|
|
|
Indian Pediatr 2010;47: 339-341 |
 |
Serum ALT: LDH Ratio in Typhoid Fever and
Acute Viral Hepatitis |
|
S Balasubramanian, K Kaarthigeyan, S Srinivas* and R
Rajeswari
From the Department of Pediatrics and *Pediatric
Gastroenterology, Kanchi Kamakoti CHILDS Trust Hospital,
Chennai, India.
Correspondence to: Dr S Balasubramanian, Senior
Consultant Pediatrician, Kanchi Kamakoti CHILDS Trust Hospital, 12-A,
Nageswara Road, Nungambakkam, Chennai 600 034, TN, India.
Email: [email protected]
Received: September 15, 2008;
Initial review: October 18, 2008;
Accepted: February 10, 2009.
Published online: 2009. April 15.
PII : S097475590800558-2 |
|
Abstract
In 100 consecutive children aged below 18 years with
confirmed typhoid fever, 29 had moderate hepatitis. Serum alanine amino
transferase: lactate dehydrogenase (ALT: LDH) ratios of these 29
children at the time of hospitalization were compared with that of 29
children with acute viral hepatitis. The serum ALT: LDH ratio levels
(expressed in multiples of upper limit of normal) was found to be less
than 9 in typhoid hepatitis and more than 9 in acute viral hepatitis.
Serum ALT: LDH ratio helps to differentiate typhoid hepatitis from acute
viral hepatitis.
Key words: Acute viral hepatitis, Enteric fever, ALT: LDH
ratio, Typhoid hepatitis.
|
|
S
almonella hepatitis is known to
clinically mimic acute viral hepatitis(1,2). The differentiation between
typhoid fever and evolving acute viral hepatitis in a child presenting
with fever, hepatomegaly, elevated transaminases with or without jaundice
assumes paramount significance in clinical practice in a country where
both diseases are common, since the former has definitive treatment in the
form of antimicrobials. We studied the profile of hepatobiliary
involvement in children with typhoid fever and evaluated the significance
of ALT: LDH ratio in differentiating typhoid hepatitis from acute viral
hepatitis.
Methods
A descriptive case control study was carried out at
Kanchi Kamakoti Childs Trust Hospital, a tertiary care children’s hospital
at Chennai, India from March 2003 to March 2005. 100 consecutive children
with confirmed typhoid fever (blood culture positive for Salmonella
typhi) were evaluated with special reference to hepatobiliary
manifestations. They were hospitalized and investigated with complete
blood counts, abdominal sonogram, complete liver functions tests, serum
lactate dehydrogenase (LDH), prothrombin time (PT) and activated partial
thromboplastin time (aPTT). The children were classified as having mild,
moderate and severe hepatitis based on serum alanine amino transferase
levels: 2-3 times, 3-20 times and more than 20 times above the upper limit
of normal, (40 IU/L), respectively. Children were followed up to detect
any complication.
The controls consisted of 29 children with a clinical
picture consistent with acute viral hepatitis and jaundice and IgM
positive for Hepatitis A or E viruses. Their serum ALT levels, serum LDH
levels and serum ALT: LDH ratio at hospitalization was compared with the
subgroup of 29 children with typhoid having moderate to severe hepatitis.
Statistical analysis: Z- test was used to
compare the significance of difference between arithmetic means and
standard deviations of ALT and LDH in viral and typhoid hepatitis. The
ratio analysis was carried over to find the upper and lower bounds of
serum ALT: LDH ratios in typhoid and viral hepatitis. Fischer ‘F’ test was
used to identify the existence of variability and consistency between ALT:
LDH ratios in typhoid and viral hepatitis. Statistical analysis was done
using SPSS version 11.0 and a P value <0.05 was considered
significant.
Results
Of the 100 children with enteric fever enrolled into
the study (66 boys and 34 girls), 44 children were below 5 years of age
and these included 7 infants. Hepatomegaly was noticed in 54% children,
splenomegaly in 37% and hepatosplenomegaly in 36%. Icteric hepatitis was
seen in 4% of typhoid patients whereas anicteric hepatitis was more
common. Fifty-nine cases had elevated serum transaminases more than two
times above the upper limit of normal (i.e. > 80 IU/L). Thirty children
had mild hepatitis and 29 children had moderate hepatitis. Prolongation of
PT/PTT was seen in 4% of patients and only one child had bleeding
manifestations in the form of upper gastrointestinal bleeding.
Serum ALT was elevated to a greater extent in viral
hepatitis than in typhoid hepatitis; while serum LDH was elevated to a
greater extent in typhoid hepatitis than in viral hepatitis (Table
1) and these differences were statistically significant. Serum
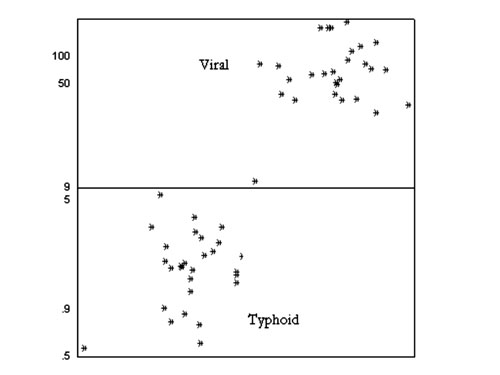
ALT: LDH ratio at the time of hospitalization, when levels of the enzymes
were expressed in multiples of the upper limit of normal, was found to be
more than 9 in acute viral hepatitis and less than 9 in typhoid hepatitis
(Fig.1).
Table I
Serum ALT and LDH in Typhoid and Acute Viral Hepatitis
|
|
Serum ALT (IU/L) |
Serum LDH (IU/L) |
ALT: LDH Ratio |
|
|
Range |
Mean±SD |
P value |
Range |
Mean±SD |
P value |
Range |
Mean±SD |
P value |
|
Typhoid hepatitis |
120-428 |
188 ±78 |
|
348-2976 |
1103 ± 668 |
|
0.58-7.48 |
2 ± 2 |
|
|
|
|
|
<0.001 |
|
|
<0.001+ |
|
|
<0.001† |
|
Viral hepatitis |
1320-8678 |
4689 ± 1883 |
|
245-874 |
582 ± 165 |
|
10.33-192.81 |
86 ± 45 |
|
|
+Student’s t-test, †Mann-Whitney U test. |
 |
|
Fig.1 Scatter diagram showing ALT/LDH
ratios in typhoid and acute viral hepatitis. |
Discussion
The spectrum of hepatic injury in typhoid has been well
studied in adults and the liver is always affected in typhoid, although
clinical jaundice is rare(3). In our study, the incidence of typhoid
hepatitis was 59% versus only 19% documented in an earlier study in
Malaysian children(4). The incidence of
clinical jaundice in typhoid was low (4%) in our study and all 4 children
with icteric typhoid hepatitis had serum transaminases levels between 5-12
times the upper limits of normal.
This is the first study on Indian children with culture
proven typhoid to evaluate the serum LDH in differentiating typhoid
hepatitis from acute viral hepatitis. The rise in serum LDH in typhoid
occurs early during the disease and is attributed to cell necrosis of
intestinal lymphatic tissue(5). Serum LDH could serve as an additional
clue in the diagnosis of typhoid hepatitis apart from clinical pointers to
typhoid, like fever persisting beyond the 1st week and a lower incidence
as well as milder degree of jaundice, and lower levels of elevation of
serum transaminases than in acute viral hepatitis. Thus the combination of
lower levels of serum ALT and higher levels of serum LDH in typhoid
combine to give a lower serum ALT: LDH ratio than in acute viral
hepatitis. Serum ALT: LDH ratio has been studied earlier in adults and
suggested as a useful point in differentiating typhoid hepatitis from
acute viral hepatitis(1,6). All cases of typhoid hepatitis had admission
ALT: LDH ratio less than 4 and all cases of acute viral hepatitis had
values above 5 in the study(1). In our study, all cases of typhoid
hepatitis had admission ALT: LDH values below 9 and all cases of acute
viral hepatitis had values above 9. If a cut-off value of 4 had been used
in our study, typhoid hepatitis could be misclassified as viral hepatitis.
Since there is no overlap between the cut-offs, construction of an ROC
curve is not possible and sensitivities and specificities of different
cut-offs were not calculated.
Serum LDH may also be elevated in other conditions like
toxic and ischemic hepatitis(7). Our study has not evaluated serum LDH in
other common febrile conditions with mild to moderate hepatitis like
malaria, dengue hemorrhagic fever and leptospirosis.
Contributors: SBS designed the study and will act
as a guarantor. SS and KK analyzed data. SBS and KK were involved in
review of literature and preparation of manuscript. RR collected data and
carried out clinical examination.
Funding: None.
Competing interests: None stated.
|
What This Study Adds?
• Serum ALT: LDH ratio is less than 9 in typhoid
hepatitis and more than 9 in acute viral hepatitis in children.
|
References
1. El-Nehiwi HM, Alamy ME, Reynolds TB. Salmonella
hepatitis: analysis of 27 cases and comparison with acute viral hepatitis.
Hepatology 1996; 24: 516-519.
2. Gurkan F, Derman O, Yaramis A, Ece A. Distinguishing
features of Salmonella and viral hepatitis. Pediatr Inf Dis J 2000;
19: 587.
3. Morgenstern R, Hayes PC. The liver in typhoid fever:
always affected, not just a complication. Am J Gastroenterol 1991; 86:
1235-1239.
4. Malik AS. Complications of bacteriologically
confirmed typhoid fever in children. J Trop Pediatr 2002; 48: 102-108.
5. Fumagalli G. Behaviour of Lactate dehydrogenase in
typhoid infection. Minerva Med 1977; 68: 1199-1204.
6. Das D, Mandal SK, De BK. Typhoid hepatitis. J Assoc
Phy India 2003; 51: 241.
7. Cassidy WM, Reynolds TB. Serum lactic dehydrogenase
in the differential diagnosis of acute hepatocellular injury. J Clin
Gastroenterol 1994; 19: 118-121.
|
|
|
 |
|

