|
|
|
Indian Pediatr 2016;53: 879-882 |
 |
Bacterial
Co-infection in Hospitalized Children with Mycoplasma
pneumoniae Pneumonia
|
|
#
Qing Song, Bao-ping Xu and *Kun-Ling
Shen
From The #Aerospace Center Hospital and
*Beijing Children's Hospital, Capital Medical University, China.
Correspondence to: Dr KL Shen, Beijing Children's
Hospital, Capital Medical University, Beijing, 56 NanlishiRd, Xicheng
District, China.
Email: [email protected]
Received: September 10, 2015;
Initial review: October 26, 2015;
Accepted: August 08, 2016.
|
Objective: To describe the frequency and impact of bacterial
co-infections in children hospitalized with Mycoplasma pneumoniae
pneumonia.
Design: Retrospective, descriptive study.
Setting: Tertiary-care hospital in Beijing,
China.
Participants: 8612 children admitted to Beijing
Children's Hospital from June 2006 to June 2014.
Methods: According to the testing results of
etiology we divided the cases into pure M. pneumoniae infection
group and mixed bacterial infection group. We analyzed clinical
features, hospital expenses and differences between these two groups.
Results: 173 (2%) of included children had
bacterial co-infection. 56.2% of bacterial pathogens were identified as
Streptococcus pneumoniae.
Conclusion: The most common bacterium causing
co-infection in children with M. pneumoniae pneumonia was S.
pneumoniae.
Keywords: Acute respiratory infection, Etiology, Microbiology,
Streptococcus pneumoniae.
|
|
Mycoplasma pneumoniae
is a
common cause of community-acquired pneumonia (CAP) in children [1,2].
There is a scarcity of studies investigating co-infections of M.
pneumoniae pneumonia (MPP) in children. The purpose of this study
was to investigate the frequency and impact of bacterial co-infection in
hospitalized children with MPP. Bacterial co-infection occur in
respiratory MPP infections, but the attack rates and the clinical
profile are not clear. The purpose of this study was to investigate the
impact of bacterial co-infection in hospitalized children with MPP.
Methods
Medical records of all patients with MPP who were
admitted to Beijing Children's Hospital from June 2006 to June 2014 were
reviewed. The Pediatric Internal Medicine Department had 10039 MPP
admissions during this time. Cases were eligible for enrolment if
complete data were available. Pneumonia was diagnosed according to
standard guidelines [3-5].
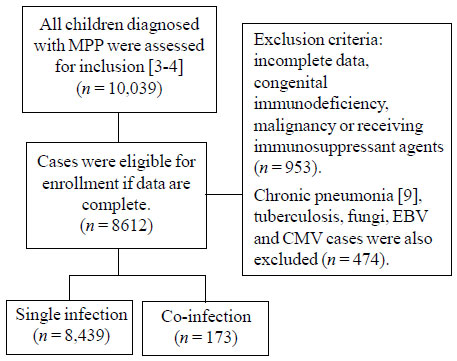
Patients were excluded if they had chronic pneumonia
[6], tuberculosis (TB), fungal, Epstein-Barr virus (EBV) or
Cytomegalovirus (CMV) infection, congenital immuno-deficiency,
malignancy, or were receiving immuno-suppressant agents. A total of
8,612 children aged 0-17 years old were included in this analysis (Fig.
1).
 |
|
Fig. 1 Study flow chart.
|
The acute and convalescent serum were obtained and
measured for antibody response to M. pneumoniae by enzyme-linked
immunosorbent assay methods (Serodia-mycoii, Japan) [7]. An acute
infection was indicated by a 1:160 antibody titres [8]. Patients were
also evaluated for viral, bacterial, tubercular or fungal infections.
All patients were screened for pulmonary tuber-culosis
by the Purified protein derivative skin test with 5TU purified protein
derivative. Blood, pleural effusion and bronchoalveolar lavage fluid
(BAL) were sent for slide review and bacterial, M. tuberculosis
and fungal culture.
A case with a co-infection was defined as any
bacterial pathogen except M. pneumoniae detected in any specimen.
A patient was considered to have a single infection if M. pneumoniae
was the only pathogen detected.
The severity of pneumonia was assessed by scores from
0 to 5 according to the number of following clinical find-ings observed
in the patients during admission (Table I): fever
(>38.5º), rapid breathing (and/or lower chest wall indrawing), decreased
oxygen saturation breathing room air (<92%), more than 7 days of
hospital stay, more than 2 affected pulmonary lobes on chest X-rays.
The patients with severity score ³3
were defined as severe pneumonia group and
£2 as
non-severe pneumonia group [5].
TABLE I Severity Assessment of Pneumonia in Included Children
|
Mild |
Severe |
|
Infants |
Temperature <38.5ºC |
Temperature<38.5ºC |
|
RR<50/min |
RR>70/min |
|
Mild recession |
Moderate to severe recession |
|
|
Nasal flaring |
|
|
Cyanosis |
|
|
Intermittent apnoea |
|
|
Grunting respiration |
|
Taking full feeds |
Not feeding |
|
Older children |
Temperature <38.5ºC |
Temperature<38.5ºC |
|
RR<50/min |
RR>50/min |
|
Mild breathlessness |
Severe difficulty in breathing |
|
|
Nasal flaring |
|
|
Cyanosis |
|
|
Grunting respiration |
|
No vomiting |
Signs of dehydration |
|
RR: respiratory rate. |
| |
The management of CAP in infants and children was
done as per standard guidelines [3-5]. Patients with severe M.
pneumoniae pneumonia who required intensive care unit (ICU)
admission were defined as per Infectious Diseases Society of
America/American Thoracic Society criteria for severe CAP [9]. The
symptoms mentioned above were typical of severe M. pneumoniae
pneumonia.
Statistical analyses: Analyses were performed
using SPSS 17.0 (SPSS Inc, Chicago, IL). The differences in age
distributions among patients with various pathogens identified were
tested by an independent sample t-test. P<0.05 was considered
statistically significant. Para-metric data were compared with
independent sample t-tests. Categorical data were analyzed by using the
chi-square test. We have performed a univariate and multivariate Cox's
regression analysis for various factors affecting hospital stay more
than 7 days.
Results
A total of 8612 children (age 2 m - 17 y; 51.6%
males) hospitalized with MPP were included in the study. Characteristics
of the 8,612 children hospitalized with MPP are shown in Table
II. There were 1012 children with severe pneumonia; and their
hospital stay was longer.
TABLE II Clinical Characteristics of Children Hospitalized with M. pneumoniae pneumonia
|
Characteristic |
Single infection |
Co-infection |
P value |
|
Number |
8439 |
138 |
|
|
Females; No.(%) |
4091(48.5) |
54 |
|
|
Age (year) |
9.2 |
5.9 |
0.001 |
|
Course of disease (d) |
8.3 |
12.6 |
0.003 |
|
Laboratory findings |
|
|
|
|
Leukocyte count (×109/L) |
6.21 |
12.1 |
0.001 |
|
Neutrophil (%) |
71.2 |
65.8 |
0.122 |
|
Lymphocyte (%) |
15.6 |
17.4 |
0.416 |
|
Platelet (×109/L) |
134.0 |
140.8 |
0.856 |
|
C-reactive protein (mg/L) |
22.1 |
31.6 |
0.006 |
|
Serum LDH (U/L) |
326.2 |
23.9 |
0.561 |
|
Serum CK (U/L)33.2 |
34.2 |
0.082 |
|
|
Serum ALT61.0 |
62.9 |
0.091 |
|
|
Hospital stay, median |
8.9 |
14.2 |
0.001 |
Tests for bacterial, acid-fast bacilli and fungal
infections were performed in all patients, and 2% (173/8612) of cases
were positive for at least one bacterial pathogen in addition to M.
pneumoniae. Bacterial isolates in these 173 cases are listed in
Table III. One bacterial pathogen was identified in 93.1%
(173/185), and two bacterial pathogens were identified in 6.9%(12/173).
S. pneumonia, Haemophilus influenzae (H. influenzae) and
Staphylococcus aureus (S.aureus) were the most common source of
infection (Table III).
TABLE III Pathogens Indentified in Children With Mycoplasmal Pneumonia
|
Pathogen(s) |
Cases |
Pathogen(s) |
Cases |
|
S. pneumoniae + H. influenzae |
3 |
S. epidermidis |
2 |
|
S. pneumoniae + K. pneumoniae |
1 |
S. aureus |
12 |
|
S. pneumoniae + B. cepacia |
3 |
B. cepacia |
4 |
|
S. pneumoniae + H. parainfluenzae |
3 |
Sewer coli |
1 |
|
B. cepacia + H. influenzae |
1 |
M. luteus |
1 |
|
A. baumannii + S. coli |
1 |
P. aeruginosa |
7 |
|
S. pneumoniae |
94 |
N. gonorrhoeae |
4 |
|
H. influenzae |
19 |
E. coli |
1 |
|
H. parainfluenzae |
10 |
A. baumannii |
2 |
|
K. pneumoniae |
4 |
|
|
Significant differences were observed in course of
diseases, leukocyte count, and C-reactive protein between single and
co-infections (Table II). There was no significant
difference in Neutrophil, Lymphocyte, Platelet, Serum lactate
dehydrogenase (LDH), Serum Creatine kinase (CK) and Serum Alanine amino-transferase
(ALT) between patients with single infections and those who with
co-infection (Table II). Hospital stay of children with
single infections was shorter as compared to those with than bacterial
co-infections (Table II).
Web Table
I
presents the results of univariate and multivariate Cox's regression
analysis for various factors affecting hospital stay more than 7 days.
Age was an important factor affecting hospital stay. Unilobar or
Multilobar pneumonia was another important factors. Mixed infections and
severe pneumonia also contributed to prolonged hospital stay
Discussion
In this retrospective study from China, 2% of
children with MPP were infected with another bacterial pathogen. S.
pneumoniae was the leading cause of bacterial co-infection.
Co-infections led to more disease severity in children with MPP compared
with single infections.
There were several limitations to our study. First,
nearly all children in our study received antibiotic treatment. This may
have affected the results of bacterial culture. Second, we did not study
co-infection with viruses.
Frequency of co-infections in our study was lesser
than that seen in few other reports from China [10,11]. This could be
related to inclusion of viruses as cause of co-infectioin in these
studies. The distribution and age categorization of various bactria
isolated in our study is in general similar to other reports from
developing countries [12,13].
We conclude that bacterial co-infections are
relatively uncommon in M. pneumoniae pneumonia. S. pneumoniae
is the most common cause of bacterial infection in M. pneumoniae
pneumonia.
Contributors: SQ: prepared the manuscript and
performed the statistical analysis. SQ: critically revised the
manuscript; KLS: contributed to conception and design; BPX: critically
revised the manuscript.
Funding: China National Clinical Research Center
for Respiratory Disease Fund (grant number 2013BAI09B11); Competing
interest: None stated.
|
What This Study Adds?
• About 2% of children with Myloplasma
pneumoniae pneumonia may have bacterial co-infection.
|
References
1. Kashyap S, Sarkar M. Mycoplasma pneumonia:
clinical features and management. Lung India. 2010;27:75-85.
2. Ferwerda A, Moll HA, de Groot R. Respiratory tract
infections by Mycoplasma pneumonia in children: a review of diagnostic
and therapeutic measures. Eur J Pediatr. 2001;160:483-91.
3. Shen KL, Jiang ZF. Mycoplasma pneumonia. M. Hu YM,
Jiang ZF. Zhu Futang Textbook Practical?Pediatrics. The seventh edition.
Beijing. People's Medical Publishing House. 2014; 1205.
4. Pediatrics of Chinese medical association branch
of breathing group. The Chinese journal pediatrics editorial board. The
management of community acquired pneumonia in infants and children
clinical practice guidelines. Chin J Pediatr. 2013;51:745-52.
5. Michael H, Julia C, Nicky C, Penny F, Anthony H,
Michael M, et al. British Thoracic Society guidelines for the
management of community acquired pneumonia in children: update 2011.
Thorax. 2011;66:ii1-ii23.Doi:10.1136/thoraxjnl-2011-200598.
6. Jiang ZF. Chronic pneumonia. Hu YM, Jiang ZF. Zhu
Futang Textbook (Practical) Pediatrics. The seventh edition. Beijing.
People's Medical Publishing House 2014;1213.
7. Hirschberg L, Krook A, Pettersson CA, Vikerfors T.
Enzyme-linked immunosorbent assay for detection of Mycoplasma pneumoniae
specific immunoglobulin M. Eur J Clin Microbiol Infect Dis.
1988;7:420-3.
8. Sinaniotis CA, Sinaniotis AC. Community-acquired
pneumonia in children. Curr Opin Pulm Med. 2005;11:218-25.
9. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG,
Campbell GD, Dean NC, et al. American Thoracic Society.
Infectious Diseases Society of America/American Thoracic Society
consensus guidelines on the management of community-acquired pneumonia
in adults. Clin Infect Dis. 2007;44:S27-72.
10. Chen LL, Cheng YG, Chen ZM, LI SX, LI XJ, Wang
YS. Mixed infections in children with Mycoplasma pneumonial pneumonia.
Chin J Pediatr. 2012;50:211-5.
11. Michelow IC, Olsen K, Lozano J, Rollins NK, Duffy
LB, Ziegler T, et al. Epidemiology and clinical characteristics
of community-acquired pneumonia in hospitalized children. J Pediatrics.
2004;113:701-7.
12. Chen CJ, Lin PY, Tsai MH, Huang CG, Tsao KC, Wong
KS, et al. Etiology of community acquired pneumonia in
hospitalized children in Northern Taiwan. Pediatr Infect Dis J.
2012;31:e196-201.
13. Liu XT, Wang GL, Luo XF, Chen YL, Ou JB, Huang J, et al.
Spectrum of pathgens for community-acquired pneumonia in children.
Zhongguo Dang Dai. Er Ke Za Zhi. 2013v15N1: 42-5.
|
|
|
 |
|

