|
|
|
Indian Pediatr 2014;51:
925-927 |
 |
Severe Calcinosis Cutis with Cutaneous
Ulceration in Juvenile Dermatomyositis
|
|
Bijay Kumar Meher, Pravakar Mishra, Pradeep Sivaraj
and *Prasanta Padhan,
From Department of Paediatrics, Sardar Vallavbhai
Patel Post Graduate Institute of Paediatrics, SCB Medical College,
Cuttack; and *Department of Rheumatology, Kalinga Institute of Medical
Sciences, Bhubaneswar, Odisha, India.
Correspondence to: Dr Bijay Kumar Meher, 34/B, Vima
Bihar, Sector-6, CDA, Cuttack, Odisha, India.
Email: bkmeher187@yahoo.co.in
Received: June 21, 2014;
Initial review: July 22, 2014;
Accepted: September 20, 2014.
|
|
Background: Calcinosis cutis is
usually seen in long standing and untreated cases of juvenile
dermatomyositis. Case characteristics: 7-year-old girl with
severe calcinosis cutis who developed cutaneous ulceration, rash and
myopathy. Observation: Myopathic changes in EMG, muscle edema in
MRI, elevated muscle enzymes and Jo-1 positive antibodies. Outcome:
Treatment with prednisolone and methotrexate resulted in improvement
of the lesion. Message: Calcinosis cutis may be a presenting
feature of juvenile dermatomyositis even in the absence of
characteristic findings of rash and weakness.
Keywords: Calcification, Dermatomyositis,
Diagnosis.
|
|
J
uvenile dermatomyositis (JDM) is a rare
multisystem autoimmune disorder with an incidence of 3 per million
population [1]. It is characterized early in its course by perivascular
inflammation of striated muscles and skin, and later by development of
calcinosis. Classic JDM manifests with an insidious progression of
malaise, easy fatigue, muscle weakness, fever and rash that may appear
before diagnosis by 3 to 6 months [2]. Lipodystrophy and calcinosis are
well described in JDM and are more commonly seen in long standing or
neglected disease. We report a case of juvenile dermatomyositis who
presented with extensive calcinosis cutis with ulceration long before
development of characteristics rash and weakness.
Case Report
A 7-year-old girl born out of non-consanguineous
marriage presented to us with multiple tender nodular swelling at the
back of both thigh with overlying deep ulcers at the back of right
thigh. At 6 years of age, she had pain in both thighs more on right side
– for which she had consulted physicians, neurologist, rheumatologist
and dermatologist. The pain was dull aching in nature, not related to
physical activity, and was associated with limping on the right side.
She had multiple nodular swelling on thighs and arms. Investigations
revealed normal blood counts, high erythrocyte sedimentation rate (20 mm
in 1 st hr.), raised
c-reactive protein (25 mg/dL), low vitamin D3 (17.95 ng/mL), normal
calcium and phosphorus, normal thyroid function tests, normal creatine
kinase (94 U/L), normal C3 (126 mg/dL), normal C4 (40 mg/dL), negative
antinuclear antibody by EIA (0.13) and negative anti-ds DNA (2 U/mL).
She was treated conservatively and started vitamin D supplementation
(60000 IU/week). The patient did not seek any medical advice for the
next 6 months.
On presentation to our hospital, the patient had
multiple tender nodular swellings with reddish brown pigmentation on the
back of both thighs with ulcerations on right side (Fig.
1). Due to pain and restriction of movements, muscle weakness in
the lower limbs could not be elicited. Violaceous rash suggestive of
heliotrope rash was visible on the eyelids, and multiple bright pink
shiny thickened plaques on the metacarpophalangeal joints and proximal
interphalangeal joints suggestive of Gottron papules were seen.
Provisional diagnosis of juvenile dermatomyositis was made and wound
debridement was done. Pus culture was positive for Staphylococcus
and histopathology revealed necrotic granulomatous inflammation with
foci of calcifications. Appropriate antibiotic was started with regular
dressing.
 |
|
Fig. 1 Non-healing ulcer on lower
limbs and X-ray showing extensive subcutaneous calcifications.
|
Her investigations revealed normal blood counts,
raised erythrocyte sedimentation rate (44 mm in 1 hr), raised aspartate
transaminase (92U/L), raised serum LDH (681U/L, normal 313-618), normal
alanine transaminase (44 U/L), normal serum creatine kinase (75 U/L),
normal anti-phospholipid antibody (IgG 2.4 GPLU/mL, IgM 2.5 MPLU/mL),
normal renal function tests and normal ionized calcium (1.25mmol/L),
phosphate (5.6 mg/dL) and alkaline phosphate (600 U/L). Doppler
ultrasound of limbs showed normal arterial and venous blood flow and
multiple echogenic lesions in subcutaneous tissue of both thighs and
legs. Electromyography (EMG) showed features of inflammatory myopathy.
Plain radiograph of limbs showed multiple linear and stippled
calcifications in the subcutaneous tissue in all limbs, more marked in
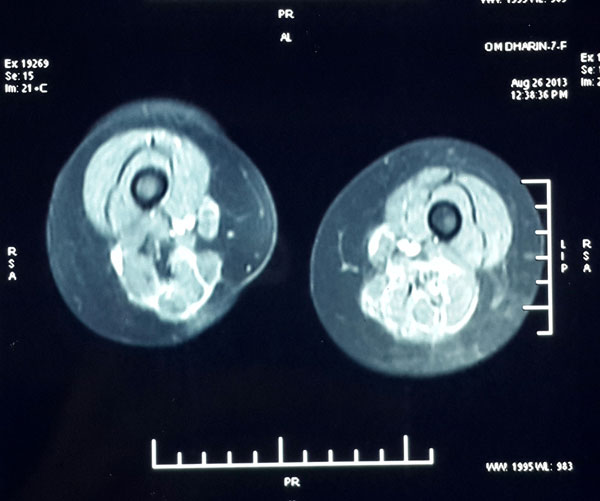
the lower limbs (Fig. 1). Magnetic Resonance
Imaging (MRI) revealed ill-defined high signal in Short Tau inversion
recovery (STIR) sequences suggestive of muscle edema in bilateral thigh
regions and few low signal foci suggestive of calcifications (Fig.
2). Antinuclear antibody (ANA) was positive: speckled 1 and ANA
profile (ELISA) revealed strongly positive for Anti-Jo-1 antibody. Chest
radiograph and high resolution computed tomograhy (HRCT) thorax did not
show any features of interstitial lung disease. A diagnosis of Juvenile
dermatomyositis was considered in the presence of pathognomic rash,
myopathic changes in electromyogram (EMG), muscle edema in magnetic
resonance imaging (MRI), elevated muscle enzymes and supported by
calcinosis cutis and Jo-1 positive antibodies.
 |
|
Fig. 2 MRI of thighs showing
ill-defined high signal in STIR sequences suggestive of muscle
edema in both thighs and few low signal foci suggestive of
calcifications.
|
Prednisolone was started at a dose of 1 mg/kg/day.
Follow-up after one month of treatment revealed healing of one ulcer
with presence of well vascularized granulation tissue in the base of
another ulcer and disappearance of the nodules. Radiograph showed
partial resolution of the calcinosis. Oral methotrexate 10 mg/week along
with folate supplementation was started in addition to prednisolone.
Discussion
Subcutaneous calcifications may occur due to several
rheumatological conditions (Juvenile dermatomyositis, Systemic lupus
erythematosus, and Systemic sclerosis), infections or local tissue
traumas [3,4]. In JDM, calcinosis is less frequently present at
diagnosis, reported in only 3% to 23% of patients [5]. When calcinosis
develops before weakness, pain and stiffness due to calcinosis cutis
masks the weakness on clinical examination, but EMG and MRI can
differentiate both. In our case, myopathy in EMG was detected after 7
months of calcinosis. Calcinosis cutis in JDM may be related to severity
of disease, delayed initiation of treatment and potentially to genetic
polymorphisms of TNF- a-308.
It is thought to be associated with longstanding or undertreated disease
[1]. Calcium deposition may occur in subcutaneous plaques or nodules, as
large tumorous deposits in muscle groups, as calcification within
fascial planes, bridging joints, or as an extensive subcutaneous
exoskeleton [6]. Some ulcerate through the skin and drain a soft
calcific liquid, and others manifest as hard nodules along extensor
surfaces or embedded along muscle [1]. Our case presented with indurated
nodule and extensive subcutaneous calcification which subsequently deve-loped
ulceration in the back of thigh, typical rash (Gottron papules and
heliotrope rash) and EMG feature of myopathy suggestive of JDM. Similar
observation was made by Wananukul, et al. who reported calcinosis
cutis in two cases years before appearance of other clinical
manifestations of JDM [7].
Calcinosis cutis may be a presenting feature of
juvenile dermatomyositis and should be thought of even in the absence of
characteristic findings of rash and weakness so that early and effective
therapy can be instituted to prevent progression.
Contributors: BKM: diagnosed the case, drafted
the manuscript, reviewed the literature; PP and PM: helped in diagnosis,
drafting and revising critically; PS: reviewed the literature and
managed the case. All the authors finally approved the final version.
Acknowledgements: Dr Deepti Damayanty Pradhan, Dr
Suchismita Bhuyan and Dr Anil Kumar Mohanty.
Funding: None; Competing interests: None
stated.
References
1. Robinson AB, Reed AM. Juvenile Dermatomyositis.
In: Kliegman R, Stanton B, Geme III J, Schor N, Behrman R, editors.
Nelson Textbook of Pediatrics. 19th ed. Philadelphia:
Saunders;2011.P.846
2. Rider LG, Lindsley CB, Cassidy JT. Juvenile
Dermatomyositis.In: Cassidy JT, Petty RE, Laxer RM, Lindsley CB,
editors.. Textbook of Pediatric Rheumatology. 6th ed. Canada: Saunders
Elsevier; 2011.P.383
3. Lobo IM, Machado S, Teixeira M, Selores M.
Calcinosis cutis: A rare feature of adult dermatomyositis. Dermatol
Online J. 2008;14:10.
4. Tristano AG, Villarroel JL, Rodriguez MA, Millan
A. Calcinosis cutis universalis in a patient with systemic lupus
erythematosus. Clin Rheumatol. 2006;25:70-4.
5. Ramanan AV, Feldman BM. Clinical features and
outcomes of juvenile dermatomyositis and other childhood onset myositis
syndromes. Rheum Dis Clin North Am. 2002;28:833-57.
6. Blane CE, White SJ, Braunstein EM, Bowyer SL,
Sullivan DB. Patterns of calcification in childhood dermatomyositis. Am
J Roentgenol. 1984,142:397-400.
7. Wananukul S, Pongprasit P, Wattanakrai P.
Calcinosis cutis presenting years before other clinical manifestations
of juvenile dermatomyositis: Report of two cases. Australas J Dermatol.
1997;38:202-5.
|
|
|
 |
|

