement project is launched-now the hard work
begins! Acad Pediatr. 2012;12:471-4.
21. Hicks PJ, Englander R, Schumacher DJ, Burke A,
Benson BJ, Gurulnick S, et al. Pediatrics milestone project: next
steps toward meaningful outcomes assessment. J Grad Med Educ.
2010;2:577-84.
22. Schumacher DJ, Lewis KO, Burke AE, Smith ML,
Schumacher JB, Pitman MA, et al. The pediatrics milestones:
initial evidence for their use as learning roadmaps for residents. Acad
Pediatr. 2013;13:40-7.
23. Kolb D. Experiential Learning as the Science of
Learning and Development. Englewood Cliffs, NJ: Prentice Hall; 1984.
24. Schon D. Educating the Reűective Practitioner.
San Francisco, Calif: Jossey-Bass Publishers; 1987.
25. Knowles MS. Self-Directed Learning. A Guide for
Learners and Teachers. Englewood Cliffs: Prentice Hall/Cambridge; 1975.
26. Morris C, Blaney D. Work-Based Learning. In:
Swanwick T, (editor). Understanding Medical Education: Evidence, Theory
and Practice. Wiley-Blackwell: Oxford, UK; 2010.
27. Ende J. Feedback in clinical medical education.
JAMA. 1983;250:777-81.
28. Moore LG, Wasson JH. Improving efficiency,
quality and the doctor–patient relationship. Fam Pract Manag.
2007;14:20-4.
29. Ashton CM. "Invisible doctors": making a case for
involving medical residents in hospital quality improvement programs.
Acad Med. 1993;68:823-4.
30. Sackett DL, Rosenberg WM, Gray JA, Haynes RB,
Richardson WS. Evidence based medicine: what it is and what it isn’t.
BMJ. 1996;312:71-2.
31. Duncan J, Evens R. Using information to optimize
medical outcomes. JAMA. 2009;301:2383-5.
32. Davis FD. Perceived usefulness, perceived ease of
use, and user acceptance of information technology. MIS Q.
1989;13:319-39.
33. Davis FD, Bagozzi RP, Warshaw PR. User acceptance
of computer technology: a comparison of two theoretical models. Manage
Sci. 1989;35:982-1002.
34. Venkatesh V. Determinants of perceived ease of
use: integrating control,intrinsic motivation, and emotion into the
technology acceptance model. Inf Syst Res. 2000;11:342-65.
35. Bird J, Cohen-Cole SA. The three function model
of the medical interview. An educational device. Adv Psychosom Med.
1990;20:65-88.
36. Lazare A, Putnam SM, Lipkin M. Jr. Three
functions of the medical interview. In: Lipkin M Jr., Putnam SM,
Lazare A, editors. The Medical Interview: Clinical Care, Education, and
Research. New York, NY: Springer-Verlag; 1995. pp. 3-19.
37. Modi JN, Anshu, Chhatwal J, Gupta P, Singh T.
Teaching and assessing communication skills in medical undergraduate
training. Indian Pediatr. 2016;53: 497-504.
38. Ericsson KA, Prietula MJ, Cokely ET. The making
of an expert. Harv Bus Rev. 2007;85:114-21.
39. Canal DF, Torbeck L, Djuricich AM. Practice-based
learning and improvement: a curriculum in continuous quality improvement
for surgery residents. Arch Surg. 2007;142:479-83.
40. Morrison LJ, Headrick LA. Teaching residents
about practice-based learning and improvement. Jt Comm J Qual Patient
Saf. 2008;34:453-9.
41. Ogrinc G, Headrick LA, Morrison LJ, Foster T.
Teaching and assessing resident competence in practice-based learning
and improvement. J Gen Intern Med. 2004;19 496-500.
42. Peters AS, Kimura J, Ladden JD, March E, Moore
GT. A self-instructional model to teach systems-based practice and
practice-based learning and improvement. J Gen Intern Med.
2008;23:931-6.
43. Ziegelstein RC, Fiebach NH. The mirror and the
village: A new method for teaching practice-based learning and
improvement and systems-based practice. Acad Med. 2004;79:83-8.
44. Tomolo AM, Lawrence RH, Watts B, Augustine S,
Aron DC, Singh MK. Pilot study evaluating a practice-based learning and
improvement curriculum focusing on the development of system-level
quality improvement skills. J Grad Med Educ. 2011;3:49-58.
45. ACGME Outcome Project. Enhancing residency
education through outcomes assessment - Advancing education in
practice-based learning and improvement. Available from:
https://www.usahealthsystem.com/workfiles/com_docs/gme/2011%20Links/Practice%20Based%20Learning.
ACGME.pdf. Accessed July 17, 2016.
46. King A. Designing the instructional process to
enhance critical thinking across the curriculum. Teach Psychol.
1995;22:13-7.
47. Whelan CT, Podrazik PM, Johnson JK. A case based
approach to teaching practice-based learning and improvement on the
wards. Semin Med Pract. 2005; 8: 64-74.
48. Arseneau R. Exit rounds: A reflection exercise.
Acad Med. 1995;70: 684-7.
49. Yaffe MJ, Gupta G, Still S, Boillat M, Russillio
B, Schiff B, et al. Morbidity and mortality audits. Can Fam
Physician. 2005;51:234-9.
50. Rosenfeld JC. Using the morbidity and mortality
conference to teach and assess the ACGME general competencies. Curr
Surg. 2005;62:664-9.
51. Green ML, Ellis PJ. Impact of an evidence-based
medicine curriculum based on adult learning theory. J Gen Intern Med.
1997;12:742-50.
52. Lough JRM, Murray TS. Audit and summative
assessment: a completed audit cycle. Med Educ. 2001;35:357-63.
53. Joshi M, Gupta P, Singh T. Portfolio-based
learning and assessment. Indian Pediatr. 2015;52:231-5.
54. Salzman DH, Franzen DS, Leone KA, Kessler CS.
Assessing practice-based learning and improvement. Acad Emerg Med.
2012;19:1403-10.
55. Smith CA, Ganschow PS, Reilly BM. Teaching
residents evidence-based medicine skills: a controlled trial of
effectiveness and assessment of durability. J Gen Intern Med.
2000;15:710-5.
56. Singh T, Modi JN. Workplace-based assessment: A
step to promote competency based postgraduate training. Indian Pediatr.
2013;50:553-9.
57. Schmidt H. Assumptions underlying self-directed
learning may be false. Med Educ. 2000;34:243-5.
58. Grow GO. Teaching learners to be self-directed.
Adult Educ Q. 1991;41:125-49.
59. Nichol DJ, Macfarlane-Dick D. Formative
assessment and self-regulated learning: a model and seven principles for
good feedback practice. Stud Higher Educ. 2006;31: 199-218.

