|
|
|
Indian Pediatr 2016;53: 924-926 |
 |
Etiology and Short-term
Outcome of First Seizure in Hospitalized Infants
|
|
Niraj Kumar Nikunj, *Devendra Mishra, Monica Juneja and
#Bibek Talukdar
Departments of Pediatrics, Maulana Azad Medical College
and associated Lok Nayak Hospital, and #Chacha Nehru
Hospital; Delhi, India.
Email: drdmishra@gmail.com
|
|
We enrolled 75 consecutive infants
presenting with history of first seizure at a tertiary-care hospital in
New Delhi, India. Clinical and biochemical work-up for etiology, and
electroencephalography were performed in all infants. Developmental
assessment was done 3-month after discharge. 72% had generalized
seizures, and fever was the commonest co-morbidity (57.3%). 68% had
provoked seizures, mainly due to hypocalcemia (34.3%) or neuro-infections
(29.3%). Seven (9.3%) infants died during hospital stay; mostly those
with neuro-infections. 13 (20.3%) infants had developmental delay.
Keywords: Child; Cause; Epilepsy; Prognosis.
|
|
A seizure is one of the commonest childhood
neurological illnesses and the risk is the highest in the first year of
life [1]. Even after four decades of the initial studies on etiology and
outcome of first seizure in infants [1], not much information is
available on this aspect from India [2,3]. This descriptive study was
conducted from April 2012 to March 2013 in the Pediatrics department of
a public hospital to describe the clinico-etiolgical profile and
short-term outcome of first seizure in infants.
After Institutional Ethical board’s clearance,
consecutive infants (aged 4-52 weeks) presenting with seizures (on three
pre-specified days per week) were admitted in the department and
evaluated for inclusion after initial management and stabilization. A
written informed consent was obtained from parents. Inclusion criteria
were: history of first episode of seizure, or history of more than one
seizure (within last 7 days) but not evaluated. Infants who had received
any medication (other than anti-convulsants) prior to coming to the
hospital, and infants with no documentation of treatment received for
the seizure, were excluded. Prospective enrolment continued till a
pre-decided sample size of convenience of 75 infants was achieved.
Detailed neurological history including details of
each episode of seizure was obtained from the parents, primary caregiver
or any additional person who had observed the seizure. Based on the
history, seizure semiology was classified for those not having any
seizure observed by a health worker. If the child had further seizures
during the hospital stay, the attending doctor classified the seizure
semiology, as per ILAE classification, 1981 [4]. All infants enrolled in
the study were treated using standard treatment protocol of the unit. In
brief, the protocol included essential investigations at time of
admission for all infants: blood glucose, serum calcium and
electrolytes, Serum urea/creatinine, and complete blood count.
Additional investigations were also done as guided by history and
physical examination and as per standard recommen-dations [5]. EEG was
done at least two weeks after discharge with a 32 channel digital video
EEG using International 10-20 system of electrode placement.
Neuroimaging, and work-up for inborn errors of metabolism were done as
required.
The presumed etiology of seizure was ascribed based
on the history, clinical findings and investigation results, as Provoked
seizures (occurring in close temporal relationship with an acute CNS
insult, which may be metabolic, toxic, structural, infectious, or due to
inflammation), Unprovoked seizures (occurring in the absence of a
potentially responsible clinical condition), and Febrile seizures, using
standard criteria [4,6,7].
All patients were kept in contact through monthly OPD
visits or telephonically, and neurodevelopmental assess-ment was done by
Developmental Assessment Scale for Indian Infants (DASII) three months
(±1 week) after discharge, by a single examiner. Data were analyzed
using SPSS 17.0 software. Comparisons between groups were done using
Chi-square test for discrete variables and Student’s t-test for
continuous variables.
 |
|
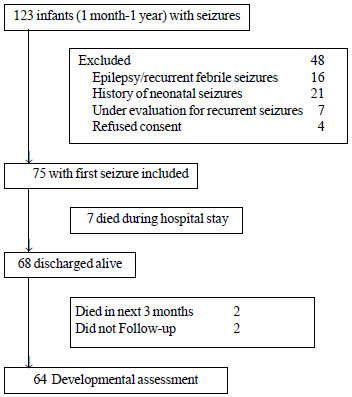
Fig.1 Flow of participants in the
study.
|
75 infants (61.3% males) with mean (SD) age of 5.8
(3.4) months were finally enrolled (Fig. 1).
Seizure was the only complaint in 42.7%, and fever (57.3%) was the
commonest co-morbidity. Solitary seizure was the presentation in 57
(76%) infants, and 12 (16%) had more than one seizure in previous 24
hours; seizure recurrence during hospital stay occurred in 7 (9.3%)
infants. and (93.3%) had a short-lasting seizure (<15 min). Seizure
semiology was determined based on eye-witness account in 77.3% and
observation of seizures by a pediatrician in the rest. Majority (72%)
had generalized seizure (tonic in most), though 7 (9.3%) had
unclassified seizures. 68% of the infants had provoked seizures, mainly
due to hypocalcemia and neuro-infections. All patients with hypocalcemia
had nutritional rickets. Of the febrile seizures, a quarter presented
with febrile status epilepticus (Table I). Thirteen
(20.3%) infants had developmental delay, with majority having moderate
delay.
TABLE I Disease Characteristics of the Study Population (N=75)
|
Characteristic |
No
(%) |
|
Presumed etiology |
| Provoked
|
51 (68.0) |
| Metabolic
derangement |
27 (36) |
|
Hypocalcemia |
26 (34.3) |
|
Neuroinfections |
22 (29.3) |
|
Pyomeningitis |
16 (21.3) |
| Others |
2 (2.7) |
| Unprovoked#
|
16 (21.3) |
| First febrile
seizure |
8 (10.7) |
|
Co-morbidities |
| Rickets |
16 (21.3) |
| Developmental
delay (n=64) |
13 (20.3) |
| Death during
hospital stay |
7 (9.3) |
|
#Benign infantile convulsions in 5. |
Nine (12%) infants died during the course of the
study, 7 of whom died during hospital stay. Maximum seizure deaths were
noticed in the neuro-infection group (Web Table I). The
median time from admission to death in those dying in hospital was 24
hours (range, 96 hours). The only infant in the unprovoked group dying
in the hospital died 4 days after admission, with septic shock. Two
infants, discharged in healthy state, died after discharge. One
2-month-old girl with acyanotic congenital heart disease, died one month
after discharge during an episode of bronchopneumonia. An 11-month-old
girl, diagnosed as benign infantile convulsion, was brought dead to the
hospital with a history of high-grade fever of three days duration, two
month after discharge.
Most studies on first non-febrile seizure in children
have shown very few abnormal results on laboratory studies [5]. In two
studies of both febrile and non-febrile seizures, results of laboratory
studies did not contribute to diagnosis or management [8,9]. However, in
another study of 65 children with new onset afebrile seizures, around
10% had either hyponatremia or hypocalcemia, mostly in those younger
than six months [5,10]. Previous results from developing countries also
suggest hypocalcemia to be a common cause of seizures in infants [3,7].
Our observation of developmental delay in 20% is similar to previous
reports of 15-27% [11,12]. A relatively high death rate during follow-up
observed in our study, has also been reported by few other studies
[13,14].
Limitations of the current study include a
convenience sample, absence of objective pre-morbid developmental
status, lack of video-EEG confirmation of seizure semiology, and a short
duration of follow-up, especially for seizure-recurrence and
developmental delay.
The major finding of the present study was that
hypocalcemia (due to rickets in majority) was responsible for more than
a third of the infants with the first seizure. Guidelines for evaluation
of first seizure in children from developed countries do not recommend
evaluation for metabolic derangements in a child with first seizure [5].
Our results favor evaluation for hypocalcemia in all infants presenting
with the first seizure. The presence of developmental delay in nearly a
fifth of the infants suggests that this group of infants may be
considered as a high-risk group for assessment and screening for
developmental delay.
Contributors: DM: conceived the study, provided
overall supervision, prepared the manuscript, and will be the guarantor;
NKN: identified, enrolled and managed the patients, searched literature,
analyzed the data, and helped in manuscript preparation; MJ, BT:
Provided important intellectual inputs during the planning and conduct
of the study and preparation of the manuscript; BT: reported on the EEG
findings. All authors approved the final manuscript for publication.
Funding: None; Competing interest: None
stated.
References
1. Chevrie JJ, Aicardi J. Convulsive disorders in
the first year of life: Etiologic factors. Epilepsia.
1977;18:489-98.
2. Mehrotra P, Marwaha RK, Aneja S, Seth A,
Singla BM, Ashraf G, et al. Hypovitaminosis D and
hypocalcemic seizures in infancy. Indian Pediatr. 2010; 47:581-6.
3. Agarwal KS, Beri RS, Puliyel JM. Repeated
unifocal seizure in post neonatal infants with hypocalcemia. Indian
Pediatr. 2000;37:203-5.
4. Commission on Classification and Terminology
of the International League Against Epilepsy. Proposal for revised
clinical and electroencephalographic classification of epileptic
seizures. Epilepsia. 1981;22:489-501.
5. Hirtz D, Ashwal S, Berg A, Beltis D, Camfeild
C, Crumrine P, et al. Practice parameter: Evaluating a first
non-febrile seizure in children. Neurology; 2000:55; 616-23.
6. Beghi E, Carpio A, Forsgren L, Hesdorffer DC,
Malmgren K, Sander JW, et al. Recommendation for a definition
of acute symptomatic seizure. Epilepsia. 2010; 51:671-5.
7. Huang CC, Chang YC, Wang ST. Acute symptomatic
seizure disorders in young children – a population study in southern
Taiwan. Epilepsia. 1998;39:960-4.
8. Smith RA, Martland T, Lowry MF. Children with
seizures presenting to accident and emergency. J Accid Emerg Med.
1996; 13:54-8.
9. Nypaver MM, Reynolds SL, Tanz RR, Davis T.
Emergency department laboratory evaluation of children with
seizures: dogma or dilemma? Pediatr Emerg Care. 1992; 8: 13-16.
10. Garvey MA, Gaillard WD, Rusin JA,
Ochsenschlager D, Weinstein S, Conry JA, et al. Emergency
brain computed tomography in children with seizures: who is most
likely to benefit? J Pediatr. 1998; 133:664-9.
11. Hamiwka LD, Singh N, Niosi J, Wirrell EC.
Diagnostic inaccuracy in children referred with "first seizure":
role for a first seizure clinic. Epilepsia. 2007;48:1062-6.
12. Sogawa Y, Masur D, O’Dell C, Moshe SL,
Shinnar S. Cognitive outcomes in children who present with a first
unprovoked seizure. Epilepsia. 2010;51:2432-9
13. Shinnar S, O’Dell C, Berg AT. Mortality
following a first unprovoked seizure in children: a prospective
study. Neurology. 2005; 64:880-2.
14. Loiseau J, Picot MC, Loiseau P. Short-term mortality after a
first epileptic seizure: a population-based study. Epilepsia.
1999;40:1388-92.
|
|
|
 |
|

