|
|
|
Indian Pediatr 2009;46: 887-890 |
 |
Clinical Risk Factors Associated With
Extubation Failure in Ventilated Neonates |
|
GM Hiremath, K Mukhopadhyay and A Narang
From the Division of Neonatology, Advanced Pediatric
Centre, PGIMER, Chandigarh 160 012, India.
Correspondence to: Dr Kanya Mukhopadhyay, Associate
Professor, Neonatology, PGIMER, Chandigarh 160 012, India. Email:
[email protected]
Manuscript received: June 3, 2008;
Initial review : June 24, 2008;
Accepted: September 9, 2008.
Published online 2009 April 15. PII:S097475590800358-2
|
|
Abstract
We conducted this study to find out the
incidence of extubation failure (EF) in ventilated neonates and
associated clinical risk factors. Eighty two ventilated neonates were
followed up to 48 hours post-extubation to look for EF. Twenty two
babies (26.8%) had EF. The common risk factors for EF were presence of
patent ductus arteriosus, post-extubation lung collapse and acquired
pneumonia. The duration of ventilation, and maximum and pre-extubation
alveolar arterial oxygen gradients (AaDO2) were significantly higher (P<0.05)
in EF group. The incidence of sepsis (P=0.034), anemia (P=0.004)
and pneumonia (P=0.001) were significantly higher in EF group.
Detection of significant PDA and adequate post extubation care may help
to reduce rate of extubation failure in neonates.
Key words: Extubation failure, Newborn, Risk factors,
Ventilation.
|
|
W
eaning neonates off mechanical
ventilation involves as much art as science(1). Extubation failure (EF) in
neonates can occur upto one-third of cases(2). An attempt to extubate is
considered a failure if there is a need for reintubation or need for
accessory respiratory support within 48 hours of extubation(3). The causes
of extubation failure vary from upper airway edema or stenosis to drugs,
sepsis, extreme prematurity, post-extubation atelectasis and
bronchopulmonary dysplasia(4,5). Usually, more than one factor is
responsible for extubation failure(5). The present research was intended
to document the incidence and risk factors associated with EF in
ventilated neonates.
Methods
This was a prospective observational study done in a
level III neonatal unit over one year period. All inborn neonates
ventilated for at least 12 hours were eligible. Neonates with major
congenital malformation, HIE stage III or intraventricular hemorrhage
grade 4 (USG confirmed), and babies on continuous positive airway pressure
(CPAP) and nasal intermittent mandatory ventilation (NIMV) were not
included. The study was approved by Institute research ethics committee
and written informed consent was obtained from all parents.
All ventilated babies were monitored every hour for
vitals along with continuous saturation monitoring till 48 hours post-extubation.
Biochemical and blood gas monitoring was done 12- hourly. The decision of
extubation was according to unit policy which were (i) Clinical:
improvement in basic disease and complications managed (all
hemodynamically significant PDA had ECHO done and treated); (ii)
Laboratory: acceptable blood gas, packed cell volume >30%, normal
blood sugars and electrolytes; (iii) Ventilator setting at minimum:
peak inspiratory pressure of 12-14 cm of water, positive end expiratory
pressure of 3 to 3.5 cm of water, rates of 15-20/min, FiO2 0.3 to 0.25 and
hemodyna-mically stable for 12-24 hours. Aminophylline was started pre-extubation
in babies <34 weeks of gesta-tion and steroid was used in cases of
prolonged venti-lation (more than 7 days). Stomach was emptied and ET
suction was done just before extubation. Babies <1.5 kg were put on CPAP
(4-5 cm H2O) and babies >1.5 kg were
directly extubated to head box O2.
Extubation failure was defined as the need for
reintubation or accessory respiratory support in the form of CPAP in those
babies who were on head box O2, within 48
hours of extubation. The decision of reintubation or extubation failure
was taken if 2 or more of the following were present: (i) Increase
in respiratory rate of >25% baseline; (ii) Increase in FiO2
requirement of >50% of baseline; (iii) Downe’s score >6 (6);
(iv) Silverman’s score >7(7) and; (v) PaO2 <50 mm Hg,
or PaCO2 >60 mm Hg.
For each episode of extubation failure, a primary,
definite cause was assigned by the resident and consultant in charge who
were not masked. All other contributory factors were recorded as secondary
causes. Only the first episode was considered for calculating incidence in
cases of repeated extubation failure. In case a child died on ventilator
or left against medical advice (LAMA), he was excluded from the final
analysis of incidence of extubation failure.
Results
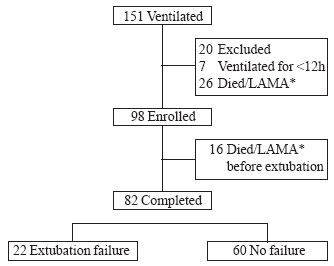
Enrolment is shown in Fig. 1. The
demographic characteristics are given in Table I and
they are similar to the babies who did not complete the study. The
commonest indication of ventilation was hyaline membrane disease (40.2%)
in both the groups, followed by congenital pneumonia which was
significantly (P=0.005) more in the EF group (n=5, 22.7%) as
compared to no EF group (n=2, 3.3%). Recurrent apnea was the second
most common indication of ventilation in no EF (n=14) group as
compared to none in EF group.
|
 |
|
* LAMA – left against medical advice and
care withdrawn
Fig. 1 Flowchart of total ventilated cases. |
TABLE I
Demographic Characteristics of Subjects
|
Variable |
Group1 |
Group 2 |
P value |
|
|
( EF) |
(no EF) |
|
|
|
n=22 |
n=60 |
|
|
Gestational age |
29.9±2.4 |
31.05±3.6 |
0.291 |
|
(wk)(mean ±SD) |
|
|
|
|
Gestational age categories |
|
<28 wk |
2 (9) |
7 (11.6) |
0.74 |
|
28 - 37 wk |
19 (86.3) |
46 (76.6) |
0.33 |
|
≥37 wk |
1 (4.7) |
7 (11.8) |
0.33 |
|
Birthweight (g) |
1402±463 |
1444±623 |
0.80 |
|
(mean±SD) |
|
|
|
|
Birthweight categories |
|
<1 kg |
4 (18.8) |
12 (20) |
0.85 |
|
1 to 2.499 kg |
17 (77.2) |
43 (71.6) |
0.61 |
|
≥2.5 kg |
1 (4) |
5 (9.4) |
0.55 |
|
Sex |
|
|
|
|
Male |
17 (77.3) |
50 (83.3) |
0.37 |
|
Antenatal steroid |
16 (73) |
39 (65) |
0.51 |
|
received |
|
|
|
|
Values are expressed as mean + SD and n (%). |
The incidence of extubation failure was 26.8% (n=22).
Thirteen babies (15%) needed reintubation while 9 (10%) babies needed CPAP
only. There were no differences among various weight and gestation
subcategories. The three most common primary causes of extubation failure
were patent ductus arteriosus (PDA), post extubation collapse and acquired
pneumonia (5 each out of 22 cases). The other primary causes were apnea of
prematurity, hypothermia, shock, stridor, BPD spell, premature weaning and
aspiration, accounting for 1 case each.
The duration of SIMV in the extubation failure group
was significantly higher in the EF group than in the no failure group
(167±121 hours and 90±95 hours respectively, P=0.006). Maximum
Alveolar- arterial oxygen gradient (AaDO2) was significantly higher (P=0.003)
in EF group (246±150) as compared to no EF group (159±105). Pre extubation
AaDO2 was also higher (P=<0.001) in EF group (51 ± 17) than no EF
group (33±14). But a similar significant difference was not found in the
initial AaDO2. Presence of prior anemia, pneumonia and sepsis
significantly increased the risk of extubation failure (Table II).
TABLE II
Risk Factors in Neonates With Extubation Failure
|
Risk Factor |
EF group
(n=22) |
No EF group
(n=60) |
P value |
Relative risk |
95% Confidence Interval |
| Anemia |
11 (50%) |
11 (18%) |
0.004 |
2.7 |
1.38 to 5.37 |
| Pneumonia |
12 (54%) |
10 (16%) |
0.001 |
3.27 |
1.65 to 6.48 |
| Sepsis |
9 (42%) |
11 (18%) |
0.034 |
2.23 |
1.07 - 4.64 |
Discussion
Extubation failure is still a common occurrence in
neonatal units(3-5) and nearly one fourth of our babies had extubation
failure, which is in concordance with other studies(4,8). Some authors
found the association between low gestational age and low birthweight to
extubation failure(4), but we did not observe this as probably we had less
number of ELBW babies. Extubation failure usually indicates either
incomplete resolution of underlying illness or the development of new
problems. Unrecognized patent ductus arteriosus (which can be missed
clinically in upto 50% cases) and fluid overload can contribute
significantly to the incidence of extubation failure and their signs can
be masked in a ventilated neonate, until the end expiratory pressure is
removed and hence many PDA may remain silent(5), which probably happened
in our cases. Five cases of EF were attributed to post extubation
collapse. Use of CPAP, adequate humidification and physiotherapy have been
proposed to decrease the incidence of post extubation collapse(9-11).
Acquired pneumonia accounted for a significant number of EF probably
related to high number of sepsis in our unit. Prolonged duration of
ventilation has been quoted as a risk factor of extubation failure(12-14)
and we also found the similar trend, probably suggesting the fact that
these babies had severe lung disease needed longer duration of
ventilation. The maximum as well as the pre-extubation AaDO2 were
significantly higher in the EF group, suggesting that these neonates had a
significant lung disease leading to a higher chance of extubation failure.
Babies who had anemia any time during their course also
had a higher risk of extubation failure which is in concordance with other
studies(15). We also found an association between pre-existing pneumonia
and sepsis, and extubation failure, which probably are related to sickness
of the baby and requiring prolonged ventilation in pneumonia cases. The
strength of our study is a large sample size and meticulous study
protocol, which was followed strictly, but the limitations are small
number of ELBW babies in whom chances of extubation failures are higher.
We also did not attempt NIMV before reintubating them. Future trials
should include larger no of ELBW babies and trying NIMV for extubation
failure cases.
Contributors: GMH and KM conceived the idea and GMH,
KM, AN designed the study. GMH collected the data. GMH and KM analysed the
data, drafted the paper. AN helped in critical review of manuscript.
Funding: None.
Competing interests: None stated.
|
What This Study Adds?
• Patent ductus arteriosus, post extubation lung
collapse and acquired pneumonia are associated with extubation
failure in neonates.
|
References
1. Sinha SK, Donn SM. Weaning from assisted
ventilation: Art or Science? Arch Dis Child Fetal Neonatal Ed 2000 ; 83: F
64-70.
2. Eric C Eichenwald, Cloherty JP. Mechanical
ventilation. In: Manual of Neonatal Care, 5th ed. Philadelphia
Lipincot Williams and Wilkins; 2004. p. 348-361.
3. Kavvadia V, Greenough A, Dimitriou G. Prediction of
extubation failure in preterm neonates. Eur J Pediatr 2000; 159: 227-231.
4. Dimitriou G, Greenough A, Endo A, Cherian S,
Rafferty GF. Prediction of extubation failure in preterm infants. Arch Dis
Child Fetal Neonatal Ed 2002; 86: F32-36.
5. Goldsmith JP, Roca TP. Ventilatory management
casebooks. In: Goldsmith JP, Karotkin EH, eds. Assisted Ventilation
of the Neonate, 4th ed. Philadelphia: WB Saunders; 2003. p. 519-521.
6. Wood DW, Downes JJ, Locks HI. A clinical score for
the diagnosis of respiratory failure. Am J Dis Child 1972; 123: 227-229.
7. Silverman WC, Anderson DH. Controlled clinical trial
on effects of water mist on obstructive respiratory signs, death rate and
necropsy findings among premature infants. Pediatrics 1956; 17: 1-4.
8. Vento G, Tortorolo L, Zecca E, Rosano A, Matassa PG,
Papacci P, et al. Spontaneous minute ventilation is a
predictor of extubation failure in extremely-low-birth-weight infants. J
Matern Fetal Neonatal Med 2004; 15: 147-154.
9. Higgins RD, Richter SE, Davis JM. Nasal continuous
positive airway pressure facilitates extubation of very low birth weight
neonates. Pediatrics 1991; 88: 999-1003.
10. So BH, Tamura M, Mishina J, Watanabe T. Application
of nasal continuous positive airway pressure to early extubation in very
low birth weight infants. Arch Dis Child 1995; 72: F191-193.
11. Flenady VJ, Gray PH. Chest physiotherapy for
prevention of morbidity in babies being extubated from mechanical
ventilation. Cochrane Database Syst Rev 1999; 2: CD 000283.
12. Darmon JY, Rauss A, Dreyfuss D, Bleichner G,
Elkharrat D, Schlemmer B, et al. Evaluation of risk factors for
laryngeal edema after tracheal extu-bation in adults and its prevention by
dexa-methasone. Anaesthesiology 1992; 77: 245-251.
13. Koka BV, Andre JM, Smith RM, Jeon IS, Mackay I.
Postintubation croup in children. Anaesth Analg 1977; 56: 502-505.
14. Baisch SD, Wheeler WB, Kurachek SC, Cornfield DN.
Extubation failure in paediatric intensive care: incidence and outcomes.
Pediatr Crit Care Med 2005; 6: 312-318.
15. Rothaar RC, Epstein SK. Extubation failure:
magnitude of the problem, impact on outcomes, and prevention. Curr Opin
Crit Care 2003; 9: 59-66.
|
|
|
 |
|

