From *Department of Preventive and Social
Medicine, B.J. Medical College, Ahmedabad 380 016, Gujarat, India.
Correspondence to: Dr. Kamlesh R. Lala, I,
Vastu Flats, Near S.B.I., Girdharnagar, Ahmedabad 380 004,
Gujarat, India. E-mail: [email protected]
Intramuscular injections (IM) are a common yet
complex technique used to deliver medication deep into the large
muscles of the body(l). However it is not a benign procedure and
unsafe injection practices are estimated to have significant impact on
patient morbidity and mortality. Unsafe injection practice results in
millions of dollars in direct medical costs on an annual basis(2).
Although there is significant research spanning over eight decades, on
the procedure and techniques of administering medications by the IM
route, instruction materials and clinician practice do not always
reflect research-based practice.
According to WHO, intramuscular injection is an
administration of medications parenterally through a skin puncture by
a syringe and a needle deep into a large muscle of the body for
prophylactic or curative purposes(3). Injections are among the most
frequently used medical procedures, with an estimated 12 billion
administered throughout the world on an annual basis. Of these 5% or
less are for immunization and rest are given for curative purposes,
many of which have been judged to be unnecessary(4). In India, a
survey found that 96% of all injections given by private doctors were
of antibiotics, vitamins and analgesics(5). A conservative estimate of
the average number of injection ranged from 0.9 to 8.5 per person per
year, with a median of 1.5 injections per person per year(2).
Giving an IM injection is not a benign procedure:
the complications reported are muscle fibrosis and contracture,
abscess at the injection site, gangrene and nerve injury. Unsafe
injection practice may result in number of infections, particularly
hepatitis B and C and HIV(6-8). Ironically, even though IM injections
are known to have iatrogenic complications, healthcare providers are
not imparted proper education(9). It has been found that techniques
used by nurses in giving IM injections were "little more than a
ritualistic practice, one based on tradition, which passes from one
nurse to another and from one generation to the next". This happens
inspite of the fact that there is a vast body of research extending
back to 1920s regarding injection sites, blood flow and absorption in
various muscle groups, discomfort, positioning, administration
techniques and complications. Even today this is the area of study
that continues to be of interest to nursing researchers(l). Until the
introduction of antibiotics-penicillin in the late 1940s, the
administration by IM route was a skill that was almost exclusively
practiced by physicians. By the late 1960s, IM injections were
routinely administered by nurses(10). This was the period when glass
syringes were being replaced with disposable plastic syringes and
needles in USA.
The Goal
Administering an IM injection is a complex
psychomotor task that requires skill and knowledge on the part of the
clinician who is performing the procedure. Our goal is to maximize the
therapeutic effect of the medica-tion, eliminate or minimize the
complications and discomfort from IM injection. In addition to being
able to physically perform the skill, the clinician needs knowledge of
pharma-cology, anatomy, physiology, physics and microbiology along
with legal and ethical issues.
The first decision that must be made before any IM
injection is whether it is necessary and justified. According to WHO,
"An injection should only be given if it is necessary and each
injection that is given must be safe"(11). Once the decision has been
made that based on medication and patient characteristics an IM
injection is justified, the second decision is to determine the site
for injection(12,13). The site selection is critically important
because (i) the medication effect can be enhanced or diminished
depending on the site of injection (ii) complications like
muscle contracture and nerve injury are site dependent, (iii)
site varies depending upon the age of the patient, and (iv)
vaccines are never administered in gluteal area even in children, as
gluteal fat retards absorption and so affects the antibody titers.
Site Selection
Anterolateral thigh: The anterolateral thigh is
the preferred site of injection for infants less than 12 months and
sometimes in children above 2 years also. Here the target muscle is
vastus lateralis (VL), which is part of the quadriceps femoris. This
muscle is well developed at birth(13). The site is antero-lateraly in
the middle third of the portion between greater trochanter and lateral
femoral condyle (Fig. 1). Damage to femoral nerve or artery can
be prevented by assiduously selecting the site and using needle with
proper length. Rectus femoris muscle which is anterior on the thigh
should not be used.
Fig. 1. Injection site for anterolateral
thigh(14).
Deltoid: Though the deltoid muscle is small,
this site is adequate for low volume injection. For toddlers and older
children deltoid may be used only if muscle mass is adequate. It is a
triangular muscle that originates from the lateral one third of the
clavicle, the acromian and the scapular spine and converges into the
deltoid tuberosity near middle of the humerus. The site should be
selected 3-5 cm below the bony landmark of acromian process or midway
between acromian process and deltoid insertion(13,15) (Fig. 2).
In younger children the layer of subcutaneous (SC) tissue over the
deltoid muscle is fairly consistent i.e., approximately 4.9 mm
regardless of weight(17). This site has potential for injury to (i)
axillary nerve beneath the deltoid at surgical head of humerus, (ii)
axillary nerve and posterior circumflex humeral vessels near deltoid
tuberosity of humerus near insertion of deltoid and (iii)
radial nerve under scapular portion of deltoid muscle if the injection
is placed posteriorly and inferiorly.
Fig. 2. Injection site for deltoid(16).
The radial, brachial and ulnar nerves and profunda
brachii artery are under the triceps muscle. So this muscle is not
used for injection(13).
Gluteal: It may be dorsogluteal (DG) or
ventrogluteal (VG) (Fig. 3). This is a preferred site for
injection volume 2-5 mL, oily, painful and irritating injections and
depot medications. The target muscle for DG injection is gluteus
maximus. This muscle does not develop in size until child has been
walking for a period of time. So this is not a preferred site(13). The
target muscle for VG injection is gluteus medius. This muscle has a
large mass, is well developed in young children and adults and is
relatively free from major nerves and vessels. Subcutaneous layer over
the muscle is uniform in thickness irrespective of patient’s
weight(8).
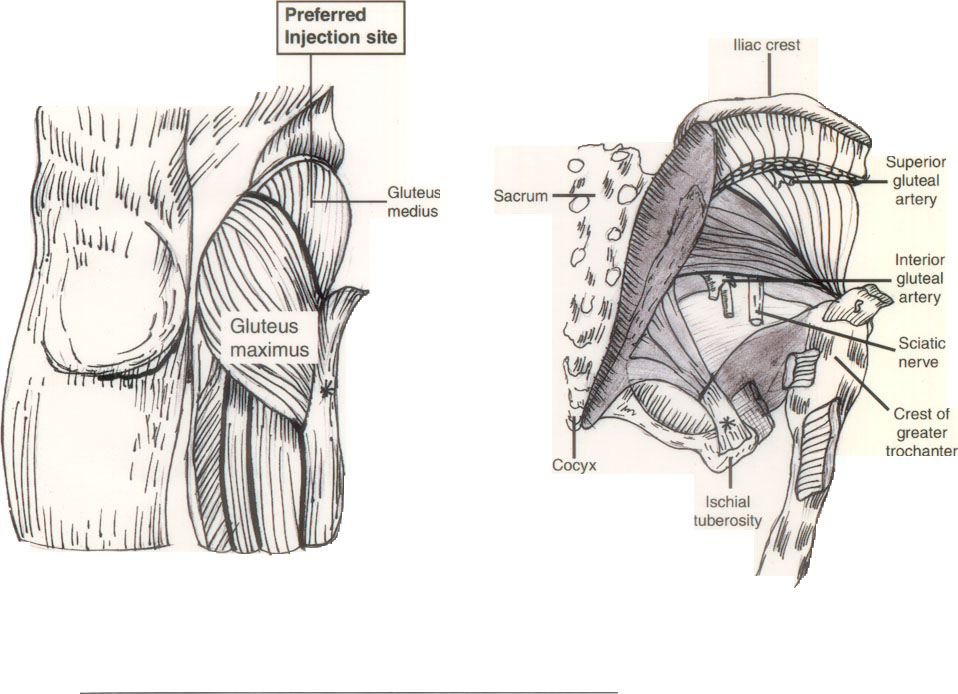
Fig. 3. Injection sites for gluteal region. Also
shows relation of nerves and vessels with potentiality of injury(14).
There are various methods suggested to identify the
site(1,18).
(i) The area is bounded by the iliac
crest, and by intersecting lines drawn from the upper end of the
gluteal cleft to the anterior superior iliac spine and from ischial
tuberosity to the uppermost part of the iliac crest respectively (Fig.
4). Only the upper outer quadrant area of this imaginary cross
is used for injection site. If going high, then there is potential
to hit the bone. If the site is chosen too close to the center, then
there is potential of injuring greater or lesser sciatic nerves.
Also this imaginary cross leaves too much margin of error as it may
change with the position of the patient. The injection would be most
of the time into gluteus maximus.
Fig. 4. Methods for identification of injection
site at gluteal region(19).
(ii) The simpler method to identify the
injection site is: spread the palm of the opposite hand flat against
the greater trochanter. Index finger is placed on the anterior
superior iliac spine and middle finger extended along the iliac
crest towards the iliac tubercle, the gluteus medius muscle "pops"
up between the fingers (Fig. 4).
(iii) Draw an imaginary line between the
posterior iliac spine and the greater trochanter of the femur.
Injections are given in an area lateral and superior to this
imaginary line and most of the time the injection would be into
either the upper outer mass of the gluteus maximus or into the
gluteus medius.
Preparation of Injection
Though some of the vaccines and medications are
available in prefilled syringes, some are not. So here apart from site
selection, size of the syringe, length and gauge of needle are to be
selected. Ensure ‘Universal Precautions’ as laid down by WHO before
any injection(20). Alcohol based hand rubs are more convenient and
effective than soap and water if there is no dirt and mess.
Equipment: Use only new disposable syringe and
needle every time. WHO recommends that auto disable syringe is the
preferred type of disposable equipment for administering vaccines and
the equipment of choice for conducting mass immunization campaign(21).
Withdrawing medication: Safest practice is to
withdraw medication by using filter needle and change it before
injection. It is believed to prevent particulate matter such as glass
or rubber particles from being withdrawn into the syringe. If same
needle is used then there is a fear that needle may be bent or dulled.
But both the above points are theoretical and there are no research
evidences to support either positive or negative claims(22,23). It is
not recommended for immunization because of cost and use of higher
gauge needle(24).
Air Bubble: Though it is a topic of heated
debate, it has been proved to be outdated and non-scientifically
recommended procedure and should be eliminated from IM injection
procedure(15,18,25). There were two thoughts: (a) It ensures
correct dose taking into consideration of dead space. But disposable
syringes are calibrated taking into account of medication within
syringe hub and needle. Some syringes are available with projection on
the plunger, which enters the hub after finishing of pushing the
medication. (b) Air bubble seals the medication in the muscle
after injection and prevents backflow of medication through needle
track. This later problem can be eliminated by using Z track
technique(26,27). Skin is pulled downwards and laterally before
injection. This displaces the skin and SC tissue leaving the muscle
there only and uses the valve action to prevent leakage of medication
into the SC tissue (Fig. 5).
Fig. 5. Z-track technique for IM injection(19).
Wiping the needle: Excess medication is
expelled through the needle. Medication dripped on the needle should
be wiped off as it can cause pain if tracked through SC tissue. Do not
use alcohol swab to wipe the needle, as it is irritant. Cotton swab
also should not be used as some cotton fibres may be left over on the
needle. So use only dry gauze pad(28,29).
Needle length and gauge: The selection of
length of the needle depends upon the age of the child, the size of
the muscle and SC mass over the muscle. For VL needles of 16 mm, 22 mm
or 25 mm, for deltoid 16 to 32 mm and for VG 25 to 38 mm length are
used. It has been found that longer needle with the same gauge was
associated with significant reduction in redness and swelling
following routine immunisation(30). It is because medication is sure
in the muscle. For general biologicals and medications in aqueous
solution, 23 g to 27 g and for viscous and oil based medication, 18 g
to 23 g needle is used. Using higher gauge (thinner) needle may cause
more trauma because they have a narrow bore producing a jet under
higher pressure. So for immunisation 23 g needle is preferred over 25
g(30).
Procedure
1. Positioning
Proper positioning allows clinician to identify the
site correctly and ensures patient comfort by relaxing the muscles.
Expose the part completely.
(i) For deltoid: The patient may
sit or stand. Child may be held in an adult’s lap. Placing the hand
on the hip will relax the deltoid muscle(l).
(ii) For VL: To position the child
for left VL, the adult’s left arm should be around the child,
supporting the head and holding the outside arm. The child’s inside
arm should be tucked around the adult’s body. The adult’s right hand
should firmly hold the child’s legs(11).
(iii) For VG: The position may be
sitting, standing or lying in supine or lateral. But having patient
lay down is the safest position. Internal rotation of femur relaxes
the gluteal muscle. In a lateral position, the upper leg can be
flexed at 20º to ensure internal rotation. Flexing one or both knees
will relax the muscle in a supine position(28).
2. Cleansing
Once the patient has been positioned, the muscles
relaxed and. the site properly identified by using bony landmarks, the
site is cleaned properly avoiding the site where skin is obviously
infected. There are several thoughts and hypothesis regarding
cleansing of the site. In a study it was found that the rate of
infection was so low as to be non existent and so routine disinfection
of the skin is not necessary, provided patient is physically clean and
proper hygiene and asepsis are observed during the procedure(31,32).
Since our goal is cleansing and not disinfection, if the intended
vaccination site is visibly dirty, obvious dirt can be removed using
clean water, water for injection or saline and a clean tissue, cloth,
cotton wool, gauze or other such non-impregnated material. Wipes that
are impregnated with medicated chemical must not be used. Such
chemicals may interfere with the vaccines, especially live ones(33).
There is a thought against this also. Most of the clinical trials in
US evaluating the efficacy of vaccines are done wiping the injection
site without evidence of inactivity(34). Hence we should not
generalize the either recommendation on cleansing. In our setting it
is better to clean the area with single use alcohol wipes in a
circular fashion in an area approx. 5-8 cm and is allowed to dry. Pre
wetted cotton swabs are avoided for fear of contamination(34).
3. Technique
One method of insertion of the needle is known as
US method and is promulgated by ACIP(12,13,33). The clinician uses his
non dominant hand to bunch the muscle and direct the needle inferiorly
along the long axis of leg at an angle appropriate to reach the
muscle, usually 45º. This method stabilizes the leg and increases the
muscle mass. In the second method, recommended by WHO(11), the skin is
stretched flat between the index finger and thumb and the needle is
pushed down at 90º. Both these methods are worthy of further
discussion and investigation(31).
4. Methods for alleviating discomfort
Comfort measures and distraction techniques (e.g.,
playing music or blowing toys) might help children cope with injection
discomfort. Pretreatment with 5% topical lignocaine before 30-60 min.
of injection can decrease pain and it has been shown not to interfere
with immune response(24). Administering sweet tasting fluid (2 mL of
20% w/v sucrose solution or mother’s milk -EBM) immediately before
injection can result in a calming or analgesic effect(24,35,36).
Applying pressure to the site for about 10 sec prior to injection
would reduce injection pain.
An interesting piece of anecdotal evidence suggests
an alternate method(37). Place the needle point on the skin and if
there is no pain at the initial point of contact, push the needle. If
there is pain, the needle is moved over 2-3 mm at a time until a
painless point on the skin is found, at which point the needle is then
inserted. This is based on the anatomy of cutaneous innervations
providing distinct points without pain receptors and hence no pain
sensation. This technique is used by neurologists for EMG studies. But
these methods to reduce discomfort seem to warrant further research.
5. Insertion of the Needle
Ensure smooth and steady insertion of the needle
with a dart technique. Though routine recommendations over the years
has been to insert the needle at 90º, with angles ranging 72º-90º, the
injection is in the muscles as opposed to SC tissue.
6. Aspiration (Before pushing medication)
Aspirate by pulling back the plunger for 5-10 sec
to ensure that the needle is not in low flowing blood vessel. If blood
is aspirated in the syringe, withdraw the needle and discard the
syringe with medication. There are thoughts against this: (i)
This is not possible while using AD syringe. (ii) Large blood
vessels are not located around the recom-mended injection sites. (iii)
Understanding the anatomy of injection sites and using appropriate
landmarks prevent injury to vessels. (iv) All of the
complications in the literature of intra-arterial injection involved
penicillin and similar medications and not vaccines. It is safe to
assume that immunization as a class of IM injection poses less risk to
the patient than other medications particularly antibiotics(1,31,33).
The disadvantages of the aspiration procedure are:
it prolongs the time the needle is inserted into the patient, may
result in loss of control of the syringe if both hands are used and
may cause trauma at the site of injection. But because of lack of
sufficient evidences against aspiration also, WHO is neither able to
support nor offering alternative action and recommends to make locally
appropriate choices keeping in mind the risk associated with a "blind
injection"(33). After introduction of AD syringes in immunization, we
at least do have substantial field experience that injection with EPI
vaccines into standard sites have no reports of adverse events(34).
According to ACIP, no data exist to document the necessity of
aspiration during immunization(24). So we can conclude that aspiration
is not necessary during immunization and care is to be taken with
injections other than vaccines.
7. Pushing the medication
Inject the medication at the rate of 1 mL per ten
sec. This slow pushing allows muscle fibers to stretch and accommodate
the injected volume while lessening the chances of leakage back
through needle track. Once the syringe has been emptied of medication,
wait for 10 sec before withdrawing the needle. Withdraw the needle
with a smooth and steady movement and apply gentle pressure with a dry
gauge. Use of alcohol or spirit swab may cause burning sensation(1).
8. Multiple Injections
If more than one injection is to be administered
simultaneously, it is preferable to administer each at a different
anatomical site. If it is not possible then the thigh is usually a
preferred site and two injections are sufficiently (1"-2")
separated(24).
9. Post Injection
Post injection syncope is a known side effect
especially in adults and adolescents and so it is better to observe
the patient for 10-15 min after injection(38). Instruction is given
for proper self-management with paracetamol like drugs for local pain
and fever. All equipments used for injection are to be disposed of
safely.
Conclusion
Based on this review, a research based guideline
for practice has been developed (Table I). Use of these
guidelines along with clinical judgment can assist the clinician to
ensure that the practice of IM injection is evidence based.
Contributors: KRL provided the framework and
concept of the article and reviewed the literature. KRL and MKL
drafted the paper. MKL was responsible for critical appraisal. She
will act as the guarantor of the paper.
Funding: None.
Competing interest: None stated.
Table I
Clinical Practice Guidelines:
Intramuscular Injection Guidelines for Evidence Based Technique
|
Patient Population:
Infants, toddlers, children and adults receiving medication by IM
route for curative or prophylactic purpose.
Objective:
Administration of medication to maximize the therapeutic effect for
the patient and minimize or eliminate patient injury and discomfort
associated with procedure.
Key points:
An injection should be given if it is necessary and each one is safe
as per WHO justification for IM injection. Consider:
• Medication characteristics
including formulation, onset and intensity of effect, duration of
effect*
• Patient characteristics
including compliance, uncooperativeness, reluctance, inability to
take by another route*
Site Selection:
It is single most consistent factor associated with complications and
injury. Always use bony landmarks to properly identify the site.*
Consider:
Age of patient:
• Infants: Vastus
lateralis is the preferred site*
• Toddlers and children:
Vastus lateralis or deltoid*
• Adults: VG or deltoid*
Medication type:
• Biologicals including immune
globulins, vaccines and toxoids: VL in
infants and young children or deltoid in older children and
adults*
• Irritating, viscous or oily
solution and depot formulations: VG*
Medication volume:
• Volumes 2 mL or less in
deltoid* and larger volumes of 2-5 mL in VG*
Preparation of injection:
Consider:
Equipment
(a) Needle Length
corresponds to the site, age of patient and muscle mass. Use longer
possible needle
¶§
• VL ® 16mm to 25 mm*
• Deltoid for children ®16 mm to
25 mm and for adults – 25 mm to 38 mm*
• VG (Adults) ® 38 mm*
(b) Needle gauge often
dependent on needle length. In general for most biologicals and
aqueous solutions 23-27 g and for oil based medication 18-23 g @
• Use 23 g needle for
immunization ¶§
• Always use a new sterile
syringe and needle for every injection*
• Use the markings on the
syringe barrel to ‘determine the correct dose*
• Do not include air bubble in
the syringe*
Patient preparation and positioning:
Consider site of injection
• Deltoid: patient may sit or
stand. A child may be held in adult’s lap*
• VG: patient may stand, sit or
lay laterally or supine*
• VL: Infants and young children
may lay supine or be held in adult’s lap*
• Remove clothing at the site
for adequate visualization and palpation of bony landmarks@
• Position patient to relax the
muscle*
Injection Procedure:
• Cleanse the site with alcohol
wipes and allow it to dry. If cleanliness and asepsis are,
observed, routine skin disinfection is not necessary @ ¶§
• Insert the needle into the
muscle using a smooth and steady motion @
• Though US technique is
preferable, both US and WHO methods are worthy of further
discussion and investigation ¶
• Research on two alternate
techniques to reduce pain at the moment of injection is
inconclusive at this time, but warrants further study ¶§
• No need for aspiration in
immunization, otherwise understand the anatomy of injection site
and take care to minimize injury with blind injection@ §
• Inject slowly at the rate of 1
mL/10 sec @
• After injection, wait for 10
sec before withdrawing the needle @
• Withdraw the needle slowly,
apply gentle pressure with a dry gauge @
Post injection:
• Observe the patient for 10-15
minutes*
• Assess site for complication,
both immediately and 2-4 hours later, if possible
• Instruct patient regarding
assessment, self-management of minor reactions and when to report
more serious problems*
• Properly and promptly dispose
of all equipments
|
Note: Needle sizes are: 16 mm = 5/8", 22 mm
= 7/8", 25 mm = 1", 32 mm = 11/4", 38 mm = 1/2"
Criteria for grading of the evidence:
*Empirical data from published research reports, recommendations of
established advisory panels, and generally accepted scientific
principles; @ Surveys, reviews, consensus among clinicians and expert
opinion; ¶ Published case reports; § Anecdotal evidence and letters.
