Case Report
An 8-year-old boy was admitted to hospital because of
recurrent fever (normal in the morning and febrile during night, ranged
from 39.5º C to 40.0º C) for 1 month. There was no cough except on the
first and second day. No angina, tetter, arthralgia, dyspepsia,
vomiting, night sweats, or abdominal pain were noted. He had no history
of chronic liver disease or foreign travelling and no family history of
serious illness. The patient had received intravenous cephalosporins or
penicillins for 20 days, but did not recover.
Physical examination showed normal vital signs except
for a temperature of 40º C. There was no skin lesion or peripheral
stigmata of chronic liver disease. Several cervical lymph nodes were
palpable with 0.5-1.0 cm in diameter, and no axillary or inguinal nodes
were noted. The head, ears, eyes, nose, throat, cardiac and pulmonary
examinations were all normal. The spleen was not palpable. The liver
span was 9-10 cm by percussion, easily felt 1cm with soft and smooth
edge below the right costal margin in the midclavicular line. The
neurological examination was normal.
Laboratory findings
He had increased C-reactive protein (CRP: 30 mg/L)
and erythrocyte sedi-mentation rate (ESR: 72 mm/hr). Other results of
routine laboratory studies revealed: Hemo-globin, 104-105g/L; WBC,
5.3-7.5 × 109/L; lymphocytes, 21.3-39.2%; polymorpho-nuclear leukocytes,
76.4 - 52.5%; Platelets, 349-359 × 109/L; eosinophils, 75/mL.
Flow cytometry analysis results: CD3, 30.22%; CD4, 11.48%; CD8, 12.18%;
CD2, 49.23%; CD5, 0.15%; CD7, 37.84%; CD1a, 0.40%; CD25, 3.83%; CD56,
18.56%; CD19.09%; CD34, 1.01%; HLA-DR, 25.02%; TCRa/b, 20.31%; TCRr/d,
7.54%. No malignant clone was identified.
The bone marrow seen with light microscopy had normal
cellularity; the erythrocytic series increased and significant
granulocytic hyperplasia was present. Granules increased and
vacuolization was found in the cytoplasm of some granulocytes.
Lymphocytic series were hypoplastic, but the numbers of mega-karyocytes
were normal.
Viral serologies were negative for hepatitis A,
hepatitis B, hepatitis C, hepatitis D, hepatitis E and HIV markers.
Other laboratory examination results were normal or negative, including
chest X-ray, ECG, serum levels of antinuclear antibody,
tuberculosis antibody, rheumatoid factor, antistreptolysin O antibody,
Epstein-Barr virus antibody, Purified protein derivative, Chlamydia
pneumoniae antibody, somatic O antigens and flagellar H antigens of
Salmonella, blood culture, bone marrow culture, total protein, total
bilirubin, alkaline phosphatase, alanine aminotransferase, total IgG,
IgA, IgM, IgE, C3 and C4.
Imaging findings
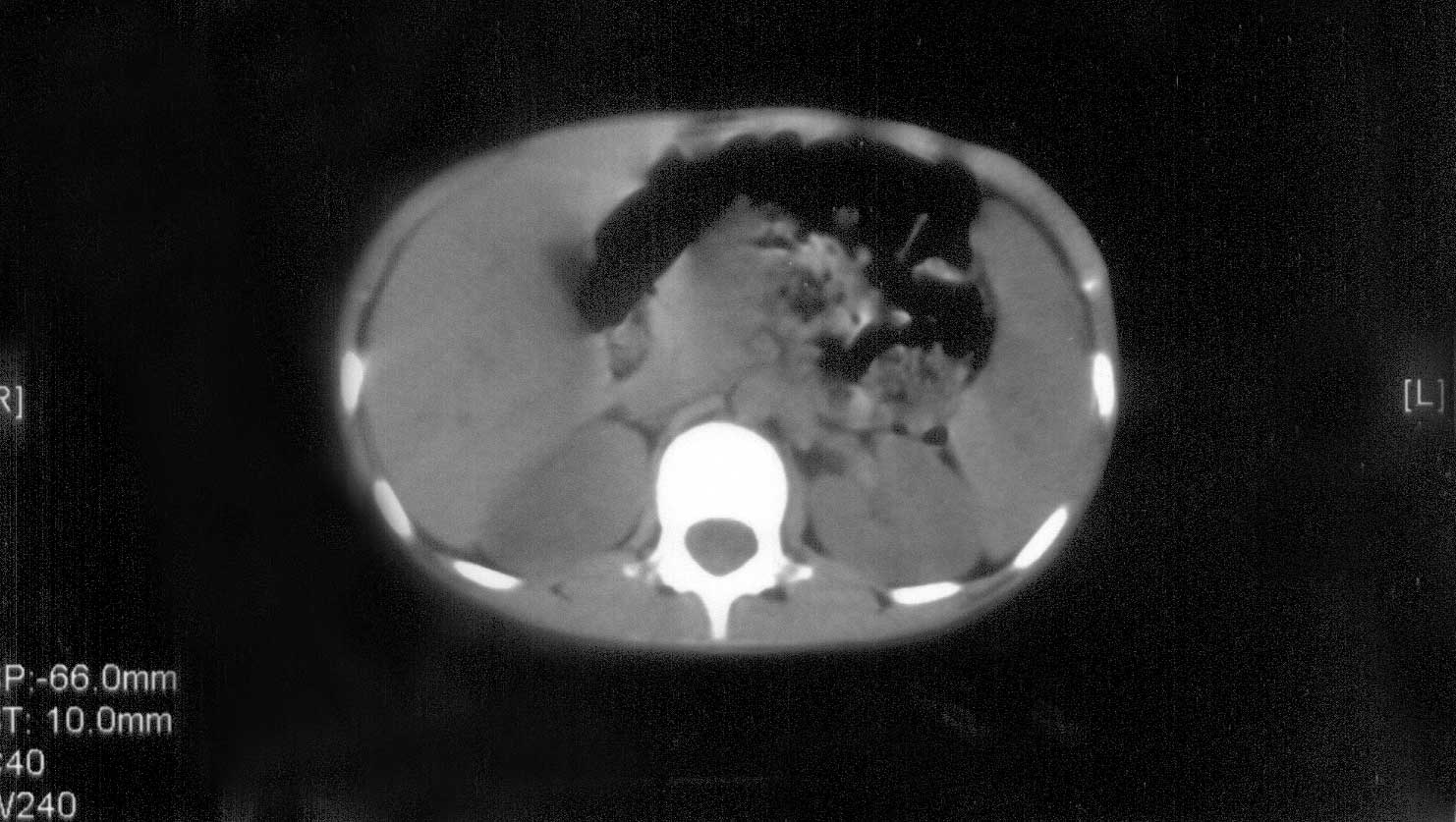
An abdominal computerized tomography (CT) examination
shown several low-attenuation lesions diffusely located in the spleen (Fig
1). Abdominal ultrasound (US) with 3.5 MHz convex transducer was
also done. The length of the liver (9.1 cm) and the width of portal
trunk (0.7 cm) were all in normal ranges. The length in the major axis
(7.8 cm) and thickness of the spleen (3.2 cm) were in normal ranges as
well. However, many small, hypoechoic, rounded, wedge-shaped and
well-defined nodules in spleen were found as in diffuse infiltration (Fig
2). Lesion diameter was about 0.5-1.0 cm and the biggest was 1.20 ×
1.06 cm. Blood flow was found in these lesions by color Doppler flow
imaging. Enlarged abdominal lymph nodes, including para-aortic lymph
nodes (the largest 1.54 × 0.91 cm) and mesenteric lymph nodes (the
largest 1.03 × 0.65 cm), were also found.
 |
|
Fig. 1. Abdominal computerized tomography
examination. Unenhanced CT image showing several low-attenuation
lesions diffusely in spleen. |
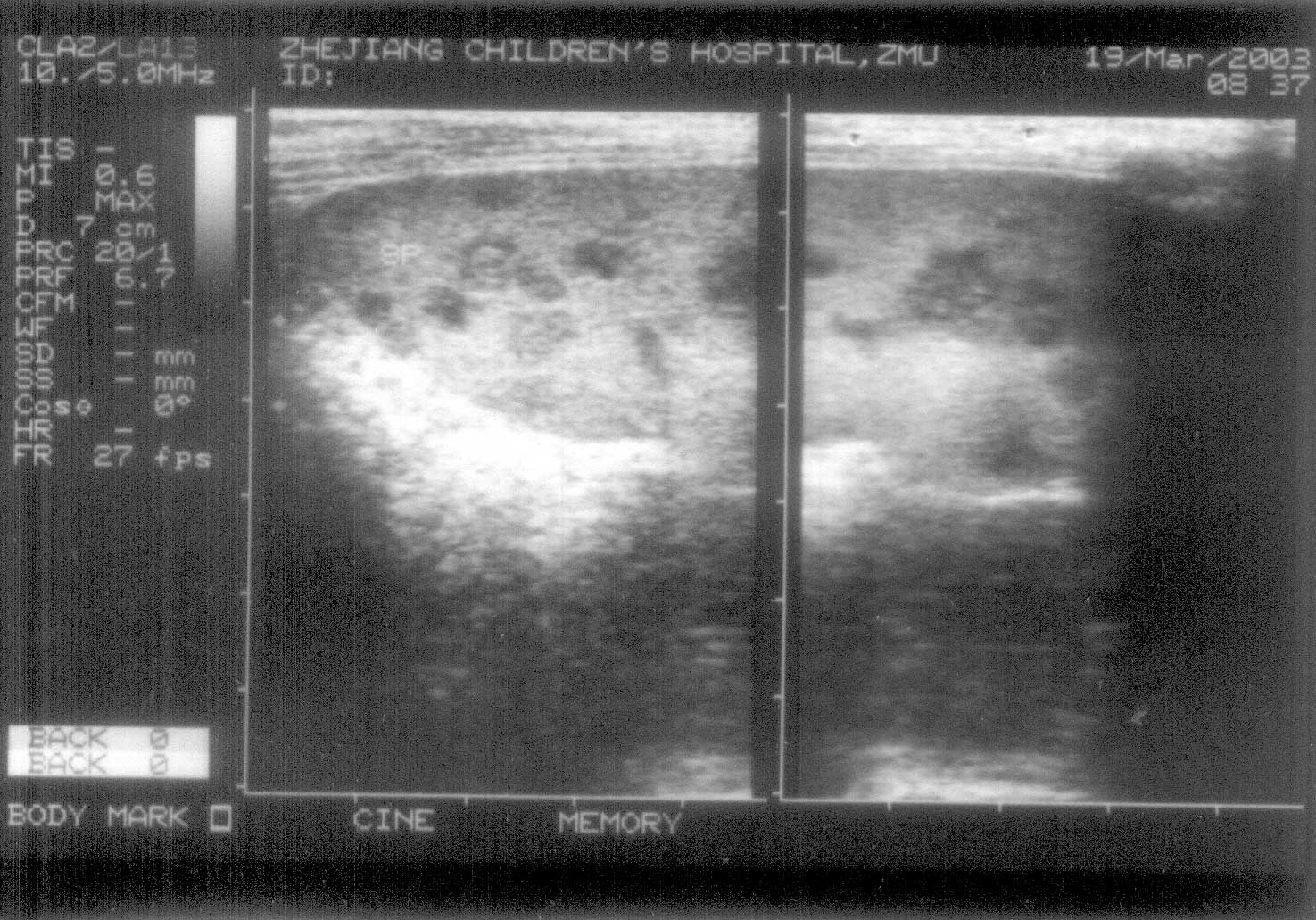 |
| Fig. 2. Abdominal ultrasound
examination showing many small, hypoechoic, rounded, wedge-shaped
and well-defined nodules diffusely in spleen. |
Clinical course
On the fifth day of hospitalization, the spleen was
found to be enlarged (the thickness of spleen was 3.6 cm) and no echoic
space, which implied internal fluid, was found in these lesions. After a
positive Mycoplasma pneumoniae (MP) IgM (1 : 32) was reported on the
sixth day, azithromycin (10 mg/kg.day for 5 days) was used intravenously
and the temperature was returned to normal in 3 days. CRP (<8 mg/dL) and
ESR (15 mm/hr) recovered in 1 week. The size of spleen (the thickness of
spleen was 2.9 cm) and splenic lesions (the biggest lesion was 1.05 ×
0.74 cm) decreased in 2 month and 10 days later. The lesions and
enlarged lymph nodes dis-appeared, MP IgM antibody became negative (<1 :
8) and IgG antibody was positive (1 : 32) in 6 months later.
Discussion
Mycoplasma pneumoniae (MP) is a frequent cause of
community-acquired respiratory infections in children and adults,
especially in school-aged children(1-2). It is also responsible for a
wide spectrum of non-pulmonary manifestations including hematological,
gastrointestinal, renal, cardiac and central nervous system
diseases(3-6). Certain observations are suggestive and can be helpful to
the physician, for example, pneumonia in young adults, serum cold
hemagglutinins in a titer of 1 : 64, a positive IgM MP antibody,
polymerase chain reaction or effective treatment with macrolies(7,8).
The cause of hospitalization in this case was mainly
the persisting fever for 1 month. Imaging findings included splenomegaly
and multiple hypoechoic nodules within spleen. To present knowledge, no
previous report suggested that multiple hypoechoic nodules in spleen
without respiratory manifestation are associated with MP infection. In
this case, however, some clinical feature and laboratory results
supported MP infection, including (1) a school-aged children, (2) fever
and cough in the first and second days, (3) positive and increasing MP-IgM
antibody in short period of time, and (4) effective treatment with
azithromycin and resistance to penicillins and cephalosporins.
As we know, there are two mechanisms for the
development of MP associated disease: direct invasion mechanism and
immune-mediated mechanism(6,9). Because azithromycin was very effective
in this case and the fever recovered in three days, we postulated that
direct organism invasion rather than autoimmune mechanisms played an
important role in the lesion of spleen. The limitation of this report
was that pathologic biopsy of the lesions in spleen were not done, so we
are not sure that these hypoechoic nodules in spleen is a lymphocytic
proliferating lesion or an abscess due to cell-mediated immune response.
As no abdominal pain and no capsule of these hypoechoic nodules were
detected, we suspected theses nodules were not abscess, but focal
nodular hyperplasia as a result of direct MP invasion. Similar lesion in
liver had been found by ultrasound because of focal nodular
hyperplasia(10).
Contributors: Both authors were involved in case
management, search of literature and writing the report.
Funding: None.
Competing Interests: None stated.
