|
|
|
Indian Pediatr 2016;53: 933-934 |
 |
Bystander Cardio-Pulmonary Resuscitation Saves
Life in a Patient with Short QT Syndrome
|
|
*Pradeep Kumar Sharma and
#Neeraj Awasthy
*Pediatric Critical Care and Pulmonology, Sri Balaji
Action Medical Institute; and #Pediatric Cardiology,
Max Super Specialty Hospital, Saket; New Delhi, India.
Email: [email protected]
|
|
The short QT syndrome (SQTS) is a primary cardiac electrical disease
characterized by abnormally short QT intervals and an increased
propensity to develop arrhythmias. It is a relatively recent addition to
the list of inherited channelopathies responsible for sudden cardiac
death (SCD). Gussak, et al. [1] first described SQTS in 2000, and
about 70 cases are reported till now.
A 10-year-old boy, resident of Delhi, suddenly fell
unconscious, was not responding, not breathing and quickly turned blue
and cold at home. His uncle, an officer with city police, was trained to
carry out cardio-pulmonary resuscitation (CPR). He immediately started
CPR, and approximately after 7 cycles of CPR, child was revived. At
arrival to our hospital, he was stable with normal vital signs and
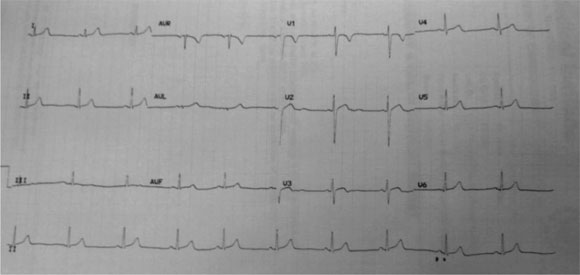
consciousness. ECG done revealed QT/QTc interval of 280ms/305ms. His
electrolytes, magnetic resonance imaging brain, electro-encephalography
and thyroid profile were normal. Repeat ECG at heart rate of 60 revealed
QT interval 280ms and J point to T-wave peak interval of 200ms (Fig.
1). Family history was negative for SCD. We placed an implantable
Cardio-defibrillator (ICD).
 |
|
Fig. 1 ECG done at HR-60/min showing QT
interval of 280ms.
|
A short QT interval is usually considered if QTc is
<340ms. However, there is an overlapping range of QT intervals between
affected individuals and apparently healthy subjects. Gollob, et al.
[2] proposed a diagnostic criterion for SQTS. SQTS is mostly seen in
males and common presentation is aborted SCD (24-32%), arrhythmias and
syncope [3]. As the risk of SCD is high in SQTS, ICD placement is
strongly recommended for secondary prevention. However, role of ICD in
primary prevention is not well defined. Information regarding
pharmacological therapy for SQTS is fairly limited, and quinidine has
been suggested as one of the therapies. SQTS is considered a rare
electrical abnormality associated with SCD in individuals with
structurally normal heart. Timely diagnosis and optimal treatment can
significantly improve the overall prognosis of the patient and family
members. There is a scarcity of data about SQTS in terms of its clinical
presentation, diagnosis, genotype-phenotype correlation,
risk-stratification and treatment. This case aptly highlights the
importance of bystander CPR in saving life in such disorders. Basic life
support education should be promoted widely to save many more lives.
References
1. Gussak I, Brugada P, Brugada J, Wright RS, Kopecky
SL, Chaitman BR, et al. Idiopathic short QT interval: a new
clinical syndrome? Cardiology. 2000;94:99 -102.
2. Gollob MH, Redpath CJ, Roberts JD. The short QT
syndrome: Proposed diagnostic criteria. J Am Coll Cardiol.
2011;57:802-12.
3. Villafañe J, Atallah J, Gollob MH, Maury P, Wolpert C, Gebauer R, et
al. Long-term follow-up of a pediatric cohort with short QT
syndrome. J Am Coll Cardiol. 2013;61:1183-91.
|
|
|
 |
|

