|
|
|
Indian Pediatr 2016;53: 1017-1018 |
 |
Retained
Capsule Endoscope
|
|
Jayalaxmi S Aihole, *GS
Vishnumurthy and M Narendra Babu
From Departments of Pediatric Surgery and *Paediatric
Gastroenterology, IGICH Bangalore, Karnataka, India.
Correspondence to: Dr Jayalaxmi S Aihole, Department
of Pediatric surgery, IGICH, Bangalore, Karnataka, India.
Email:
[email protected]
Received: September 12, 2015;
Initial review: October 26, 2015;
Accepted: August 09, 2016.
|
Background: Capsule endoscopy was invented to visualize the entire
small intestine in a non- invasive manner in adults. Case
characteristics: 1 y, 9 mo-old boy presented with generalized edema
for last 3 months. His routine investigations, including the upper
gastrointestinal endoscopy, colonoscopy, and contrast enhanced computed
tomography scan (CECT) were normal. In view of clinical suspicion of
protein losing enteropathy, we planned capsule endoscopy.
Observation: The capsule was not passed even after 3 weeks.
Laparoscopy revealed impacted capsule in a dilated intestinal loop
proximal to an ileal stricuture. Message: Capsule endoscopy
should be used judiciously in children.
Keywords: Bowel obstruction, Capsule endoscopy, Complication.
|
|
Capsule endoscopy was invented
to visualize
the entire small intestine in a non-invasive
manner. Later, its use was widened to include
children [1,2]. However,
capsule endoscopy CE has its own limitations in children, and should be
used judiciously.
Case Report
A 21-month-old boy presented to us with generalized
edema for last 3 months. Previously, patient was evaluated elsewhere and
was treated for hypo-albuminemia with clinical improvement. On
admission, child had anasarca and anemia. He weighed 10 kg and had a
length of 74.5 cm (<3 rd
centile). His hemoglobin level was 5.1 g/dL, serum proteins were 3.7
g/dL, serum albumin was 1.5 g/dL, and serum globulins were 1.6 g/dL.
Stool examination for ova, cysts and occult blood was negative.
Paediatric Crohn’s Disease Activity Index was 37.5, suggesting moderate
disease activity. Further investigations including echocardiogram, upper
gastro-intestinal (GI) endoscopy and colonoscopy, contrast enhanced
computed tomography scan (CECT) were normal. In view of clinical
suspicion of protein losing enteropathy, we planned capsule endoscopy.As
the child was not able to swallow the capsule, it was placed under
endoscopic guidance into the third part of duodenum using endoscopic
basket. Child was discharged with advice of close follow up. We used the
new version CapsoCam SV1 (Capsovision, CA) of size 11 mm × 31 mm,
which provides panoramic 360° images with a higher frequency of 20
frames per second for the first 2 h and thereafter 12 frames/s, with a
battery life of 15 h.
 |
|
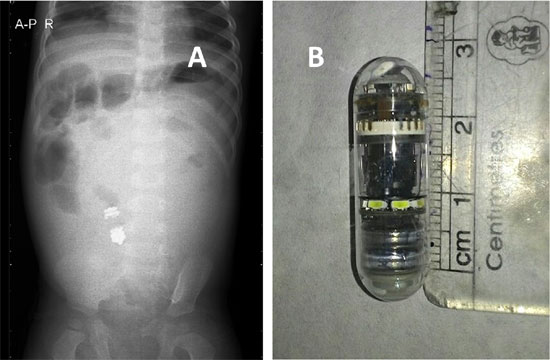
Fig. 1 (a) X-ray showing capsule
endoscrope in small bowel; (b) CAPSCOCAM Capsule
endoscope.
|
In view of non-evacuation of capsule even after 3
weeks, we evaluated him with abdominal radiography and ultrasonography
(USG) which revealed the retained capsule in the small bowel (Fig.
1a). A diagnostic laparoscopy was done which revealed
impacted capsule in the dilated mid ileal loop proximal to the
stricture. The capsule was retrieved (Fig. 1b) and
segment of ileum including focal stricture, a short circumferential
narrowing of 2 mm width, was resected and end-to-end anastomosis was
done. The small bowel mesentery was normal without any significant lymph
node enlargement. Gross examination of resected ileum did not show any
ulcers. Histopathological examination of the resected segment of ileum
revealed stricture without any ulcers with focal pyloric gland
metaplasia with viable surgical margins. Surprisingly, the images
captured by the capsule were all normal. Child is doing well for after
year of follow-up.
Discussion
Indications for capsule endoscopy in children include
evaluation of the small-bowel mucosa for evidence of Crohn’s disease,
occult bleeding, celiac disease, polyps, graft-versus-host disease,
lymphangiectasia, and diseases contributing to growth failure or
abdominal pain [2]. Capsule
endoscopy is considered safe and well tolerated, and has been approved
by the U.S. Food and Drug Administration for children
³2 years of age [3].
American Societies for Gastrointestinal Endoscopy (ASGE) guidelines
recommend its use in children as young as 2 years in special
circumstances [3]. The
primary limitations of performance of this procedure in pediatric
patients include the inability to swallow the capsule or tolerate
placement because of the inability to pass the upper esophageal
sphincter or pylorus.
Fritscher and Ravens [4] tried the feasibility and
safety of capsule endoscopy in a 1.5-year-old child. Another case report
was published on successful use of the capsule in a 10-month-old infant
weighing 7.9 kg [5]. In patients who are unable to swallow the capsule,
the capsule can be placed endoscopically in the third part of duodenum,
using retrieval nets, snares, or dedicated capsule placement devices to
prevent migration back into the stomach [2,3,6].
The main risk associated with capsule endoscopy is
capsule retention, which has been reported to occur in less than 1% of
pediatric patients [3]. The
International Conference on Capsule Endoscopy (ICCE) consensus defined
the capsule retention as, having a capsule endoscope remaining in the
digestive tract for a minimum of 2 weeks, or a capsule remaining in the
bowel for a shorter period with symptoms requiring medical, endoscopic
or surgical intervention [2,7]. A capsule retention rate of 1.4% was
reported in a large series of 207 pediatric patients, which is similar
to the rate in adults [8]. In the present case, histopathology revealed
lamina propria infiltrated with neutrophils,
lymphocytes and many eosinophils with a stricturous area showing focal
pyloric gland metaplasia and submucosal fibrosis. This is the one of the
earliest pathological findings for Crohn’s disease
[9]. Only a few such cases have been reported in
India.
Role of laparoscopy in the detection of the retained
capsule is well established. Moreover, definitive surgery to resect the
pathologic stricture can also be performed.
We retrieved the retained capsule with
laparoscopy-assisted procedure, and we were able to carry out resection
and anastomosis of the focally strictured ileal segment.
Newly designed non visualizing dissolvable capsule
with two timer plugs has been developed in order to minimize the risk of
retention [10]. However, few cases of capsule retention requiring
emergency surgery have even been described with this patency capsule
[10].
A retained capsule may indicate unsuspected stricture, which might
require surgical intervention.
Acknowlegment: Mr Preetham and all the paediatric
surgical colleagues for their inputs in managing this case.
Contributors: JSA: concept, preparing the
manuscript, review of literature; GSV: concept, review of literature,
revision of the manuscript; MNB: Critical review of manuscript.
Funding: None; Competing interest: None
stated.
References
1. Jensen MK, Tipnis NA, Bajorunaite R, Sheth MK,
Sato TT, Noel RJ. Capsule endoscopy performed across the pediatric age
range: indications, incomplete studies, and utility in management of
inflammatory bowel disease. Gastrointest Endosc. 2010;72:95-102.
2. Tokuhara D, Watanabe K, Okano Y, Tada A, Yamato K,
Mochizuki T. Wireless capsule endoscopy in pediatric patients: the first
series from Japan. J Gastroenterol. 2010;45:683-91.
3. ASGE Standards of Practice Committee, Lightdale
JR, Acosta R, Shergill AK, Chandrasekhara V, Chathadi K, et al.
American Society for Gastrointestinal Endoscopy. Modifications in
endoscopic practice for pediatric patients. Gastrointest Endosc.
2014;79:699-710.
4. Fritscher-Ravens A, Scherbakov P, Bufler P,
Torroni F, Ruuska T, Nuutinen H, et al. The feasibility of
wireless capsule endoscopy in detecting small intestinal pathology in
children under the age of 8 years: a multicentre European study. Gut.
2009;58:1467-72.
5. Nuutinen H, Kolho KL, Salminen P, Rintala R,
Koskenpato J, Koivusalo A, et al. Capsule endoscopy in pediatric
patients: technique and results in our first 100 consecutive children.
Scand J Gastroenterol. 2011; 46: 1138-43.
6. Barth BA, Donovan K, Fox VL. Endoscopic placement
of the capsule endoscope in children. Gastrointest Endosc.
2004;60:818-21.
7. Atay O, Mahajan L, Kay M, Mohr F, Kaplan B, Wyllie
R. Risk of capsule endoscope retention in pediatric patients: A large
single-center experience and review of the literature. J Pediatr
Gastroenterol Nutr. 2009;49:1-6.
8. Friedrich K, Gehrke S, Stremmel W, Sieg A. First
clinical trial of a newly developed capsule endoscope with panoramic
side view for small bowel: A pilot Study. J Gastroenterol Hepatol.
2013;28:1496-501.
9. Koukoulis GK, Ke Y, Henley JD, Cummings OW.
Detection of pyloric metaplasia may improve the biopsy diagnosis of
Crohn’s ileitis. J Clin Gastroenterol. 2002; 34:141-3.
10. Delvaux M, Ben Soussan E, Laurent V, Lerebours E,
Gay G. Clinical evaluation of the use of the M2A patency capsule system
before a capsule endoscopy procedure, in patients with known or
suspected intestinal stenosis. Endoscopy. 2005;37:801-7.
|
|
|
 |
|

