|
|
|
Indian Pediatr 2016;53: 990-992 |
 |
Longitudinal Growth in
Children and Adolescents with Type 1 Diabetes
|
|
Lavanya Parthasarathy, Vaman Khadilkar, Shashi
Chiplonkar and Anuradha Khadilkar
From Hirabai Cowasji Jehangir Medical Research
Institute, Jehangir Hospital, Pune, Maharashtra, India.
Correspondence to: Dr Anuradha Khadilkar, Hirabai
Cowasji Jehangir Medical Research Institute, Jehangir Hospital, 32
Sassoon Road, Pune.411 001, India.
Email:
[email protected]
Received: July 08, 2015;
Initial review: August 20, 2015;
Accepted: September 07, 2016.
|
Objective: To study longitudinal growth in children with type 1
diabetes mellitus.
Methods: Anthropometry, disease duration, insulin
regimens and HbA1C recorded from patients with diabetes enrolled in a
specialty clinic.
Results: 160 children (75 boys; mean (SD) age 9.4
(3.3) y) were enrolled. 35% children had low (<25th centile) height
velocity. Disease duration and HbA1C affected height velocity (adjusted
for puberty). Children on basal-bolus had higher height velocity Z
scores than those on a split mix regimen [(0.5(1.6) vs.
-0.3(1.4), P<0.05)]. Children diagnosed before 5 years of age had
lowest height velocity. Of the children who reached final height, 53%
remained below target height.
Conclusion: Children with type 1 diabetes
mellitus have lower height velocity compared to healthy children; those
diagnosed at younger age were at higher risk for growth failure.
Keywords: Diabetes mellitus, Growth Failure, Height,
Short Stature.
|
|
T
ype 1 diabetes mellitus (T1DM) is known to
adversely affect linear growth. Reduced growth and pubertal spurt in
diabetic children could be due to abnormalities in physiological bone
growth and perturbations in Growth hormone – Insulin- like growth factor
– Insulin (GH–IGF-I) axis [1]. Studies suggest that abnormalities are
common in subjects with poor metabolic control and longer disease
duration [2-5]. We conducted this study with the objectives of (i)
assessing height velocity of 4- to 16-year-old children with T1DM and
identifying factors affecting it over a one-year period; and (ii)
studying the effect of disease duration on growth during adolescent
years and on final height.
Methods
All children (age 4-16 y) visiting the type 1
diabetes clinic at a tertiary healthcare centre, in Western India were
approached for the study (May 2012- June 2014). Patients on medication
other than insulin for blood glucose control or with known
co-morbidities (celiac disease, untreated hypothyroidism, and other
chronic diseases) were excluded. Considering variability in velocity
reported in studies [6], sample size of 160 (objective 1) and 91
(objective 2) had power of 0.9 at 5% level of significance and 5% margin
of error. Ethical approval was granted by institutional ethics
committee. Assent from children and consent from parents was obtained.
Data on age at diagnosis, diabetes duration and insulin regimen were
collected. Tanner staging was performed.
Standing height (Leicester Height Meter, Child Growth
Foundation, UK) and weight (electronic scale) was measured 3-monthly by
the same observer, and converted to Z scores [7]. Yearly height velocity
values were calculated by dividing difference between annual height
measurements by age increment. Using LMS values (skewness (L), median
(M), and coefficient of variation (S) of the measurement distribution)
from the data on normal children (n=1471), height velocity
Z-scores for diabetic children were calculated [8]. Parents’ heights
were recorded using the same stadiometer to calculate mid-parental
height. Final height was defined when chronological age was >18 years or
a growth rate <0.5 cm during the last 6 months, and was compared to
target height [9].
Fasting blood sample was collected to measure HbA1C
(HPLC). An average of readings taken 3-monthly was used to describe the
metabolic control over one year.
Statistical analyses were carried out using SPSS
(version 16). Differences in means were tested using Student’s t test.
Linear regression was used to identify factors affecting HV. Polynomial
regression models were fitted for HV Z scores according to age at
diagnosis.
Results
We selected 160 children (75 boys) enrolled in the
clinic for the study on height velocity. Mean (SD) HV at end of study
was 5.5 (2) cm; mean (SD) HVZ score was -0.3 (1.5), and 35% had HV <25th
centile [8] (Table I).
TABLE I Baseline Characteristics of the Study Population
|
|
Boys (n=75) |
Girls (n=85) |
Total (n=160) |
|
Age (y) |
9.3 (3.5) |
9.5 (3.1) |
9.4 (3.3) |
|
Height (cm) |
127.6 (20.4) |
127.6 (17.3) |
127.6 (18.9) |
|
HFA Z score |
–0.9 (1.3) |
–0.9 (1.1) |
–0.9 (1.2) |
|
Weight (kg) |
27 (11.2) |
26.5 (10) |
26.7 (10.6) |
|
WFA Z Score |
–0.8 (1.1) |
–0.8 (1.0) |
–0.8 (1.1) |
|
BMI (kg/m2) |
15.8 (2.4) |
15.7 (2.3) |
15.7 (2.3) |
|
BFA Z score |
–0.5 (0.8) |
–0.5 (0.9) |
–0.5 (0.8) |
|
HbA1C (%) |
8.8 (1.8) |
8.8 (1.9) |
8.8 (1.8) |
|
*Duration (y) |
3.3 (2.7) |
3.2 (2.7) |
3.2 (2.7) |
HFA: Height for age; WFA: Weight for Age; BFA: BMI for age; BMI: Body mass index; HbAIC: glycosylated hemoglobin.
*Duration of diabetes.
|
Children on basal-bolus regimen (n=72) had
better mean (SD) HVZ score (0.5 (1.6) vs -0.3 (1.4), P<0.05)
and significantly lower HbA1C (8.4 (1.7)% vs 9.0 (1.8)%) than
those on split mix. Disease duration ( b
= -0.091, P=0.020) and HbA1C (1yr
average, b
= -0.177, P=0.001) were significant negative
predictors of HVZ scores after adjusting for puberty.
We extracted retrospective data on 91 of these
children for their height measurements during the past 2-11 years.
Across adolescence, children who were diagnosed at <5 years of age (n=32)
had the least and those diagnosed >10 years of age (n=25) had
maximum HVZ scores (Fig. 1). HVZ scores peaked at
12 years for those diagnosed >10 years; at 14 years if diagnosed between
5-10 years (n=34), and at 15 years for <5 years. Amplitude of
peak was highest in children diagnosed >10 years and smallest for those
diagnosed < 5 years (Fig. 1).
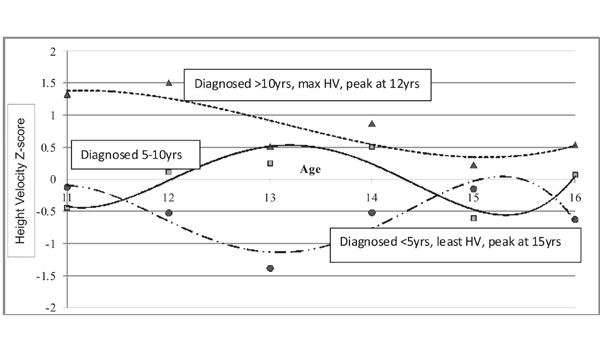 |
|
Circle- diagnosed <5yrs; Square- diagnosed
between 5-10 yrs; Triangle- diagnosed >10yrs.
Fig. 1 Height velocity Z scores during adolescence
according to age at diagnosis (longitudinal follow up).
|
Fifty percent (45/91) children achieved final
heights, and 47% percent surpassed or equaled target height. According
to age at diagnosis (<5, 5-10, >10 years), percentage of children who
did not meet target height was 80%, 33%, and 50%, respectively. When
compared to Indian references at 18 years, 18% children had HAZ scores
below -2 SD.
Discussion
Our study suggests that children with diabetes were
shorter and had lower height velocity than healthy children. Longer
disease duration and poor metabolic control were associated with low
height velocity Z scores. Height velocity of children diagnosed at
younger years, was the least across adolescent years and majority of
them fell short of target height.
Limitations of the study are data on height at
diagnosis were not available as children were followed from the first
time they visited the centre which was not necessarily at diagnosis.
Moreover, we did not evaluate IGF1 concentrations which could have
further helped in understanding the reason for lower height velocity and
reduced final height. Some earlier studies [2,10-12] have also shown
that children who had better metabolic control had higher HVZ scores,
underlining the importance of improving metabolic control. Children on
basal-bolus regime had better HVZ score and lower HbA1C; promoting the
use of basal-bolus regime may help to optimize growth. Like others
[1,2,13,14], our data also suggest that patients diagnosed before 5
years of age showed greatest height loss, and need more attention
towards growth. In our study, half the children who had reached final
height did not meet their target height, which is in contrast to other
studies who have reported normal final height amongst diabetic children
[1,2,3,5].
We conclude that children with T1DM are shorter, and
have lower height velocity in comparison with healthy children. It is
critical to monitor and improve metabolic control in children diagnosed
at younger years as they seem to be at higher risk for long-term growth
failure.
Contributors: LP, AK, VK: data collection; SC:
statistical analyses. All the authors contributed to the manuscript,
writing and its final approval.
Funding: Mr Pancharatnam and University Grant
Commission (UGC), Government of India through fellowship to first
author; Competing interest: None stated.
|
What This Study Adds?
•
Children diagnosed with type 1
diabetes mellitus at younger years are at higher risk for
long-term growth failure and reduced final height, which further
worsens with poor metabolic control.
|
References
1. Chiarelli F, Giannini C, Mohn A. Growth, growth
factors and diabetes. Eur J Endocrinol. 2004;151:U109-17.
2. Holl RW, Grabert M, Heinze E, Sorgo W, Debatin KM.
Age at onset and long-term metabolic control affect height in type-1
diabetes mellitus. Eur J Pediatr. 1998;157:972-7.
3. Timóteo C, Castanhinha S, Constant C, Robalo B,
Pereira C, Sampaio L. Growth and puberty in type 1 diabetes mellitus -
experience from a pediatric endocrinology unit. Acta Med Port.
2012;25:213-8.
4. Salerno M, Argenziano A, Di Maio S, Gasparini N,
Formicola S, De Filippo G, et al. Pubertal growth, sexual
maturation, and final height in children with IDDM. Effects of age at
onset and metabolic control. Diabetes Care. 1997;20:721-4.
5. Khadilkar VV, Parthasarathy LS, Mallade BB,
Khadilkar AV, Chiplonkar SA, Borade AB. Growth status of children and
adolescents with type 1 diabetes mellitus. Indian J Endocrinol Metab.
2013;17:1057-60.
6. Tanner JM, Whitehouse RH, Takaishi M. Standards
from birth to maturity for height, weight, height velocity, and weight
velocity: British children, 1965. I. Arch Dis Child. 1966;41:454-71.
7. Khadilkar VV, Khadilkar AV, Cole TJ, Sayyad MG.
Cross-sectional growth curves for height, weight and body mass index for
affluent Indian children, 2007. Indian Pediatr. 2009;46:477-89.
8. Khadilkar VV, Khadilkar AV, Parthasarathy LS,
Chiplonkar SA, Ekbote VH, Phanse SS, et al. Height velocities in 5-16
year old apparently healthy Indian children. 16th International Congress
of Endocrinology. 2014. P. 404.
9. Tanner JM, Goldstein H, Whitehouse RH. Standards
for children’s height at ages 2-9 years allowing for heights of parents.
Arch Dis Child. 1970;45:755-62.
10. Demir K, Altýncýk A, Abacý A, Büyükgebiz A, Böber
E. Growth of children with type 1 diabetes mellitus. J Clin Res Pediatr
Endocrinol. 2010;2:72-7.
11. Gunczler P, Lanes R, Esaa S, Paoli M. Effect of
glycemic control on the growth velocity and several metabolic parameters
of conventionally treated children with insulin dependent diabetes
mellitus. J Pediatr Endocrinol Metab. 1996;9:569-75.
12. Bognetti E, Riva MC, Bonfanti R, Meschi F,
Viscardi M, Chiumello G. Growth changes in children and adolescents with
short-term diabetes. Diabetes Care. 1998;21:1226-9.
13. Dunger D, Ahmed L, Ong K. Growth and body
composition in type 1 diabetes mellitus. Horm Res. 2002;58:66-71.
14. Danne T, Kordonouri O, Enders I, Weber B. Factors
influencing height and weight development in children with diabetes.
Results of the Berlin Retinopathy Study. Diabetes Care. 1997;20:281-5.
|
|
|
 |
|

