|
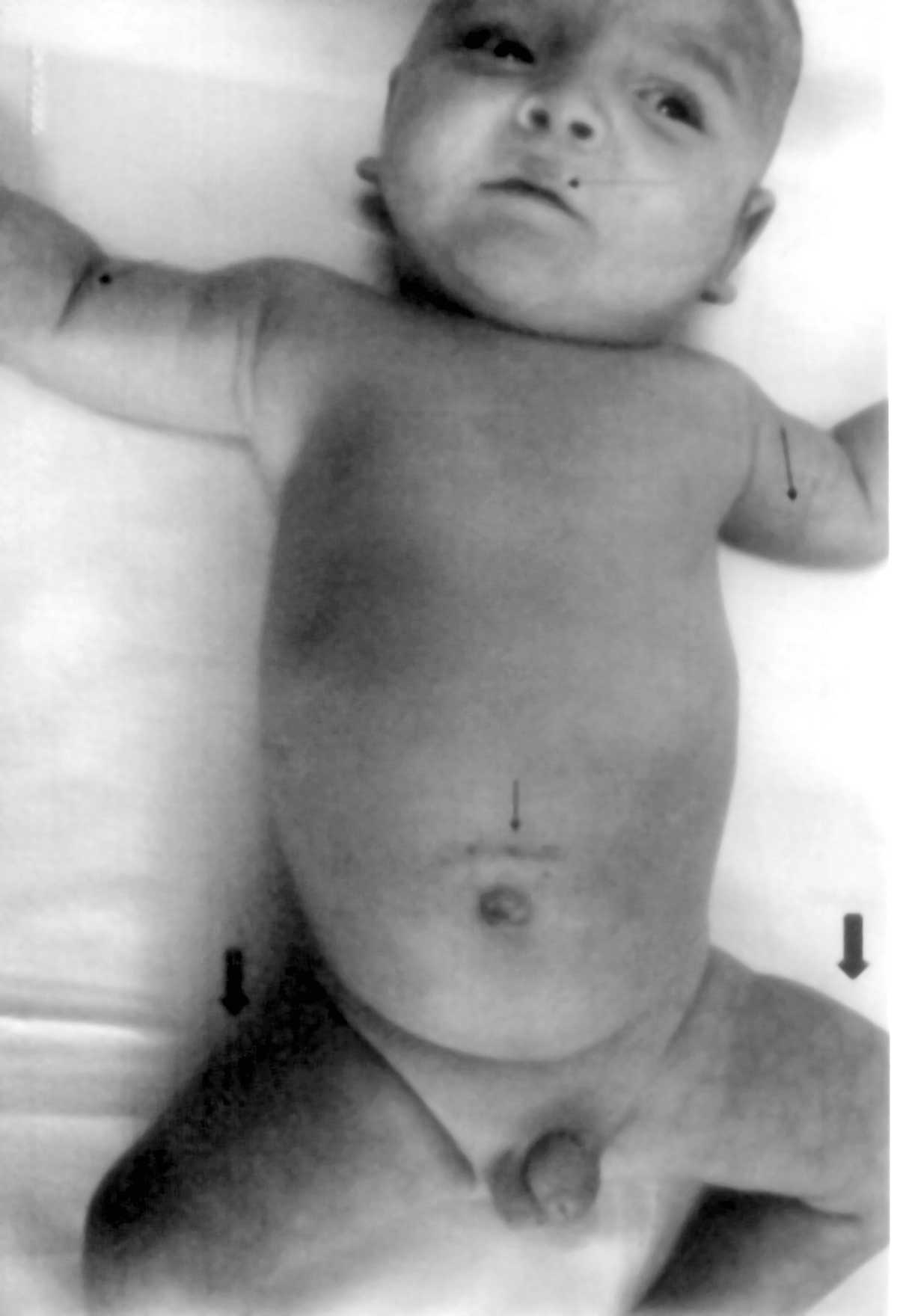
A 5-month-old boy patient was referred to us because of skin problems.
The parents were second cousins. There was no family history of
congenital skin or vascular diseases. He was born premature and
suffered from hypoxic ischemic encephalopathy, respiratory distress
syndrome and septic shock. He was kept in the neonatal intensive care
unit for fifty days and had required six cutdown procedures because of
management of life-threatening episodes of septic shock. At the age of
two months, he developed multiple reticuled, blue-violet skin lesions,
midline nevus flammeus along the upper lip, cavernous hemangioma at
the frontoparietal region and the chin (Fig. 1.). The skin
lesions were distributed all over the body especially below umbilicus.
We thought that these features of cutis marmorata telengiectatica
congenital (CMTC) might be connected with the vascular trauma because
of repeated cutdown procedures, although Doppler study of venous and
arterial system was normal. Brain computerized tomography revealed
left hemispheric atrophy, asymmetric dilatation of left lateral
ventricle and calcification at left basal ganglion level.
 |
|
Fig. 1. Typical reticulated blue-violet
net-work is evident on the left arm, right and left leg (thick
arrows). Note nevus flammeus of philtrum and upper lip (dotted
arrow) and three cutdown scars (thin arrows).
|
A number of hypothesis have been proposed for the
pathogenesis of CMTC, including environmental factors, autosomal
dominant inheritance with low or variable penetrance, a multifactorial
cause or a lethal gene surviving mosaism, a peripheral neural
dysfunction, and a failure of development of the mesodermic vessels in
the early embryonic stage(1-4). We suggest that a failure of
development of vessels might be because of septic shock and frequently
repeated cut- down procedures. One of the most serious complications
of cutdown procedures is probably arterial thrombosis. And also,
repeated microthrombosis might lead to increased peripheral flow
resistance, which causes a perfusion deficit, and thus explain the
reduced oxygen saturation in the tissues and specific skin problems.
Although, we could not confirm this theory, we presume a functional
malformation at the level of the terminal blood vessels.
Osman Baspinar,
Selim Kervancioglu,*
Departments of Pediatrics,
and *Radiodiagnostics,
Gaziantep University, Faculty of Medicine,
Gaziantep, Turkey.
E-mail: baspinar@gantep.edu.tr
1. Amitai DB, Fichman S, Merlob P, Morad Y,
Lapidoth M, Metzker A. Cutis marmorata telengiectatica congenita:
Clinical findings in 85 patients. Pediatr Dermatol 2000; 17:
100-104.
2. Gerritsen MJ, Steijlen PM, Brunner HG, Rieu P.
Cutis marmorata telangiectatica congenita: Report of 18 cases. Br J
Dermatol 2000; 142: 366-369.
3. Devillers AC, de Waard-van der Spek FB, Oranje
AP. Cutis marmorata telangiectatica congenital: Clinical features in
35 cases. Arch Dermatol 1999; 135: 34-38.
4. Mazereeuw-Hautier J, Carel-Caneppele S, Bonafe JL. Cutis
marmorata telengiectatica congenita: report of two persistent cases.
Pediatr Dermatol 2002; 19: 506-509.
|
