|
|
|
Indian Pediatr 2015;52:
787-794 |
 |
Teaching and Assessing Clinical Reasoning
Skills
|
|
* Jyoti Nath Modi,
$Anshu,
#Piyush Gupta and
Tejinder Singh
From Departments of *Obstetric and Gynecology,
People’s College of Medical Sciences and Research Centre, Bhopal;
$Pathology, Mahatma Gandhi Institute of Medical Sciences,
Sevagram; #Pediatrics, University College of Medical
Sciences, New Delhi; and CMCL-FAIMER Regional Institute, Christian
Medical College, Ludhiana, Punjab; India.
Correspondence to: Dr Tejinder Singh, Professor of
Pediatrics and Medical Education, Christian Medical College,
Ludhiana 141 008, India.
Email: [email protected]
|
Clinical reasoning is a core competency expected to be acquired by all
clinicians. It is the ability to integrate and apply different types of
knowledge, weigh evidence critically and reflect upon the process used
to arrive at a diagnosis. Problems with clinical reasoning often occur
because of inadequate knowledge, flaws in data gathering and improper
approach to information processing. Some of the educational strategies
which can be used to encourage acquisition of clinical reasoning skills
are: exposure to a wide variety of clinical cases, activation of
previous knowledge, development of illness scripts, sharing expert
strategies to arrive at a diagnosis, forcing students to prioritize
differential diagnoses; and encouraging reflection, metacognition,
deliberate practice and availability of formative feedback. Assessment
of clinical reasoning abilities should be done throughout the training
course in diverse settings. Use of scenario based multiple choice
questions, key feature test and script concordance test are some ways of
theoretically assessing clinical reasoning ability. In the clinical
setting, these skills can be tested in most forms of workplace based
assessment. We recommend that clinical reasoning must be taught at all
levels of medical training as it improves clinician performance and
reduces cognitive errors.
Keywords: Assessment, Clinical problem solving, Clinical
reasoning, Diagnostic reasoning, Medical decision-making, Medical
education.
|
|
T
he challenge of medicine lies in its complexity.
One of the most important skills that a doctor needs to have is the
ability to translate the unorganized information received from the
patient into the language of medicine. In a short period of time,
physicians are expected to work their way, starting from the presenting
symptoms of patients to the diagnosis, and plan of management pertinent
to the patient’s specific context. They also need to decide about which
direction to proceed in, which information to discard, and when to stop
looking for more information. This calls for a phenomenal degree of
observation, comprehension, recall, alertness and reasoning.
What is Clinical Reasoning?
Clinical reasoning has been defined as ‘ability to
sort through a cluster of features presented by a patient and accurately
assign a diagnostic label, with the develop-ment of an appropriate
treatment strategy as the end goal’ [1]. Clinical reasoning has also
been defined as ‘the ability to integrate and apply different types of
knowledge, to weigh evidence, critically think about arguments and to
reflect upon the process used to arrive at a diagnosis’ [2,3].
The terminology may vary to include terms such as
‘clinical/medical problem solving’ or ‘diagnostic reasoning’, but the
essence remains that it is a complex cognitive process leading to
meaningful interpretation of patients’ problems and formulation of an
effective management plan.
Experts agree that clinical reasoning is an essential
skill that must be developed during the early years in training and
further refined during subsequent years of practice. It must be taught
at all levels of medical training [4-6]. Over the last few decades, it
has been considered a crucial aspect of physician competence and is
explicitly included in most medical schools’ documents [6].
The Medical Council of India’s proposed Graduate
Medical Education Regulations (2012) also lists ‘effective clinical
problem solving’ as one of the skills to be developed in medical
graduates [7].
Advantages of Learning Clinical Reasoning Skills
Clinical reasoning skills not only help physicians in
reaching an appropriate diagnosis, but are also the key to preventing
diagnostic errors. Diagnostic errors in medicine may occur in 5-15% of
cases [8]; two-thirds of these are cognitive errors which include flaws
in diagnostic reasoning, and decision making. Deeper understanding of
the processes involved in acquisition of clinical reasoning skills will
thus help in reducing cognitive errors.
Process of Clinical Reasoning
Educational psychologists have explored the process
of medical decision making extensively, and these perspectives have
changed over time [6, 9]. It is not within the scope of this article to
discuss these theories, their evolution or evidence. We shall restrict
ourselves to merely mentioning one of the models of clinical reasoning-
namely Croskerry’s dual processing theory [10, 11].
Dual Processing Theory
Croskerry’s model proposes that clinicians use two
types of cognitive processes to arrive at a diagnosis: System 1
approaches and System 2 approaches. System 1 approaches are intuitive,
draw on past experience, and may be based entirely on pattern
recognition or heuristics [10, 11]. On the other hand, System 2
approaches are slower, analytical, more deliberate and involve deeper
thinking (Table I). The two processes are not mutually exclusive.
|
TABLE I Dual Processing Theory: System 1
and System 2 Approaches
|
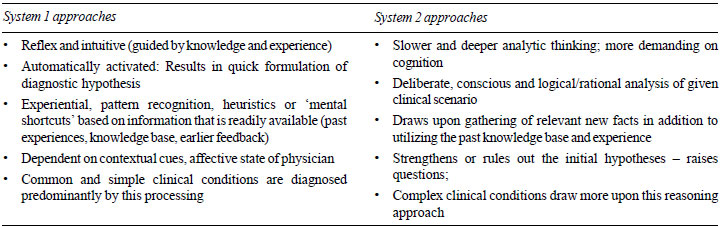 |
Clinicians tend to switch between both approaches
depending on the complexity of the case [12]. In the learning phase, one
tends to use more of System 2 or analytical approaches, and as expertise
sets in there is a tendency to use more of System 1 or pattern
recognition approaches. However even when experts encounter challenging
cases, they tend to revert to System 2 approaches. During teaching, more
emphasis is laid on System 2 processes, but in practice, physicians use
System 1 processes more often. Hence there is need to train learners in
System 1 approaches right from the beginning.
Educational Strategies to Teach Clinical Reasoning
Problems with clinical reasoning often occur because
of inadequate knowledge of the disease, failure to activate prior
knowledge, flaws in data gathering and improper approaches to
information processing [5].
It is a challenge for clinical educators to diagnose the learner’s
approach to clinical reasoning and guide them towards correct
approaches.
Clinical reasoning is perhaps best taught during the
course of a clinical encounter either conducted by the physician-teacher
(for demonstration), or preferably during observation of a clinical
encounter being carried out by the student. Clinical case presentations,
case based discussions/ chart stimulated recall, clinical problem
solving exercises and structured case presentation models like SNAPPS
(refer Box 1) and One Minute Preceptor (all discussed in detail later)
are good settings for teaching clinical reasoning skills.
We enumerate some strategies which when used
consciously by educators will encourage students to learn clinical
reasoning approaches (Table II) [13,14].
|
TABLE II Educational Strategies to
Encourage Clinical Reasoning
|
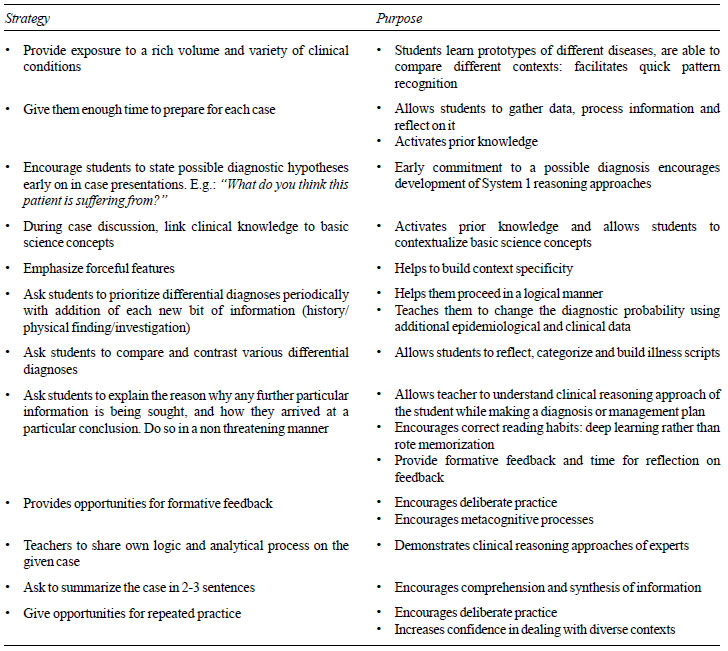 |
Exposure to a wide variety of clinical conditions:
Learning is contextual. Success in solving one kind of clinical problem
is a poor predictor of success when faced with another clinical
situation. A student thus needs exposure to a wide variety and large
numbers of clinical cases during training [1, 6]. Students can learn
prototypes of different diseases by this approach [15].
Activation of prior knowledge: Asking students
for their reasoning based on pathophysiologic knowledge also enables
them to recall and contextualize relevant basic sciences concepts [16,
17].
Emphasize forceful features: Many clinical
conditions may be recognized by certain ‘key features’ or ‘forceful
features’ or ‘anchor points’. Students must be asked to observe these
forceful features that serve as trigger in the memory for recognition of
the condition when encountered again [13]. Pattern recognition based on
above helps the physicians not only in identification of clinical
condition but also in discriminatory thinking processes [9].
Categorization and illness scripts: It is
impossible to learn the frequency of every sign and symptom of each
disease. One of the basic differences between the approaches of experts
and novices is that experts are able to mentally categorize diseases in
a logical manner [18]. The expert’s mind stores the information
pertaining to clinical conditions or diseases in the form of ‘illness
scripts’– or the predictable details of the condition such as
predisposing factors, clinical presentation, complications, etc. [1,
19]. They learn to retrieve and apply this information reflexively.
Students need to be taught or exposed to clinical
cases in a manner that they gradually develop these mental prototypes of
disease or ‘illness scripts’. This can be done by guiding learners’
thought processes by way of asking relevant questions. These questions
should encourage them to (a) propose differential diagnoses based
on minimal clinical details; (b) modify diagnostic hypothesis as
more information is available; and (c) justify or refute
hypotheses based on their background knowledge or by asking them to
compare and contrast most likely differential diagnoses [13,19]. Another
way of teaching students to build on their illness scripts is to ask
them to reflect on a previous patient with similar findings and compare
presentations.
Two models of structured case presentations which
encourage building of illness scripts or mental schemata are discussed
here –the SNAPPS model, and the One Minute Preceptor (OMP) model. These
can be utilized for teaching as well for formative assessment and are
designed for use by the physician-teacher in a busy office or
out-patient setting [20].
|
Box 1: SNAPPS Model for Structured Case
Presentation
|
|
• Summarize the case
• Narrow the
differential diagnosis
• Analyse the
differentials
• Probe the preceptor
about uncertainties
• Plan management for
the patient
• Select case related issues for self
study
|
• SNAPPS model (Box 1) can help learners
build illness scripts essentially by way of comparing differential
diagnoses and clarifications of uncertainties [21]. This method
encourages expression of intuitive as well as analytical thinking
and promotes self-reflection by the student [20, 21].
• The One Minute Preceptor (OMP) model is another
useful model of structured clinical case discussion. In this model,
the student presents a case, he/she is then asked to commit to a
diagnosis, and is probed for reasoning for the same [22]. The
preceptor, now aware of patient as well as student’s diagnosis,
teaches general rules (e.g. key features, principles of management,
effective communication). The final two steps are to reinforce what
was done well by the student and to correct the mistakes made.
Usually it takes about 10 minutes (arbitrary division of time could
be: 6 minutes for case presentation, 3 minutes for questioning and 1
minute for teaching the general rule and feedback) [23]. Despite
being a teacher-initiated model, it drives the student to propose
and justify the diagnosis, employing appropriate clinical reasoning
skills by the learner.
Use of checklists has also been mooted to help in
avoiding errors of omission [24].
Formative feedback: The role of providing
effective formative feedback to the learner is the single most important
feature which affects learning. Both SNAPPS and OMP models have an
inherent component of providing feedback to the students.
Encourage learners to use both System 1 and System 2
approaches: There is often a mismatch between what we know about
diagnostic reasoning and the way we teach our students. We have already
discussed that expert clinicians first make use of intuitive processes,
and go to analytical processes only later when the case does not fit our
illness scripts. We should make a deliberate effort to promote intuitive
thinking by asking the students at periodic intervals during the
presentation (i.e. when he still does not have the complete clinical
history or physical findings), the various possibilities that can be
considered. As each new piece of information is presented as the history
or physical finding, this list should change. The knowledge of
epidemiology further contributes to speed and accuracy of diagnosis.
Students should be trained to utilize the epidemiological data such as
seasonal, geographical or demographic variation of disease conditions
for narrowing down the diagnosis [25, 26]. Students must learn to
prioritize in a list of differential diagnoses in a given context,
enumerating points in favor and against each diagnosis. They should be
encouraged to explain the reason why any further particular information
is being sought, and how they arrived at a particular conclusion [27].
Another method, the Clinical Problem Solving (CPS)
exercise serves as a good setting to demonstrate clinical reasoning. An
expert physician is presented an unknown case in a stepwise fashion.
During the course of an interactive discussion between the expert and
the audience, the diagnostic process and its nuances are demonstrated
[28].
Reflection and metacognition: Students must be
encouraged and provided an opportunity to reflect on their diagnostic
approach, and think about what they could be missing. Morbidity and
mortality conferences are a good place to do this. Residents can be
asked to reflect on their delivery of patient care based on actual case
records (case based discussions) or on the discharge papers of patients
(chart stimulated recall) [29]. Portfolios may also be useful in
achieving this purpose. Such a metacognitive approach may help learners
to recognize the need to slow down and avoid errors that occur due to
premature closure of reasoning [30].
Deliberate practice: Just like a musician needs
to practise again and again to play well, clinicians too need to hone
their skills through training activities which are designed to maximize
improvement. Ericsson called these activities ‘deliberate practice’
[31]. Deliberate practice includes finding opportunities for repeated
practice, requesting honest feedback on performance at frequent
intervals, maximizing learning from each case, reflecting on feedback
and errors to improve performance and using mental practice to support
clinical experiences. This can be done during regular clinical
activities such as, asking students to report back during the morning
rounds or after an emergency floor/ call duty.
Assessment of Clinical Reasoning Ability
The assessment of clinical reasoning is challenging
as these skills are not measurable and must be inferred from behavior.
As clinical reasoning is context specific, it has to be assessed across
multiple domains, on multiple clinical scenarios, using multiple
assessment methods to draw meaningful and valid interpretations.
Moreover, these skills should be assessed throughout the course.
Learning strategies for developing clinical reasoning rely heavily on
feedback and reflection, and this is possible only when continuous
ongoing formative assessment is in place.
The assessment of clinical reasoning can be carried
out either in an authentic workplace-based clinical setting or outside
it. The standardization of assessment, reliability, feasibility and
resource efficacy may appear higher for assessments carried out in
formal examination settings. However, assessment carried out in
authentic clinical settings inherently scores higher in terms of
validity and educational impact. Reliability of these assessments can be
improved by increasing the number of clinical encounters. The issue of
feasibility can also be addressed by structured assessment tools such as
the mini clinical evaluation exercise (mini-CEX). Usefulness of some
methods in assessment of clinical reasoning ability is discussed below:
1. Multiple Choice Questions (MCQ)
A well blueprinted MCQ-based examination has the
potential of assessing wide content areas across different contexts in a
short time. Simple recall type MCQs contribute little to assessment of
medical decision making. However they can be improved to explore
clinical problem solving ability by making them contextual. This is done
by inserting clinical scenarios (Box 2).
|
Box 2:
Converting a Recall type MCQ into a Higher Order MCQ |
|
Recall type MCQ:
The commonest cause of childhood anemia in
India is:
a) Nutritional anemia b) Thalassemia
major
c) Sickle cell disease d) Aplastic anemia
Higher order Scenario-based MCQ:
A two year old boy presents with severe
pallor. He has been fed on milk-based diet. Anthropometry
revealed weight for length below -3 Z score and length
for age between -2 to -3 Z score. The child also has
tachypnea, tachycardia, angular stomatitis, and koilonychia.
There is no significant lymphadenopathy. Liver is palpable 5 cm
below costal margin. Spleen is not palpable. Rest of the
examination is normal. The most likely cause of anemia in
this child is:
a) Nutritional anemia b) Thalassemia major
c) Sickle cell disease d) Aplastic anemia
|
Extended matching questions (EMQs)
are also good for testing reasoning ability. Here
learners have to pick the answers to context-specific clinical scenarios
around a single theme from a list of options [32]. An example can be
seen in Box 3.
|
Box 3: Extended Matching Questions
|
|
Consider the following options
A. Nutritional Anemia
B. Thalassemia minor
C. Thalassemia major
D. Sickle cell trait
E. Sickle cell disease
F. Hookworm infestation
G. Aplastic Anemia
Lead in question: For each child with
anemia, select the most appropriate diagnosis:
Q. 1: A two-year-old girl
presented with severe anemia, icterus, hepatospenomegaly and
failure to thrive. Her malar bones were prominent. She has a
history of receiving two blood transfusions in the last year.
Key: C
Q. 2: A five-year-old boy presents with
increasing pallor for 1 month and cutaneous bleeds for 7 days.
Child is febrile. There is severe pallor but no lymphadenopathy.
Liver and spleen are not enlarged. Child has been consuming 1300
kcal daily including food items from all the four food groups.
Key: G
|
2. Key Feature Test
These are clinical scenario-based questions that
focus on critical steps in diagnosing or managing a particular clinical
condition. These test a step in which examinees are most likely to make
errors or a challenging aspect of the diagnosis and management in
practice. The questions are designed as case scenarios to prompt
learners to identify the key clinical feature in a clinical presentation
and plan essential steps in diagnostic and management strategies [33].
An example is shown in Box 4.
|
Box 4: Key Feature Test
|
|
An 18-month-old girl presented to emergency
with loose stools of 4 days duration. The weight for length of
the child was below -3Z score. Peripheral pulses were
weak and poorly palpable. Extremities and abdomen were cold to
touch.
Q1. Provide a list of 2 problems that
need immediate attention in this child.
[Score key: The question carries 2
marks. 1 mark is awarded each for any of the following answers:
severe dehydration, shock/septic shock, hypothermia. Any other
response (such as diarrhea, dehydration, gastroenteritis,
hypoglycemia, electrolyte imbalance, malnutrition) will carry
minus 1 mark].
Q2. Outline the three most important
life-saving measures in managing this child.
[Score key: The question carries 3
marks. 1 mark is awarded for each of the following answers; Warm
the child by placing under radiant warmer; Secure IV access and
provide bolus fluid (N/2 saline or Ringer lactate); Start
systemic (IV) antibiotics. Any other response will carry minus 1
mark].
|
3. Script Concordance Test (SCT)
This is based on the principle that the steps in the
clinical reasoning process can be assessed and compared to the reasoning
ability of a panel of experts [34]. The test design conforms to the
possible organizational structure of illness scripts in the minds of the
experts.
In Step 1, short ill-defined clinical scenario is
first provided and the examinee’s opinion is sought in terms of
diagnostic hypothesis or investigation or judgment. In Step 2, a new
piece of information is provided (clinical feature, test result, disease
progression etc.). The examinee is then asked how this new piece of
information affects their initial judgment. The decision making process
of the learners is reflected in their responses at the addition or
availability of each new piece of information. Learners’ responses are
scored using the responses by a panel of experts on the same case as a
reference [9, 19, 34]. An example of SCT is shown in Box 5.
|
Box 5: Design and Example of Script
Concordance Test (SCT)
|
|
[Step 1: Clinical Scenario] A
four year old girl presents to the outpatient department with
history of fever and sore throat since the last 3 days.
|
|
[Step 2: Diagnostic hypotheses] |
[Step 3: Additional information provided] |
[Step 4: Change in clinical judgment] |
|
If you were thinking: |
And then on subsequent interview |
This diagnosis becomes: (Use |
|
and examination, you found that: |
the scale below)* |
|
1. Viral pharyngitis |
• Fever was high grade; |
-2 , -1, 0, +1, +2 |
|
• She had difficulty in swallowing |
|
|
2. Streptococcal sore throat |
• Recently developed red rash |
-2 , -1, 0, +1, +2 |
|
• Neck glands palpable |
|
|
3. Diphtheria |
• Tonsils enlarged and with a white coating |
-2 , -1, 0, +1, +2 |
|
*-2 =Ruled out or almost ruled out; -1 = Less likely; 0= Neither more
nor less likely; +1 = More likely; +2 = Certain or almost certain.
|
4. Oral/ Viva voce Examination
Despite being resource-intensive, oral examinations
are ubiquitous in Indian medical schools. Though they are often reduced
to mere recall of facts, they have the potential of being utilized for
assessing clinical reasoning and medical decision making. Clinical
scenario based questions that probe the analytical skills of the
examinee may be utilized. Further, multiple clinical scenarios may be
used to assess across subject areas [32].
5. Long Case Examination
Long case remains the mainstay of most clinical
examinations conducted in our country. Usually the student works-up an
allotted case (unobserved) and presents the same to the assessor. The
assessor then asks clarifying questions or may ask to demonstrate a
clinical sign. Though the long case examination is effort-intensive as
well as time-consuming, it provides an oppportunity to the examiner to
assess the clinical reasoning process of the learner by asking
appropriate questions. Structuring of long case, like in Objective
Structured Long Examination Record (OSLER)- may improve the reliability
of the long case, make it time efficient as well as impart it the
valuable formative feedback function [35].
6. Mini-Clinical Evaluation Exercise (mini-CEX)
This method involves observing the learner during an
actual clinical encounter. This exercise could be observed on an
out-patient, inpatient or in an emergency-room setting. The assessor
scores the performance of the learner on a standard scoring sheet
(global rating) containing items pertaining to seven core clinical
skills (medical interviewing, physical examination, professionalism,
clinical judgment, counseling, organization/ efficacy and overall
clinical competence) [36]. However all skills need not be assessed in a
single encounter. The assessor then provides an immediate and contextual
feedback. Scores of ‘clinical judgment’ are likely to reflect clinical
reasoning ability.
7. Portfolios
These are case logs maintained by the student along
with their reflective and narrative writing. They are able to offer rich
and authentic evidence of learners’ achievements and developments. When
used properly, they can be suitable for monitoring and assessing learner
competence and growth [29, 37].
Faculty Development
Faculty need to be sensitized about their role in
facilitating learning and promoting development of clinical reasoning
skills in students. Teachers need to consciously share their own
clinical problem solving approaches. This guides learners through the
developmental phases of this skill acquisition [38]. Additionally,
faculty development initiatives are needed to train teachers in
assessment of clinical reasoning skills and in giving effective
feedback. Designing and conducting assessment to test reasoning ability
requires a great deal of team work among experts.
Conclusions
Clinical reasoning skills are core competencies to be
acquired and demonstrated by every physician. Conscious and sustained
efforts are needed to encourage training medical graduates in the
acquisition of these crucial skills.
Contributors: TS: conceptualized the draft; JNM,
Anshu, TS: wrote the manuscript; PG: provided critical comments and
edited the manuscript.
Funding: None; Competing interests: None
stated.
References
1. Eva KW. What every teacher needs to know about
clinical reasoning. Med Educ. 2004;39:98-106.
2. Anderson KJ. Factors affecting the development of
undergraduate medical students’ clinical reasoning ability. PhD Thesis.
The University of Adelaide, 2006; 1-4.
3. Linn A, Khaw C, Kildea H, Tonkin A. Clinical
reasoning. A guide to improving teaching and practice. Aust Fam
Physician. 2012;41:18-20.
4. Elstein AS. Thinking about diagnostic thinking: a
30 year perspective. Adv Health Sci Educ Theory Pract. 2009;14:7-18.
5. Kassirer JP. Teaching clinical reasoning:
case-based and coached. Acad Med 2010;85:1118-24.
6. Norman G. Research in clinical reasoning: past
history and current trends. Med Educ. 2005;39:418-27.
7. Medical Council of India Regulations on Graduate
Medical Education 2012. Available from:
http://www.mciindia.org/tools/announcement/Revised_GME_2012.pdf .
Accessed October 2, 2014.
8. Graber ML. Educational strategies to reduce
diagnostic error: can you teach this stuff. Adv Health Sci Educ Theory
Pract. 2009;14:63-9.
9. Grant J, Anshu, Burch V, Zachariah A. Learning
clinical problem solving. FAIMER-Keele Master’s in Health Professions
Education: Accreditation and Assessment. Module 6, Unit 6. FAIMER Centre
for Distance Learning. London: CenMEDIC;2014.
10. Croskerry P. The theory and practice of clinical
decision making. Can J Anesth. 2005;52:R1-R8.
11. Pelaccia T, Tardif J, Emmanuel T, Charlin B. An
analysis of clinical reasoning through a recent and comprehensive
approach: the dual process theory. Medical Education Online. 2011;16.
Available from: www.ncbi.nlm. nih.gov/pmc/articles/PMC3060310/.
Accessed May18, 2015.
12. Norman G. Dual processing and diagnostic errors.
Adv Health Sci Educ Theory Pract. 2009;14:37-9.
13. Bowen JL. Educational strategies to promote
clinical diagnostic reasoning. N Engl J Med. 2006;355:2217-25.
14. Rencic J. Twelve tips for teaching clinical
reasoning. Med Teach. 2011;33:887–92.
15. Bordage G. Prototypes and semantic qualifiers:
From past to present. Med Educ. 2007;41:1117-21.
16. Woods NN. Science is fundamental: The role of
biomedical knowledge in clinical reasoning. Med Educ. 2007;41:1173-7.
17. Woods NN, Brooks LR, Norman GR. The role of
biomedical knowledge in diagnosis of difficult clinical cases. Adv
Health Sci Educ Theory Pract. 2007;12:417-26.
18. Wigton RS. Use of linear models to analyse
physicians’ decisions. Med Decis Making. 1988;8:241-52.
19. Custers EJFM. Thirty years of illness scripts:
Theoretical origins and practical applications. Med Teach. 2015;
37:457-62.
20. Bannister SL, Hanson JL, Maloney CG, Raszka WV.
Using the student case presentation to enhance diagnostic reasoning.
Pediatrics. 2011;128:211-3.
21. Wolpow T, Papp KK, Bordage G. Using SNAPPS to
facilitate the expression of clinical reasoning and uncertainties: a
randomized clinical trial. Acad Med. 2009;84:517-24.
22. Neher JO, Stevens NG. The one-minute preceptor:
Shaping the teaching conversation. Fam Med. 2003; 35:391-3.
23. Neher JO, Gordon KC, Meyer B, Stevens N. A
five-step "microskills" model of clinical teaching. J Am Board Fam
Pract.1992;5:419-24.
24. Gawande A. The Checklist Manifesto: How to Get
Things Right. New York: Henry Holt and Company; 2009.
25. Custers E, Boshuizen HPA, Schmidt HG. The role of
illness scripts in the development of medical diagnostic expertise:
Results from an interview study. Cognit Instruct. 1998;16:367-98.
26. Custers E, Boshuizen HPA, Schmidt HG. The
influence of medical expertise, case typicality, and illness script
component on case processing and disease probability estimates. Mem
Cognit. 1998;24:384-99.
27. Audetat MC, Laurin S, Sanche G, Beique C, Fon NC,
Balais JG, et al. Clinical reasoning difficulties: A taxonomy for
clinical teachers. Med Teach. 2013; 35:e984-9.
28. Dhaliwal G, Sharpe BA. Twelve tips for presenting
a clinical problem solving exercise. Med Teach. 2009;31:1056-9.
29. Joshi MK, Gupta P, Singh T. Portfolio-based
learning and assessment. Indian Pediatr. 2015;52:231-5.
30. Moulton CE, Regehr GE, Mylopoulos M, MacRae HM.
Slowing down when you should: A new model of expert judgment. Acad Med.
2007;82:S109-S116.
31. Ericsson KA. Deliberate practice and the
acquisition and maintenance of expert performance in medicine and
related domains. Acad Med. 1988;79:S1-S12.
32. Beullens J, Struyf E, van Damme B. Do extended
matching multiple-choice questions measure clinical reasoning? Med Educ.
2005;39:410-7.
33. Page G, Bordage G, Allen T. Developing
key-feature problems and examinations to assess clinical decision-making
skills. Acad Med. 1995;70:194–201.
34. Lubarsky, S, Dory V, Duggan P, Gagnon R, Charlin
B. Script concordance testing: From theory to practice: AMEE Guide No.
75. Med Teach. 2013;35:184-93.
35. Gleeson F. Assessment of clinical competence
using the objective structured long examination record (OSLER). Med
Teach.1997;19:7-14.
36. Norcini, JJ, Blank LL, Arnold GK, Kimbal HR. The
mini-CEX (clinical evaluation exercise): a preliminary investigation.
Ann Intern Med. 1995;123:795-9.
37. Driessen EW, Overeem K, van Tartwijk J, van der V
leuten CPM, Muijtjens AMM. Validity of portfolio assessment: which
qualities determine ratings? Med Educ. 2006;40:862-6.
38. Askew K, Manthey D, Mahler S. Clinical reasoning: Are we testing
what we are teaching? Med Educ. 2012;46:540-1.
|
|
|
 |
|

