|
|
|
Indian Pediatr 2014;51: 897-899 |
 |
An Outbreak of Rubella in Chandigarh, India
|
|
* K Madhanraj,
#N Singh,
$M
Gupta, ^MP Singh, and
^RK Ratho
From Departments of Community Medicine, *Pondichery
Institute of Medical Science, Pondicherry and #GMCH, Chandigarh; and
$School of Public Health and ^Department of Virology, PGIMER,
Chandigarh; India.
Correspondence to: Dr Madhanraj, Assistant Professor, Department of Community Medicine, PIMS, Pondicherry.
Email: [email protected]
Received: July 23, 2013;
Initial review: August 19, 2013;
Accepted: September 15, 2014.
|
|
Objective: To investigate an
outbreak of fever with rash in an urbanized village in Chandigarh,
India.
Methods: Active case search was
performed by house-to-house survey. The etiological agent of the
outbreak was confirmed by serology. Spot map was done using Geographical
Information System (GIS) technology.
Results: Out of 7742 persons
screened, 12 were serologically confirmed rubella cases and 83 were
epidemiologically linked cases. Overall attack rate was 1.1, more among
the age group 1-4 years (4.9).
Conclusion: An outbreak mimicking
measles was investigated only to be confirmed as rubella.
Keywords: Epidemiology, Outbreak
investigation, Rubella.
|
|
Large-scale rubella vaccination during the past
decade has practically eliminated rubella and congenital rubella
syndrome (CRS) in many developed and some developing countries [1,2].
About 131 of the 194 WHO member States introduced rubella-containing
vaccines (RCVs) in their routine immunization programmes along with
measles and/or mumps by 2010 [1].
In India, there is a lack of comprehensive evidence about
the true burden of rubella and CRS [2].
Setting up of reliable surveillance system for
understanding local rubella epidemiology can provide such information.
The present study was done to investigate an outbreak of exanthematous
illness to document local descriptive epidemiology and to control the
outbreak.
Methods
In fourth week of May 2012, a four-year-old girl from
an urbanized village, Burail in Chandigarh [3], reported to the health
center in the field practice area of School of Public Health, PGIMER,
with the complaints of fever and rash meeting the clinical description
of measles [4]. Based on the details given by the index case, a team of
two postgraduate resident doctors (each from School of Public Health and
Department of Virology) from PGIMER, Chandigarh, visited the area with
the aim to confirm and investigate the measles outbreak. Initial line
listing of ten cases of febrile rash was done by rapid inquiry in
neighbourhood houses of index case and in the nearby anganwadis.
Blood samples were collected from thirty nine cases after informed
consent of parents for serological testing. All the blood samples
collected were found to be negative for measles IgM by ELISA (Novatech,
Germany). These were then tested for rubella IgM antibodies by ELISA (Dialab,
Italy) and twelve turned out to be positive. Thus, suspected measles
outbreak turned out to be a confirmed rubella outbreak. House-to-house
survey was done to investigate the outbreak further.
World Health Organization (WHO) definition of
suspected rubella case of ‘occurrence of fever with maculopapular rash,
with or without cervical, sub occipital or post auricular adenopathy or
arthralgia /arthritis in any patient of any age’ was used [4,5].
Active case search was started from mid-June 2012
and extended till the end of first week of July 2012. It was stopped
when no case was reported for three consecutive days. The passive
surveillance was continued for another three weeks. Cases were mapped
using Geographical Information System technology. The data were analysed
by using Epi-info 7. Epidemiological analysis included time, place and
person analysis. This investigation was done in the context of public
health response to an outbreak. Therefore, retrospective approval was
obtained from the Institute Ethics Committee.
Results
A total of 7742 persons were contacted during the
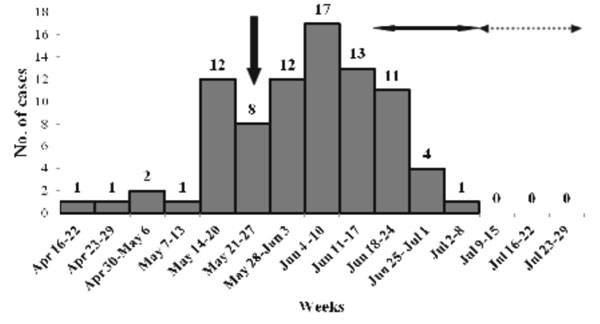
house-to-house survey and 83 cases were identified. Epidemic curve is
given in Fig. 1. The overall attack rate (AR) was 83/7742
(1.1%), and was higher in the age-group of 1-4 years. No complication or
mortality was reported. There was one pregnant ante-natal woman among
cases. Out of 83 cases, 31 cases (37.3%) were immunized against measles.
Among unimmunized cases, 20 (57.1%) cases were in age group of 1-4
years. Five cases (6%) had received MMR from private clinic. None of the
adolescent case had history of rubella immunization.
 |
|
Fig.1 Epidemic curve of rubella
outbreak by time of onset of rash in Burail village, Chandigarh.
Vertical arrow indicates week of reporting of index case.
Horizontal arrow (solid) indicates period of active case finding
and horizontal arrow (dotted) indicates period of passive case
finding.
|
Discussion
In this study, an outbreak of fever with rash in an
urbanized village in Chandigarh was investigated. It was confirmed as
rubella that affected all age groups and had higher AR among children
aged 1-4 years. One pregnant woman was found to be affected; on follow
up she had a normal pregnancy outcome.
Limitation of this investigation could be incomplete
coverage of the study area, as 20% population is migratory and 10% work
as labourers during day hours as per the annual health survey report
2011-12, Burail. However, locked houses were visited at least three
times before excluding from the survey.
TABLE I Distribution and Attack Rate of the Cases by Age Group and Sex
|
Age (years) |
Female |
Male |
Total |
|
Cases |
Total |
Attack rate |
Cases |
Total |
Attack rate |
Cases |
Total |
Attack rate |
|
0-1 |
3 |
108 |
2.8 |
3 |
131 |
2.3 |
6 |
239 |
2.5 |
|
1-4 |
16 |
324 |
4.9 |
19 |
391 |
4.9 |
35 |
715 |
4.9 |
|
5-9 |
15 |
400 |
3.8 |
6 |
481 |
1.2 |
21 |
881 |
2.4 |
|
10-14 |
5 |
398 |
1.3 |
2 |
480 |
0.4 |
7 |
878 |
0.8 |
|
³ 15 |
8 |
2281 |
0.4 |
6 |
2748 |
0.2 |
14 |
5029 |
0.3 |
|
Total |
47 |
3511 |
1.3 |
36 |
4231 |
0.9 |
83 |
7742 |
1.1 |
Compared to results of rubella outbreak in Himachal
Pradesh in 2006 where adolescents were mainly affected, children less
than 10 years were affected in this outbreak [6]. Low attack rate, no
complication and no mortality reiterates the mild nature of the disease
as mentioned in other studies [6-9]. About 57% of the cases in 1-4 years
age group were not immunized against measles in the study area. This is
because of floating nature of the population in this area. However it is
an important indicator for consideration before introducing RCVs.
Inadequate vaccine coverage may decrease rubella virus circulation in
children sufficiently with the resultant upward shift of the median age
at infection, thus leading to higher proportion of girls remaining
susceptible up to adulthood leading to a paradoxical increase in the
number of rubella infections and also in the number of cases of
Congenital Rubella Syndrome [10]. Prevailing cultural and religious
beliefs regarding febrile rashes in the community prevent people from
bringing their children to hospital. Hence these disease are less likely
to get reported unless strong surveillance system and sensitization of
the community is in place. Moreover, behaviour of the people to visit
local practitioners for minor ailments might delay the identification of
outbreak. In order to prevent and control such outbreaks in future, it
is essential to strengthen the existing disease surveillance system.
Contributors: KM and NS: Data collection,
drafting manuscript; MG: Intellectual inputs to manuscript; MPS:
Laboratory investigations, Intellectual inputs to manuscript; RKR:
Intellectual inputs to manuscript.
Funding: School of Public Health, PGIMER,
Chandigarh; Competing interests: None stated.
|
What This Study Adds?
• Rubella has the
potential to cause outbreak in the community that are often
missed or considered to be due to measles unless there is strong
surveillance system.
|
References
1. World Health Organization: Global measles and
Rubella, Strategic Plan 2012-2020. Geneva: World Health Organization;
2012. Accessed from: http://www.
measlesrubellainitiative.org/learn/the-solution/the-strategy/.
Accessed April 21, 2013.
2. Dewan P, Gupta P. Burden of congenital Rubella
syndrome (CRS) in India: A systematic review. Indian Pediatr.
2012;49:377-99.
3. Provisional Population Totals. Chandigarh. Census
of India 2011. Accessed from:
http://censusindia.gov.in/2011-provresults/prov_data_products_chandigarh.html.
Accessed November 19, 2013.
4. World Health Organization: Measles and Rubella
Surveillance and Outbreak Investigation Guidelines. Regional Office for
South-East Asia: World Health Organization; 2009. Accessed from:
http://www.who.int/immunization/newsroom/Measles_Rubella_Strategic
Plan_2012_2020.pdf. Accessed April 20, 2013.
5. World Health Organization: Report of a Meeting on
Preventing Congenital Rubella syndrome: Immunization, Surveillance
Needs. Geneva:World Health Organization; 2000. Accessed from:
http://whqlibdoc.who.int/hq/ 2000/WHO_V&B_00.10_eng.pdf. Accessed
April 21, 2013.
6. Gupta SN, Gupta NN. An outbreak of rubella in a
hilly district of Kangra-Chamba, Himachal Pradesh, India, 2006. Indian J
Pediatr. 2009;76:717-23.
7. Singh MP, Diddi K, Dogra S, Suri V, Varma S, Ratho
RK. Institutional outbreak of rubella in a healthcare center in
Chandigarh, North India. J Med Virol. 2010;82:341-4.
8. Singh MP, Arora S, Das A, Mishra B, Ratho RK.
Congenital rubella and cytomegalovirus infections in and around
Chandigarh. Indian J Pathol Microbiol. 2009;52:46-8.
9. Singla N, Jindal N, Aggarwal A. The
seroepidemiology of rubella in Amritsar (Punjab). Indian J Med Microbiol.
2004;22:61-3.
10. Bhaskaram P, Ramalakshmi BA, Raju LA, Raman L.
Need for protection against rubella in India. Indian J Pediatr.
1991;58:811-4.
|
|
|
 |
|

