|
|
|
Indian Pediatr 2016;53: 841 |
 |
Long QTc Syndrome and Propionic Acidemia
|
|
* Moisés Rodríguez-González and
Ana Castellano-Martínez
From Pediatric Cardiology Section, Hospital
Universitario Puerta del Mar, 34th of Ana de Viya Avenue, Cádiz, Spain.
Email: [email protected]
|
|
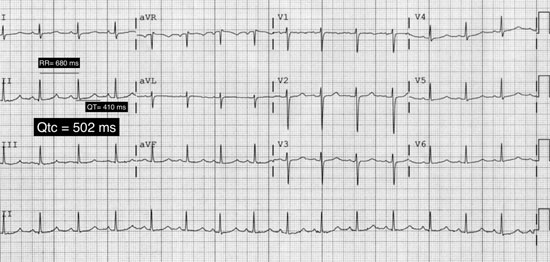
A 9-year-old boy diagnosed as Propionic acidemia at 2 months of age,
complained of palpitations and near-syncope episodes related with
exercise. His metabolic condition was well controlled on sodium
benzoate, carnitine, protein-free diet and biotin treatment. A prolonged
QTc interval was noted on ECG-Holter (Fig. 1).
Echocardiography showed no anomalies. He fulfilled criteria for
diagnosis of Long QTc Syndrome (LQTS) [1], and treatment with
propranolol was initiated with an observed decrease of the QTc interval
to normal values. Acquired causes of LQTS were discarded, and genetic
test was negative. At present he remains asymptomatic without cardiac
events, and is under periodic follow-up.
 |
|
Fig. 1 ECG showing prolonged QTc
interval (Maximun 502 ms).
|
Patients with propionic acidemia can develop cardiac
complications such as dilated cardiomyopathy and sudden cardiac death,
both dependent of the metabolic state [2]. Recent literature highlights
the association of propionic acidemia and LQTS, two disorders that are
potentially lethal separately [3-5]. This association increases the risk
of life-threatening cardiac events in these patients. The QTc interval
prolongation is observed up to 70% of patients with propionic acidemia
during their follow-up [3]. It is independent of the metabolic state and
tends to increase with age [3].
Various pathogenetic mechanisms have been proposed
but not proved; e.g., deficiency of carnitine, a direct toxic
metabolic effect, an intracardiac depletion of essential substrates in
the intermediary metabolism or the inhibition of the oxidative
phosphorylation in mitochondria [3]. Recently the possibility of a
genetic linkage has been proposed because of the genetic defect causing
LQTS type 3 has been mapped to 3p-21 (SCN5A gene), and propionic
acidemia encoding genes for the a
subunit were found on chromosome 3q13.3-q2 [3].
Because of the increased risk of having LQTS and
sudden cardiac death in children with propionic acidemia, a regular
follow-up with a 12-lead ECG, echocardiography, Holter monitoring and
exercise testing is warranted. When LQTS is diagnosed, therapy with
beta-blockers along with lifestyle changes and avoidance of factors that
prolong QTc interval must be initiated.
Funding: None; Competing Interest: None
stated.
References
1. Schwartz PJ, Ackerman MJ. The long QT syndrome: A
transatlantic clinical approach to diagnosis and therapy. Eur Heart J.
2013;34:3109-16.
2. Sutton VR, Chapman KA, Gropman AL, MacLeod E,
Stagni K, Summar ML, et al. Chronic management and health
supervision of individuals with propionic acidemia. Mol Genet
Metab.2012;105:26-33.
3. Baumgartner D, Scholl-Bürgi S, Sass JO, Sperl W,
Schweigmann U, Stein J-I, et al. Prolonged QTc intervals and
decreased left ventricular contractility in patients with propionic
acidemia. J Pediatr. 2007;150:192-7.e1.
4. Jameson E, Walter J. Cardiac arrest secondary to
long QTc in a child with propionic acidemia. Pediatr Cardiol.
2007;29:969-70.
5. Kakavand B, Schroeder VA, Di Sessa TG. Coincidence
of long QT syndrome and propionic acidemia. Pediatr Cardiol.
2005;27:160-1.
|
|
|
 |
|

