|
|
|
Indian Pediatr 2013;50: 399-404 |
 |
Consensus Statement of the Indian Academy of
Pediatrics on Integrated Management of
Severe Acute Malnutrition
|
|
Indian Academy of Pediatrics
Writing Committee: Samir Dalwai, Panna Choudhury,
Sandeep B Bavdekar, Rupal Dalal, Umesh Kapil, AP Dubey, Deepak Ugra,
Manohar Agnani and HPS Sachdev
Correspondence to: Dr Panna Choudhury, D-II/M,
2753, Netaji Nagar, New Delhi 110 023, India. [email protected]
|
|
Justification: Severe acute malnutrition (SAM) is a major public
health issue. It afflicts an estimated 8.1 million under-five children
in India causing nearly 0.6 million deaths. The improved understanding
of pathophysiology of SAM as well as new internationally accepted growth
charts and newer modalities of integrated intervention have necessitated
a relook at IAP recommendations.
Process: A National Consultative
Meeting on Integrated Management of Severe Acute Malnutrition was held
in Mumbai on 16th and 17th October, 2010. It was attended by the invited
experts in the field. Extensive discussions were held as per the
program. The participants were then divided into six groups for detailed
discussions. The groups deliberated on various issues pertaining to the
task assigned and presented recommendations of the groups in a plenary
session. The participants made a list of recommendations after extensive
discussions. A Writing Committee was formed and was entrusted with the
task of drawing a Consensus Statement on the basis of these
Recommendations. After multiple deliberations, the following Consensus
Statement was adopted.
Objectives: To critically
evaluate the current global evidence to formulate a consensus among
stakeholders regarding diagnosis and management of SAM.
Recommendations: An integrated
management of malnutrition is likely to yield more dividends. Thus,
management of SAM should constitute an important component of Integrated
Management of Neonatal and Childhood Illnesses (IMNCI) program.
Determination of SAM on the basis of Z-scores using WHO Growth
charts is considered statistically more appropriate than cut-offs based
on percentage weight deficit of the median. Considering the fact that
many children with SAM can be successfully managed on outpatient basis
and even in the community, it is no more considered necessary to advise
admission of all children with SAM to a healthcare facility. Management
of SAM should not be a stand-alone program. It should integrate with
community management therapeutic programs and linkages with child
treatment center, district hospitals and tertiary level centers offering
inpatient management for SAM and include judicious use of
ready-to-use-therapeutic Food (RUTF). All sections of healthcare
providers need to be trained in the integrated management of SAM.
Key words: Child, Malnutrition, Management,
Ready-to-Use-Therapeutic Food.
|
|
Mission of the Indian Academy of Pediatrics (IAP)
IAP is in cognizance of the acute necessity of
undertaking immediate remedial measures for an estimated 8 million
children below 5 years of age who are suffering from Severe acute
malnutrition (SAM). IAP is committed to provide academic as well as
programmatic support to a concerted national effort in this direction.
It commits the service of over 300 branches and 18,000 pediatricians for
a systematic and structured effort to address this issue.
Introduction
Severe acute malnutrition is a major public health
issue. It afflicts an estimated 8.1 million under-five children in India
[1]. Nearly 0.6 million deaths and 24.6 million DALYs (disability
adjusted life years) are attributed to this condition. Diarrhea and
pneumonia account for approximately half the under-five deaths in India,
and malnutrition is believed to contribute to 61% of diarrheal deaths
and 53% pneumonia deaths (2). Thus, strong scientific evidence exists on
synergism between under nutrition and child mortality due to common
childhood morbidities including diarrhea, acute respiratory infections,
malaria and measles. In SAM, the case fatality rates related to these
morbidities are excessively high.
The understanding of pathophysiology of SAM
(including edematous malnutrition) has improved. New internationally
accepted growth charts have become available, in which data from Indian
children has also been included. Determination of SAM on the basis of
Z-scores using WHO Growth charts is considered statistically more
appropriate than cut-offs based on percentage weight-deficit of the
median. Dietary interventions using WHO F-75 and F-100 formulae (or
analogues) in the management of inpatient care of SAM have improved
outcomes including reduced mortality, early recovery and higher weight
gain. It is possible to implement this intervention in hospitals and
healthcare facilities. Community-based programs have shown success in
the management of SAM in emergency and non-emergency situations.
Considering the fact that many children with SAM can be successfully
managed on outpatient basis and even in the community, it is no more
considered necessary to advise admission of all children with SAM in a
healthcare facility. This becomes pertinent in view of the economic and
social burden that hospitalization entails on families that are already
battling poverty. Further, our country does not have sufficient hospital
beds for offering inpatient care to all children with SAM. An integrated
management of malnutrition is likely to yield more dividends. Thus
management of SAM should constitute an important component of Integrated
Management of Neonatal and Childhood Illnesses (IMNCI) Program.
Management of SAM should not be a stand alone program. It should
integrate with community management therapeutic programs, and linkages
with child treatment center, district hospitals and tertiary level
centers offering inpatient management for SAM.
Process
A National Consultative Meeting on Integrated
Management of Severe Acute Malnutrition was held in Mumbai on 16th and
17th October, 2010. It was attended by invited experts in the field (Appendix
1). The participants made a list of recommendations
after extensive discussions. A Writing Committee was formed and was
entrusted with the task of drawing a Consensus Statement on the basis of
these recommendations.
Diagnosis of SAM
In children between the ages of 6 and 59 months,
Severe acute malnutrition (SAM) is defined as:
(i) Weight/height or Weight/length < -3
Z score, using the WHO Growth Charts; OR
(ii) Presence of visible severe wasting;
OR
(iii) Presence of bipedal edema of
nutritional origin; OR
(iv) mid- upper arm circumference (MUAC) <
115 mm.
For infants below 6 months, Criteria (i) or (ii)
or (iii) above should be used till data on MUAC below 6 months
becomes available. IAP guidelines of 2006 have stated MUAC <110 mm as
one of the criterion. Research in India is required to arrive at
critical MUAC that will screen and produce similar results when we use
weight for height <-3 Z score, using WHO new growth charts, as the
criterion. As infants and children from India were also included while
formulating WHO growth charts, a MUAC below 115 mm, as being used for
other countries, should be adopted till we have more Indian data.
Active Detection of Children with SAM
Early detection of children with SAM will ensure that
these children will be identified before they develop medical
complications. This would mean management of many of them before their
prognosis worsens and it would also reduce the need for hospitalized
care [4,5]. Health professionals and healthcare providers should detect
children with SAM at every opportunity provided by health contacts, be
it for a medical complaint or for health promotional measures (e.g.
growth monitoring or immunization). This can be undertaken at every
health facility (primary health center and sub-center, health posts,
hospitals, day-care centers, etc) and even in the community and
anganwadis by healthcare workers.
MUAC is a simple measure for the detection of SAM.
Screening of children in the community for SAM can be done using MUAC
tape. Good quality, non-stretchable, long lasting MUAC tapes should be
available at every healthcare facility.
Appetite Test
Appetite test is an important criterion to
differentiate a complicated from an uncomplicated case of SAM and
therefore decide if a patient should be sent for in-patient or
out-patient management. Children with SAM who have poor appetite are at
immediate risk of death and they will not take sufficient amounts of the
diet at home to prevent deterioration and death.
TABLE I: Criteria for Passing Appetite Test
|
Body weight |
Minimum amount of RUTF |
|
(kg) |
to be consumed for passing |
|
the Appetite Test (mL or grams) |
|
>4
|
15 |
|
4 6.9 |
25 |
|
7 9.9 |
35 |
|
10 14.9 |
50 |
This test has not been standardized or published in
diverse Indian settings with different types of therapeutic foods. In
the African settings, it is usually conducted in a quiet area with ready
to use therapeutic food (RUTF). In African setting, a child, not
consuming the minimum recommended amount of RUTF (Table I),
is labeled as failed Appetite Test and is referred for in-patient
care. It may be possible to extrapolate these guidelines to the
therapeutic food being used in the Indian setting.
The appetite test should be carried out at each
visit for patients not hospitalized, particularly those who do not
gain weight steadily.
Failure of an appetite test at any time is an
indication for full evaluation and probable transfer for in-patient
assessment and treatment.
If the appetite is "good" during the appetite
test and the rate of weight gain at home is poor then a home visit
would be required because this may indicate a social problem at
household level or extensive sharing of the medical nutrition
therapy. A simple "trial of feeding" at residential care may be
needed to differentiate a difficulty with the home environment from
a metabolic problem with the patient
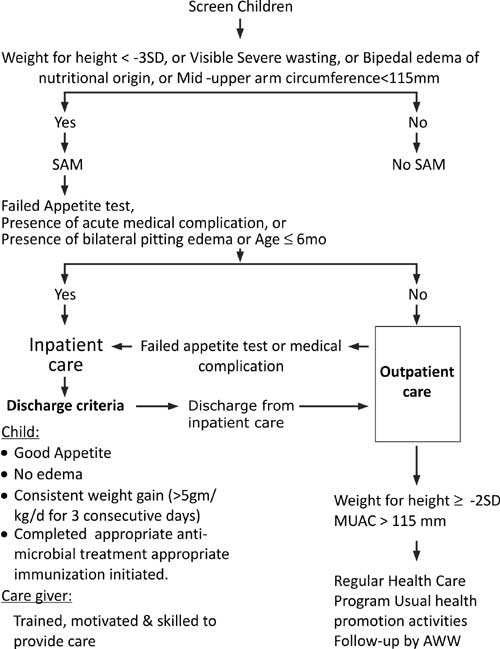
Triage for Inpatient Care
Triage is undertaken in the community or in any
facility that the child is brought initially to find out if children
identified to have SAM need facility care like child treatment center or
district or tertiary hospital. Indications for inpatient care include
the following: (i) Presence of a medical complication; (ii)
Reduced appetite (as judged on the basis of a failed appetite test); (iii)
Presence of bilateral pitting edema; and (iv) Age
≤ 6 months.
A detailed identification and management plan for
children with SAM is provided in Fig. 1.
 |
|
(Adapted from WHO Growth Standards and identification of Severe
Acute Malnutrition in infants and children. A joint statement of
WHO and UNICEF. 2009) [3].
Fig. 1 Identification and management
of children with severe acute malnutrition (SAM).
|
Outpatient Care
Children with SAM who do not have any criterion for
inpatient care can be managed under an outpatient therapeutic program
(OTP) center closest to the childs home. There is a need to establish
such a program as a part of Integrated Child Development Scheme (ICDS)/
RCH-II/ IMNCI-ANM, NRHM-ASHA.
TABLE II: Amount of Therapeutic Food to be Consumed
|
Weight |
Amount of RUTF per day |
|
3 4.9kg |
105 130 g/day |
|
5 6.9kg |
200 260 g/day |
|
7 9.9kg |
260 400 g/day |
|
10 14.9kg |
400 460 g/day |
|
RUTF: ready to use therapeutic food |
There is a need to provide "therapeutic food"
broadly adhering to the WHO and UNICEF specifications; this Medical
Nutrition Therapy [6] is based on sound scientific principles with a
balanced composition of type 1 and type 2 nutrients for consumption
by children suffering with SAM who are being managed in the
community or at home [7]. One form of "therapeutic food" is ready to
use therapeutic food (RUTF), which is a high-energy food, available
in a ready-to-use form with long shelf-life and requiring no
preparation at the point of use. This specific composition has been
tested and proved effective in functional recovery of SAM children,
primarily in the African settings [8]. Controlled trials and
experience with RUTF in India is limited and further, there is no
robust comparative data documenting the benefits of this formulation
over locally produced analogous medical nutrition therapy or
augmented home food.
A rough guide about the amount of therapeutic
food to be consumed is summarized in Table II
below. Breast feeding should be continued while the child is on
therapeutic food. Other foods may be given if child has good
appetite and has no diarrhea.
The amount is to be given in 2-3 hourly feeds
along with plenty of water.
There is a need to generate Indian data in this
regard so that an effective and safe therapeutic food that is
acceptable to children and meets WHO/UNICEF specification can be
made available under the program. It must be emphasized to the
families and to the society at large, that the therapeutic food is
to be used only in children with SAM as a part of therapy. It is not
meant to be a supplementary food for other children or a part of
regular diet. In order to ensure that the same is readily available
and can reach the target population, appropriate notification(s) for
use of such therapeutic food and for its procurement through
institutional mechanisms and its distribution through appropriate
channels e.g. nutrition rehabilitations centers, Anganwadis, etc.
would be ideal and desirable. To ensure that it is not misused, the
Government may consider implementing appropriate restrictions such
as restricting its availability only under the program for children
with SAM and prohibiting its widespread availability.
Outpatient management is not recommended for
children aged six months or less with SAM.
The caretaker/ mother should also be counseled
about breast feeding, supplementary care hygiene, optimal food
intake, immunization and other appropriate health promotional
activities.
Outcome of treatment can be defined as follows:
(a) Non-responder/ Primary Failure (i)
Failure to gain any weight for 21 days, or (ii) Weight loss since
admission to program for 14 days.
(b) Secondary Failure or Relapse (i)
Failure of Appetite test at any visit or (ii) Weight loss of 5% body
weight at any visit. Non-responders and children who develop a
danger sign at any time during first 4 weeks should be referred to a
hospital.
(c) Defaulters: Not traceable for at least 2
visits.
Children can be discharged from the program if
any of the following criteria are satisfied: (a)
Children admitted to SAM program on the basis of weight for height
criteria should be discharged from the program (end therapeutic
feeding) when weight for height becomes greater than or equal to -2
Z score of WHO reference and there is no edema. (b)
Children admitted on the basis of MUAC criteria or presence of
bilateral edema should be discharged (end therapeutic feeding) when
MUAC becomes greater than or equal to 125 mm and there is no edema.
Thereafter, the child can be referred for usual
health care program and growth promotion activities can be ensured by
anganwadi workers (AWW), health care workers and health care
providers.
Inpatient Care
The principles of management are as outlined in the
earlier IAP recommendation (9). The following measures should be
undertaken for children requiring inpatient care:
Ψ
Admission in a warm area separate from other children with infection
Ψ
Prevent, look for and manage: Hypoglycemia,
Hypothermia, Dehydration, Electrolyte disturbances, Infection and
sepsis, Micronutrient-Deficiency; using IAP Guidelines 2006 (9).
A. Children above 6 months of age
Early initiation of appropriate feeding is an
important step in the management of SAM. Therapeutic feeding
conforming to F-75 composition can be used as an initial starting
formula in the acute phase, followed by F-100 composition in the
rehabilitation phase.
B. Infants less than 6 months
Prospect of continuing or re-initiating
breastfeeding: Breastfeeding should be encouraged in children
(aged less than 6 months) and having SAM. Supplemental suckling
technique can be used to support and enhance breastfeeding. These
children should be monitored by determining weight gain and amount
of supplemental feeding taken. The supplemental feeding can be
slowly withdrawn as the breast milk output increases and baby shows
weight gain. A baby showing consistent weight gain on exclusive
breastfeeding can be discharged from the inpatient facility. The
babys growth can then be monitored on outpatient basis.
No prospect of continuing or re-initiating
breastfeeding: These babies should be treated with F-75
composition therapeutic food in the acute phase and response
monitored in a manner described above.
It is necessary to monitor the child and check
for failure to respond to therapy. Failure to respond to therapy
should prompt a review of the case, assessment of actual intake and
checking for untreated infection and psychological problems.
Continuation of breastfeeding should be
encouraged.
Sensory stimulation in the form of tender
loving care, cheerful stimulating environment, structured play
therapy, initiation of physical activity as soon as the child is
well and maternal involvement in comforting, feeding and play are
important aspects of overall management.
Supplementary Suckling Technique
The supplementation is given using tube
feedings: the same size as 8NGT (5NGT can be used and is better for
the infant, but the milk should be strained to remove any small
particles that block the tube. The appropriate amount of
supplemental suckling milk is put in a cup. The mother or assistant
holds it.
The end of the tube is put in the cup.
The tip of the tube is put on the breast at the
nipple and the infant is offered the breast in the normal way so
that the infant attaches properly.
At first, cup should be placed about 5 cm to 10
cm below the level of the nipples so the SS-milk can be taken with
little effort by a weak infant. It must NEVER be placed above the
level of nipple, or else it will flow quickly into the infants
mouth by siphon with a major risk of inhalation. As the infant
becomes stronger the cup should be lowered progressively to about 30
cm below the breast. It may take a day or two for the infants to get
used to the tube and the taste of the mixture of milks, but it is
important to persevere.
Children with SAM above 6 months of age can be
discharged from the health facility once the child and the caretaker
satisfy all the following criteria.
Discharge
Discharge should be done when the child has:
a good appetite (eating at least 120-130
Cal/kg/d) along with micronutrients;
lost edema;
shown consistent weight (>5g/kg/d) on three
consecutive days;
completed anti-microbial treatment; and
appropriate immunization has been initiated,
Mother or Care-taker:
Has been trained to prepare and provide
appropriate feeding
Has financial resources to feed the child
Has been motivated to follow the advice given
Children with SAM below 6 months of age can be
discharged from the health facility once the baby shows consistent
weight gain on oral feeds and has no medical complications. Babies on
breast feeding should be showing this weight gain based on exclusive
breast feeding.
Training and involvement of the mother/ caretaker is
an important aspect of inpatient care. After discharge the child should
be referred for further care to the appropriate OTP center and continue
the integrated management.
Organizational Issues
Inpatient and outpatient treatment should be
one Integrated Program.
The program should be integrated with other
existing health programs intended to provide health promotion
activities
After the initial feasibility testing, the
program may be initiated in a few high-risk districts of the
country. After assessing the effectiveness of the programmatic
interventions, the program can be scaled up to involve all the
districts in the country in a phase-wise manner
The effectiveness of the overall program needs
to be monitored in terms of number of beneficiaries and, improvement
in mortality, among others
The various segments of the program (facility
based inpatient care and outpatient care/ community-level
management) need to be linked; so that children can be followedup
and continued care is assured. This would also help in monitoring
and judging effectiveness of the program
It is necessary to encourage indigenous
commercial production of "therapeutic foods" with strict quality
control.
Training
All sections of the healthcare providers need
to be trained in the Integrated management of SAM
Pediatricians should be motivated and trained
for taking a leadership role at national/state/district level as
this is a child rights issue
Health professionals and medical teachers
should be enrolled as trainers for the program after holding
structured training workshops
Assessment of the effectiveness of training
should be an essential component of the training program
The Universities should be encouraged to accord
a prominent position to the detection and Integrated Management of
SAM in the pediatric curriculum.
Research Priorities
Research priorities should address gaps in
knowledge related to SAM.
Programmatic Research for assessing the
cost-effectiveness of various interventions used in the program
Public and Media Participation
The presence of children with SAM is a reality. The
program to tackle SAM can only be successful through media participation
and creation of public awareness.
Role of Indian Academy of Pediatrics
IAP can play an important role in:
Providing technical advice to the government
regarding appropriate interventions and in formulating management
guidelines and training modules
Assisting the program through conduct of
training programs
Creating public awareness and ensuring media
participation
Recommend the Medical Council of India and the
Universities to include management of SAM in the medical curriculum
for the subjects of Pediatrics and Preventive and Social Medicine
Funding: UNICEF; Competing interests: None
stated.
Appendix 1:
A. List of Participants: Simin F
Irani, Mumbai; Michel Golden, Ireland; Pramila Menon, Pune; Phadke
Mrudula, Mumbai; Rupal Dalal, Mumbai; KG Menon, Pune; Tanmay Amladi,
Mumbai; Manohar Agnani, Bhopal; Reshma Patel, Bhopal; Sandeep B Bavdekar,
Mumbai; Victor Aguayo, Delhi; Manoj Rathi, Amravati; MKC Nair, Amravati;
S Narayan, Delhi; S S Bhambal, Bhopal; Anuradha Bose, Vellore; K S
Multani, Bangalore; M L Agnihotri, Now-Gong; M V Mangalni, Mumbai;
Girish Agarwal, Bareilly; Vasant Khaltakar, Nagpur; Major K Naganath,
Chennai; Arun Bansal, Chandigarh; Evilet Sequeira, UNICEF; Alka Jadhav,
Mumbai; Shaila Aiyer, Vadodara; A Fernandez, Mumbai; A P Dubey, New
Delhi; Panna Choudhury, New Delhi; Sameer H Dalwai, Mumbai; Dhanesh
Volvoikar, Goa; Jayendra Parulekar, Sawantwadi; K V Radhakrishna,
Hyderabad; Bharati Kulkarni, Hyderabad; RK Gupta, Jaipur; Omkar
Khandelwal, Raipur; Deepak Ugra, Mumbai; Tarun Patni, Jaipur and Sandhya
Khadase, Mumbai.
B. List of Participants who could not
attend but participated in finalization of the Recommendations:
Rohit Agarwal, Mumbai; C P Bansal, Gwalior; HPS Sachdev, New Delhi; Uday
Bodhankar, Nagpur; Shashi Vani, Nagpur; Umesh Kapil, New Delhi; and
Sailesh Gupta, Mumbai.
Acknowledgments: Office Bearers and Staff Members
at Central Office, Indian Academy of Pediatrics, Mumbai, for Logistical
Support; and Staff Members, New Horizons Child Development Centre,
Mumbai, for Graphics and Presentation Support.
References
1. International Institute for Population Sciences.
National Family Health Survey 3, 2005-2006. Mumbai India: International
Institute of Population Science; 2006
2. Black RE, Allen LH, Bhutta ZA, de Onis M, Ezzati
M, Mathers C, et al. Maternal and Child undernutrition: global
and regional exposures and health consequences. Lancet. 2008; 371:
243-60.
3. WHO Child Growth Standards and the Identification
of Severe Acute Malnutrition in Infants and Children. A joint statement
by WHO and UNICEF, 2009. Accessed from
http://www.who.int/nutrition/publications/severemalnutrition/9789241598163_eng.pdf
4. Collins S. Treating severe acute malnutrition
seriously. Arch Dis Child. 2007; 92: 453-61.
5. Linneman Z, Matilsky D, Ndekha M, Maleta K, Manary
MJ. A large-scale operational study of home based therapy with
ready-to-use therapeutic food in childhood malnutrition in Malawi.
Maternal Child Nutr. 2007; 3: 206-15.
6. Sachdev HPS, Kapil U, Vir S. Consensus Statement:
National Consensus Workshop on Management of SAM Children through
Medical Nutrition Therapy. Indian Pediatr. 2010; 47: 661-65.
7. Community-based Management of Severe Acute
Malnutrition. A Joint Statement by the World Health Organization, the
World Food Programme, the United Nations. System Standing Committee on
Nutrition and the United Nations Children Fund, Geneva: UNICEF; 2007.
8. Briend A, Lacsala R, Prodhon C, Mounier B,
Grellety Y, Golden MH. Ready to use therapeutic food for treatment of
marasmus. Lancet 1999; 353:1767-1768.
9. Bhatnagar S, Lodha R, Choudhury P, Sachdev
HPS, Shah N, Narayan S, et al. IAP Guidelines 2006 on
hospital based management of severely malnourished children. Indian
Pediatr. 2007; 44: 443-61.
|
|
|
 |
|

