As I write this, WHO has declared the Spring 2003
severe acute respiratory syndrome (SARS) epidemic to be defeated in all
countries, with a warning that it may return unless vigilance is
maintained (http://www. who.int/csr/sars/country/2003_07_09/en/). In
about six months, SARS killed some 800 people and caused economic
devastation, mostly in Eastern Asia. India avoided most of the problem
by having only 3 cases and no deaths. Over the same period, however,
another rapidly acting pneumonia, what might be called old SARS, killed
nearly 2.0 million people around the world. India suffers from Old SARS
more than any other nation. Indeed, a hundred people die of Old SARS
every hour in India, making the entire global New SARS epidemic equal to
less than a half day’s toll of Old SARS in India.
Old SARS, of course, is commonly known as "acute
respiratory infection", the chief source of childhood morbidity around
the world. As acute lower respiratory infection (ALRI-mainly pneumonia),
it kills more children than any other disease making it also the chief
cause of lost life-years in the world(1). In South Asia, it is
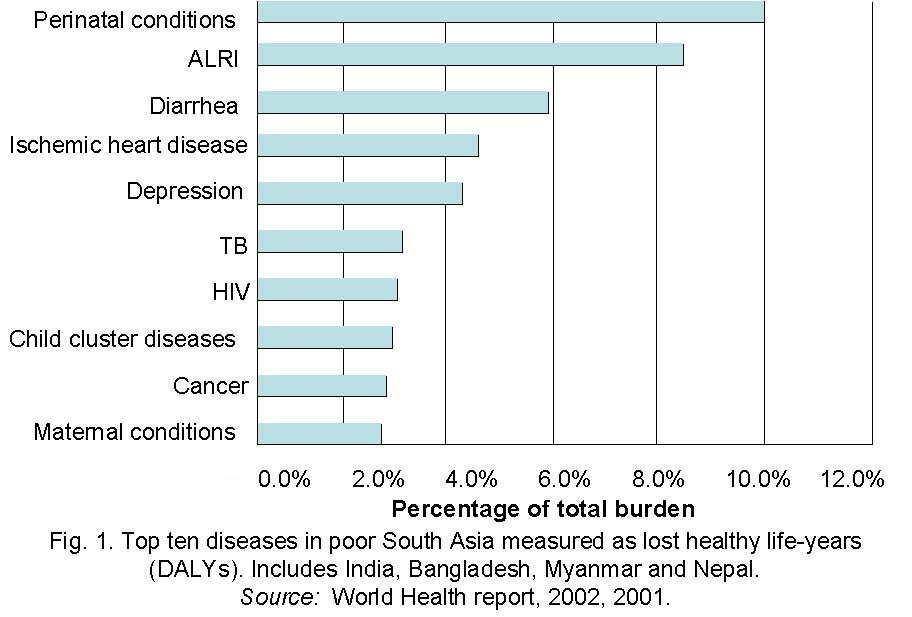
responsible for more than 8% of the burden of disease (Fig 1).
ALRI in Indian children under 5 (one disease, one country, one age
group) is responsible for 1.5% of the entire global burden of disease.
Unlike New SARS, of course, ALRI normally does not
threaten healthy adults. Businessmen who until recently were afraid to
fly to Hong Kong, for example, can walk through the slums of Kolkata,
without fear of catching it. Thus, it does not make the news, affect the
economy, or trigger emergency worldwide action. Nevertheless, it exacts
a terrible toll.
The chief risk factor for ALRI mortality might be
said to be poverty. After all, young children allover the world
apparently contract ARI at about the same rate, but only the poor ones
die of it. Although accurate, however, it is not also true that poverty
alleviation is the best intervention. As with other major
poverty-related diseases, we know ways to make people healthy before
they become wealthy. In the case of ALRI, promotion of breast feeding;
vaccination for Hib and measles; nutrition supplements for babies and
pregnant women, and case-management with antibiotics have been shown to
be effective means to reduce mortality in India and elsewhere(2).
Studies of ALRI risk factors in currently poor
countries and historical analyses of the decline of pneumonia rates in
currently rich countries argue for modification of important environment
risk factor. These factors seem to operate through housing, ventilation,
crowding, drainage, and chilling, As housing improved in the past, ALRI
rates went down, well before vaccines and antibiotics came along. It has
been difficult, however, to quantify the contribution of individual
housing risk factors or separate them from nutritional and other factors
until recently.
In the last decade or so, many studies have been done
showing a relationship of household indoor air pollution and various
types of ill-health in women and children(3), These studies have focused
on households using solid fuels for cooking and heating because these
fuels produce rather large amounts of toxic air pollutants in simple
household stoves(4). When used in unvented stoves (no chimney or flue),
the resulting indoor air pollution levels for small particles (the best
indicator of the hazard of combustion-generated air pollution) are above
national standards or WHO guide-lines and higher than outdoor air
pollution in even the worst hit cities. Typical 24 h levels in north
Indian villages for particles less than 10 microns (inhalable into the
deeper respiratory system) are 400-1000 µg/m3(5) compared to 100-200
µg/m3 in cities(6). Levels are lower in south India, where houses are
better ventilated, but still rival those in the worst cities(7).The
total pollution exposure in the country is quite high due to the
ubiquity of solid fuel use in households. Some 75% rely on them, mostly
in the form of biomass (wood, dung, crop residues). A few percent,
mainly in West Bengal, use coal, which, depending on quality, can
produce even worse pollution than biomass(8).
Compared to other forms of air pollution, indoor air
pollution from solid fuel use has been investigated less for health
effects. During the 1990s, a number of observational studies of ALRI
risk from use of solid fuels in developing countries households around
the world were done(9). A meta-analysis of these studies found an odds
ratio of about 2.3(10). Two Indian hospital based case-control studies
not included in this meta-analysis also found high risk. In a Delhi
study, the authors report an odds ratio of 2.5 (CI: 1.5-4.2) for cooking
with fuels other than LPG(11). Unlike other indicators of socio-economic
status, such as housing material (thatch or not) and floor type (cement
or not), which were significant in the bivariate but not in the
multivariate analysis, fuel type remained significant after adjustment
for a range of socio-economic confounders. In a Kolkata study, adjusted
multivariate analysis found an odds ratio of 4.0 (CI: 2.0-7.9) for
cooking with wood and/or cowdung(12).
Given India’s high prevalence of exposure, if an odds
ratio of 2-3 were to accurately describe the impact of solid fuel use on
mortality as well as morbidity (such studies cannot evaluate mortality
risks directly), the attributable burden of ALRI due to indoor air
pollution in India would be immense. A calculation of this sort was done
for the Comparative Risk Assessment study of WHO, summarized in the 2002
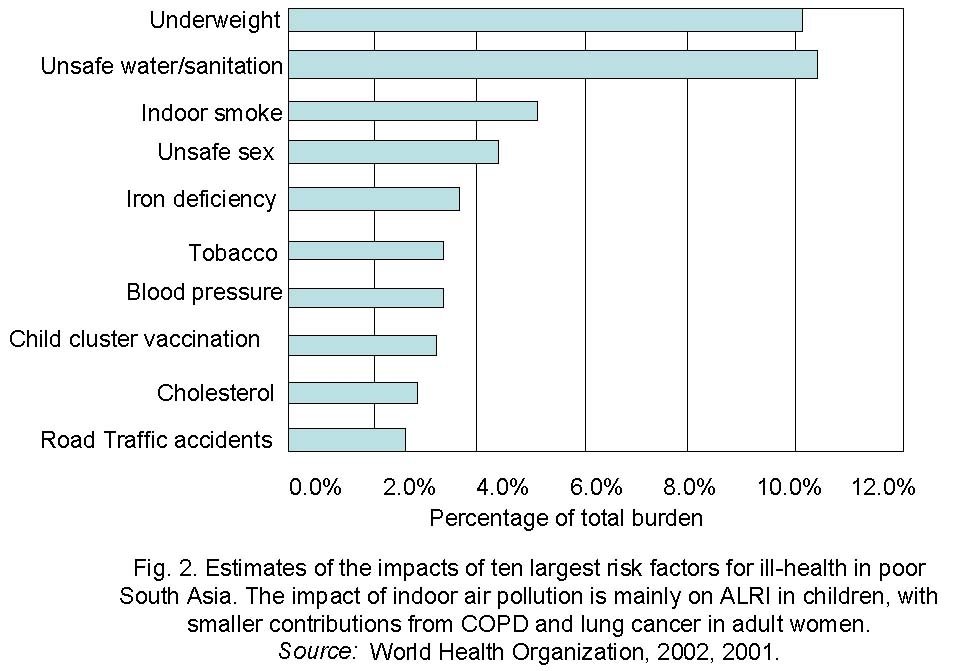
World Health Report(10). As shown in Fig. 2, indoor air pollution
ranks third among all major risk factors in the region, only being
exceeded by malnutrition and unsafe water or sanitation(1).
The number and consistency of the observational
studies in solid-fuel using households and the associated information
from ETS and outdoor air pollution studies as well as laboratory tests
with animals provide good evidence for a causative effect of indoor air
pollution on ALRI. Probably the pollutants act through suppression of
the immune system and other respiratory protective mechanisms. In
developed countries with large government public health budgets, this
evidence would be more than sufficient for action. Ironically, however,
in poor countries such as India there is need for even stronger evidence
before action can be undertaken on a large scale. Because of the small
amount of funds available for public health interventions - less than $5
per year per capita in India, for example, compared to $1800 in the
USA(13) competition is fierce. A proposal for shifting these funds must
show evidence of the highest quality to make a convincing case(2).
However, observational epidemiologic studies only provide limited
evidence of causality because of inherent biases in the study designs.
The gold standard both for showing causality and for
showing what an actual intervention can achieve in the real world is a
randomized intervention trial. Although full blinding and placebo
controls are difficult to undertake with environmental studies, it is
possible to conduct randomized trials for household interventions, such
as improved fuels, stoves, or ventilation. Calls for such trials have
been made since the 1980s in order to pin down the causality and scale
of indoor air pollution and ALRI sufficiently to convince policy makers
and donors to invest in intervention(14). To date, however, only one
such trial has been funded in the world, which is ongoing in Central
America (see http://ehs.sph.berkeley.edu/guat/default.htm).
Environmental interventions often have significant
non-health as well as health benefits. Provision of clean water and
sanitation near households is an example where benefits in the form of
time-savings can be significant. If such benefits are not included in
the policy analysis, the optimum investment in clean water can be
underestimated. In the case of clean fuel or efficient stoves with
chimneys, there can also be significant benefits in the form of time and
fuel savings, as well as reduced pressure on forests in some areas.
Thus, a full understanding of the social benefits of these clean air
interventions requires consideration of these non-health benefits as
well. Unfortunately, however, it is difficult to find a government
agency or private donor that has interests across such a wide range of
benefits. Health ministries want health benefits; development agencies
want economic benefits; and environmental donors look for ecological
benefits. Thus, para-doxically, those interventions that ought to
receive special attention because they offer benefits of varying kinds
end up being penalized because they look less cost-effective at
producing any one benefits compared to narrowly targeted interventions.
In the case of ALRI, for example, antibiotics in some studies
cost-effectively stop babies from dying, but they do little else of
benefit and, indeed, will cause problems over time. They do not even
change incidence, only severity. Even though improved stoves are
unlikely to compete in this narrow calculation on ALRI mortality, they
not only offer important non-health benefits, but potentially a range of
smaller but still quite significant health benefits in the form of lower
disease rates for women and other family members exposed to smoke. High
quality integrated analysis of well-conducted intervention trials will
be needed to pin down the overall benefits of clean air for India’s
children and their families.
Kirk R. Smith,
Professor and Division Chair,
Environmental Health Sciences,
Maxwell Endowed Chair in Public Health,
School of Public Health, Warren Hall 7360
University of California, Berkeley 94720
E-mail:
[email protected]
