|
Left
ventricular noncompaction (LVNC) is a reportedly
rare disorder of endomyocardial morphogenesis
[1]. The prevalence of LVNC among patients
referred to echocardiography laboratories is
reported to be between 0.014 and 1.3% [2,3] and
accounts for 9.5% of all primary
cardiomyopathies [4]. It is commonly
misdiagnosed as hypertrophic or dilated
cardiomyopathy. There is only one case report of
LVNC in children from India [5].
Case Report
A 3-months-old boy presented
with feeding difficulty and sweating over
forehead since 15 days and breathlessness since
2 days. His parents were unrelated and he was
their first child. On examination, he had
congestive heart failure (heart rate -100 /min,
weak pulses, capillary refill time of 5 seconds,
S3 gallop, grade 3/6 pansystolic murmur at apex,
hepatomegaly, tachypnea and bilateral basal
crepitations). Other systemic examination was
normal. He had no dysmorphic features.
The X-ray chest showed
cardiomegaly. The ECG revealed left ventricular
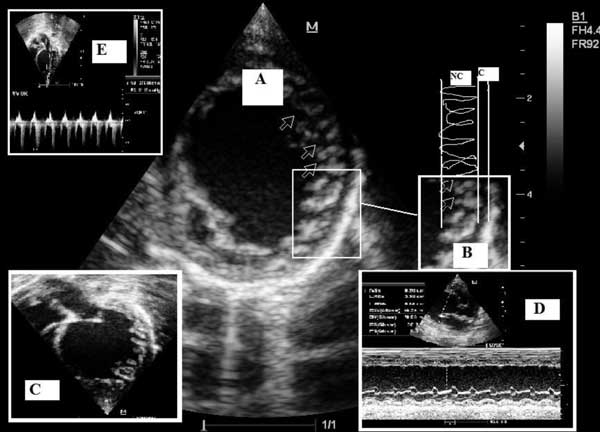
hypertrophy. The echocardiography demonstrated
grossly enlarged left ventricle. A two layer
structure was seen, with a compacted thin
epicardial band and a thick noncompacted
endocardial layer with coarse trabeculations
having deep intertrabecular recesses at the
apical and lateral wall segments of the left
ventricle (Fig. 1). The end
systolic ratio of noncompacted to compacted
layers was 3.2. The color Doppler imaging showed
blood filling the recesses from the ventricular
cavity. The origin of both the coronary arteries
was normal. The M-mode showed left ventricular
end- diastolic diameter (LVEDD) – 3.72 cm (Z
score = 7.52), left ventricular end- systolic
diameter (LVESD) – 3.39 cm (Z score = 12.12),
the left ventricle ejection fraction (LVEF)
-30.2% and shortening fraction (SF) -9%. There
was mitral regurgitation with velocity of 279
cm/s. The right ventricle was normal. These
findings were consistent with isolated left
ventricular noncompaction.
 |
|
Fig.1 (A)
Parasternal short axis view. The end-
systolic still frame shows the two
layered structure with thin epicardial
layer and an extremely thickened
endocardial layer with prominent
trabeculations and deep recesses
(arrows). (B) To quantify the thickness
of the noncompacted layer at the site of
maximum thickness, the end- systolic
ratio of the noncompacted (NC) to
compacted (C) layer is determined. (C)
Apical four- chamber view still frame.
(D) M-Mode study demonstrating LVEF-
30%. (E) mitral valve Doppler
demonstrating regurgitation.
|
He was treated with
decongestive therapy and inotropes for 3 days,
and subsequently discharged on oral enalapril,
frusemide and ecosprin. The echocardiography of
parents was normal.
Discussion
Left ventricular
non-compaction represents an arrest in
endomyocardial morphogenesis, which normally
occurs between 5- 8 weeks of fetal life and is
characterised by gradual compaction of
myocardium, transformation of large
intertrabecular spaces into capillaries, and
evolution of the coronary circulation [1].
Clinically, patients may be asymptomatic or
present with CHF, arrhythmia and embolic events
[4-6]. The presenting symptoms include tachypnea,
cyanosis, syncope, or failure to thrive, Chin,
et al. [7] have described facial
dysmorphism, including a prominent forehead, low
set ears, strabismus, high- arched palate and
micrognathia.
LVNC can be diagnosed by
two-dimensional echocardiography and color
Doppler [7,8]. The criterion for diagnosis is
ratio of noncompacted to compacted layer of >2
measured at end systole.
There is no specific therapy.
The mainstay of treatment is diuretics, ACE
inhibitors and beta- blockers (Carvedilol) to
improve the left ventricular systolic function.
Anticoagulation (target INR – 2.0-3.0) is
recommended when LVEF <40% [3]. Pignatelli,
et al.[4] recommend oral aspirin and a
metabolic cocktail including thiamine, coenzyme
Q10, riboflavin and carnitine. Poor prognostic
markers predicting death or heart transplant are
age at onset, NYHA functional class III–IV,
sustained ventricular arrhythmias, ratio of
noncompacted to compacted layers, number of
affected segments, LVEDD and abnormal lateral
mitral tissue Doppler Ea velocity [3,9].
Funding: None;
Competing interests: None declared.
References
1. Elshershari H, Okutan V,
Celiker A. Isolated noncompaction of the
ventricular myocardium. Cardiol Young.
2001;11:472-5.
2. Oechslin EN, Attenhofer
Jost CH, Rojas JR, Kaufmann PA, Jenni R. Long-
term follow-up of 34 adults with isolated left
ventricular noncompaction: a distinct
cardiomyopathy with poor prognosis. J Am Coll
Cardiol. 2000;36:493-500.
3. Oechslin E, Jenni R. Left
ventricular non-compaction revisited: a distinct
phenotype with genetic heterogeneity? Eur Heart
J. [online]. Available from: URL:
http://www.eurheartj.oxfordjournals.org/content/early/2011/01/31/eurheartj.ehq508.full.
Accessed February 9, 2011
4. Pignatelli RH, McMahon CJ,
Dreyer WJ, Denfield SW, Price J, et al.
Clinical characterization of left ventricular
noncompaction in children: A relatively common
form of cardiomyopathy. Circulation.
2003;108:2672-78.
5. Suvarna JC, Deshmukh CT,
Hajela SA. Left ventricular noncompaction: a
cardiomyopathy often mistaken. Indian J Med Sci.
2009;63:303-7.
6. Ichida F, Hamamichi Y,
Miyawaki T, Ono Y, Kamiya T, Akagi T, et al.
Clinical features of isolated noncompaction of
the ventricular myocardium: long- term clinical
course, hemodynamic properties, and genetic
background. J Am Coll Cardiol. 1999; 34:233-40.
7. Chin TK, Perloff JK,
Williams RG, Jue K, Mohrmann R. Isolated
noncompaction of left ventricular myocardium: A
study of eight cases. Circulation.
1990;82:507-13.
8. Jenni R, Oechslin E,
Schneider J, Attenhofer Jost C, Kaufmann P.
Echocardiographic and pathoanatomical
characteristics of isolated left ventricular
non-compaction: a step towards classification as
a distinct cardiomyopathy. Heart.
2001;86:666-71.
9. McMahon CJ, Pignatelli RH,
Nagueh SF, Lee VV, Vaughn W, et al. Left
ventricular noncompaction cardiomyopathy in
children: characterisation of clinical status
using tissue Doppler- derived indices of left
ventricular diastolic relaxation. Heart.
2007;93:676-81.
|

