octors are expected to
consistently exhibit professional attitudes, behaviour, values and
ethics in their practice. Professionalism is an important component of
medicine's contract with society. The concept of the profession of a
doctor has changed considerably with the times. Previously, doctors were
granted autonomy by the community, with the belief that they would place
the welfare of their patients before their own. However in contemporary
society, this autonomy has been challenged by the altered public
perception of the role of the doctor. Their behaviour is now observed
and scrutinized more closely by the media. Doctors' own attitudes
towards their vocation have also changed [1,2].
Though a small minority of professionals exhibit
inappropriate professional behaviour, they end up receiving
disproportionate attention, maligning the entire profession. Medical
errors, adverse outcomes, malpractice and inappropriate behaviour result
when doctors do not adhere to guidelines, have difficult workplace
relationships, find themselves inadequate in communication,
collaboration and transfer of information, or suffer from low morale
[3].
Studies from the West have shown that students who
demonstrate unprofessional behaviour during their undergraduate and
postgraduate education are more likely to be found guilty of
unprofessional actions by the monitoring boards after they graduate
[3,4]. Thus, the need to include teaching and assessment of
professionalism in the formal curricula for undergraduate and
postgraduate medical training has been globally acknowledged. The
Medical Council of India (MCI), the custodian of medical education in
the country, has not even explicitly mentioned professionalism in the
Graduate Medical Education Regulations [5]. The Postgraduate Medical
Education Regulations 2000 cursorily mention that their goal is to
produce competent specialists "who shall recognize the health needs of
the community, and carry out professional obligations ethically and in
keeping with the objectives of the national health policy", but do not
elaborate this further. The focus is on acquisition of theoretical
knowledge, practical and clinical skills, communication skills, and
research acumen [6]. Further, there is no consensus on what is meant by
professionalism or how it should be integrated into the curriculum.
Assessment of professionalism is an even more contentious territory as
it is such an intangible entity.
Defining Professionalism
Professionalism is a theoretical construct, more
easily described in lofty idealistic terms than by observable
behaviours. There is also much variation in what 'professionalism' means
across different countries. Epstein and Hundert, in 2002, defined
professional competence as "the habitual and judicious use of
communication, knowledge, technical skills, clinical reasoning,
emotions, values, and reflection in daily practice for the benefit of
the individual and community being served’’ [7]. The Royal College of
Physicians, UK, defines professionalism as "a set of values, behaviours,
and relationships that underpin the trust the public has in doctors"[8].
The American Board of Internal Medicine identified the key elements of
professionalism as: altruism, accountability, duty, excellence, honor,
integrity and respect for others [8]. The medical educationists from
Netherlands defined professionalism in terms of observable behaviours to
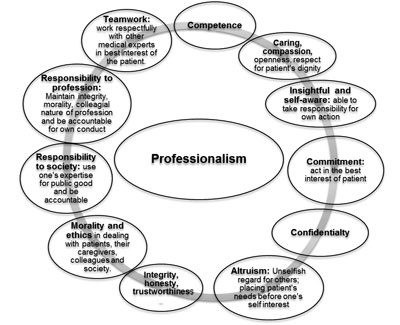
make assessment feasible [8]. In an effort to make these elements more
explicit, a faculty development initiative tried to build consensus by
defining some of the core attributes of professionalism. Some of these
are displayed in Fig. 1 [9].
 |
|
Fig. 1 Core attributes of
professionalism,
|
Evolving definitions of professionalism perhaps
reflect the place it is accorded in medical training. The elements in
initial definitions are easy to identify but difficult to measure as
learning outcomes. The subsequent definitions include behaviours that
are observable, to some extent measurable, and hence amenable to
assessment and inclusion as a core curricular component.
The societal and cultural value system influences the
perception and interpretation of professional behaviour of a physician.
Naturally, while everyone agrees on the core elements of
professionalism, a consensus on a culturally appropriate global
definition appears to be lacking. Therefore, it is imperative for each
country and every institution to develop its own definition of
professionalism, according to the societal norms of the times, and
identify its core elements.
Though no Indian publication dedicated to defining
professionalism in Indian context could be found on literature search,
there have been recent meetings and conferences addressing this issue.
One of the authors (TS) was a keynote speaker at a deliberation on
Professionalism held at Karamsad in April 2013 where these aspects were
discussed in depth. Also, a workshop and meeting of the Indian
physicians from all over the world (Global Indian Doctors) was held in
Kolkata in January 2014 to address the worrisome decline in practice of
professionalism and ethics. They noted the critical role of education
and mentorship in inculcating right values from the start of medical
training [10]. A welcome beginning was also made by the MCI in form of
proposed new regulations for Graduate Medical Education 2012 that
mentioned some aspects of professionalism as a core competency for
Indian medical graduates.
Teaching And Learning Professionalism
Professionalism is not a single skill, but a
multi-dimensional competency construct with several component skills. A
combination of teaching-learning methods is essential for imparting
training in professionalism. It is worthwhile to address the 'why, what,
who, where, when and how' of teaching professionalism before
incorporating it into the curriculum [11].
Why does professionalism need to be taught and
assessed?
For years, the development of professional values in
a doctor was taken for granted and it perhaps held true in the earlier
apprenticeship model of physician training. With changing models of
physician training, this view has changed. As professionalism is so
intrinsic and integral to the medical profession, it should be an
explicit part of the medical curriculum. It is now globally agreed that
professionalism is a core competency for physicians and cannot be left
to informal means to be imbibed [8,12]. It is well known that what is
not assessed is not valued by students. Therefore, institutions need to
develop written criteria about what needs to be taught and assessed.
What should be taught and learnt?
As mentioned earlier, it is important for each
institution to define professionalism in its own context. The faculty as
well as students should have a clear understanding of the traits,
characteristics and qualities that contribute to professionalism. A
written statement of curricular outcomes, content (such as ethics,
decision making/moral reasoning, humanism, empathy, communication), and
an explicit list of knowledge, skills and attitudes guards against
delivering conflicting messages to students [13]. Developing an
institutional curriculum for professionalism with a feasible and
acceptable blueprint for teaching-learning and assessments is also
likely to instil a sense of ownership in the faculty, and hence
facilitate effective delivery of this curriculum [14].
Who should teach and be taught?
Without doubt, professionalism should be included in
the formal curriculum of both undergraduate medical students and
postgraduate trainees [9,13]. At the same time, the traditional place of
professionalism in the hidden and informal curriculum deserves equal
attention. The behaviour of faculty must reflect the attributes of
professionalism as endorsed by the institution rather than be at
conflict with it. For this, the sensitization and training of faculty in
teaching learning and assessing professionalism is of key importance.
The students' training will enable them to observe and imbibe
appropriate attitude and behaviour.
When and where should professionalism be taught?
Teaching and learning of professionalism cannot be
confined to a certain stage of medical training but has to be explicitly
'woven into the fabric' of entire undergraduate curriculum and also the
postgraduate training [15]. Inculcation of professional values should
begin at the time of entry into medical school. Cruess and Cruess
suggest 'continuity' and 'incremental approach' in teaching-learning and
assessing professionalism in medical schools [16]. They further propose
that with an initial strong cognitive base, 'stage appropriate'
educational activities (including assessment) should be devised. Faculty
must also utilize the opportunities at workplace to reinforce the
correct behaviour and allow the students to practice what they have
learnt during the formal training sessions in professionalism. Thus
training should focus not only on inculcating the core aspects of
professionalism, but also on making the student a self-motivated and
self-directed learner.
How should professionalism be taught?
Many of the core attributes of professionalism are
related to soft skills. Some common aspects that contribute to bringing
about attitudinal or behavioural changes and are integral to planning
educational activities for professionalism are outlined below:
(i) Motivation (self-driven;
intrinsic): Students must imbibe the importance of the desired
change in behaviour for it to be a driving force.
(ii) Observation of role models:
Teachers have always been role models for students and their
positive as well as negative behaviour patterns are likely to be
imbibed by the students (informal and hidden curriculum). The
trainees need orientation and a cognitive base to be able to
discriminate between good and poor role modelling [17].
(iii) Continued stimulus to be thinking
about these aspects of being a physician rather than in spurts
occasionally.
(iv) Feedback: Timely and effective
feedback on own behaviour received from friends, colleagues, peers,
seniors with positive reinforcement of desired behaviour as well as
corrective suggestions for improvement.
(v) Reflection and reflective practice:
Very simply expressed as ‘mental processing with a purpose or
anticipated outcome’, this is the key to attitudinal change [8]. One
could reflect on an experience or a behaviour or on feedback
received. 'Reflection on action' is most important and can be well
encouraged by providing situations and experiences during the course
of training [15].
(vi) Extrinsic motivation: Reward
or appreciation related to behaviour. Assessment works by way of
feedback as well as by providing an extrinsic motivation.
Teaching professionalism involves several intricacies
(Box I). The teaching-learning methods that may be
utilized are:
• Interactive lecture and brainstorming:
These can help in initial sensitization and in introducing students
to the concept. A good cognitive base with clarity on definitions
and concept in the initial stages of training will enable the
students to make the most out of experiences and other educational
activities in later stages of training [18].
• Clinical scenarios or case vignettes:
These could be designed to focus on various aspects of
professionalism, such as, honesty with patients, patient
confidentiality, maintaining appropriate behaviour with patients and
their caregivers, active listening etc. Small group discussions or
individual exercises that involve responding to such scenarios
compel the students to reflect on these aspects of a doctor's
working [18].
• Reflective exercises: These could be
discussions based on actual situations that arose during work,
sharing of own experiences by the trainee or based on what they
observed. Dedicated time needs to be put aside for this activity
[15].
• Feedback: Provision of timely and
effective feedback to the trainee is a powerful way of guiding the
development of professional values. The feedback should be specific,
based on an observed incident/behaviour and be given along with a
feed forward for appropriate behaviour in future in such situations.
The importance of observing in authentic workplace setting and
providing feedback based on it cannot be overemphasised. Assessment
methods such as mini-clinical evaluation exercise and directly
observed procedural skills (DOPS) have 'feedback' built into the
assessment process and are therefore excellent teaching methods as
well.
• Portfolios: Student portfolios, in
contrast to a log-book, include reflections of the student in his
own words. This is another way of compelling the trainees to
think-back about their observations and experiences, and thus
inculcate a habit of self-development based on reflective thinking
[19].
• Role models: Students knowingly or
unknowingly imbibe the professional behaviour of teachers. So it is
of utmost importance that teachers are sensitized to their role as a
'role model' to the students and that they are consciously aware of
the same at all times [17].
• Art-based interventions: Use of arts in
medical education to foster a better understanding of patients'
perspectives is also being utilized as a strategy for developing
professional values in some institutions. This approach not only
develops trainees as better communicators, but also encourages them
to explore own feelings [20]. The 'Theatre of the Oppressed'
initiative by the medical humanities group of University College of
Medical Sciences, New Delhi, India is an example of this effort in
India.
|
Box I Strategies to Teach Professionalism |
•
|
Sensitization: Orienting students to the concept of
professionalism and its importance so that they recognize it as an
essential component of physician training and subsequent practice. |
•
|
Immersion: Expose them to situations (hypothetical or real) that
force them to think on these lines. |
•
|
Provide time and opportunities for reflection: Following
exposure to situations or experiences, it is equally important to
provide a conducive environment, create opportunities and provide
dedicated time to reflect upon them. |
In summary, a structured stepwise approach in
planning a training program using a judicious combination of various
methods in an appropriate sequential or simultaneous manner is
desirable.
Faculty development in teaching and learning of
professionalism serves two main purposes. One, faculty are sensitized to
their role as 'role models' to students and the imbibed curriculum.
Second, it encourages them to consciously adopt one or more methods for
imparting professional values to the students [9]. In India, it may be a
good idea to include a module on professionalism in faculty training
sessions by the Medical education units.
An obvious cognizance of professional behaviour by
authorities (rather than appreciation of only clinical competence) can
be an effective way of setting the expected standards [14]. Positive
acknowledgement of exemplary professional behaviour and punitive action
for unprofessional behaviour will drive home the message well.
Assessment of Professionalism
Assessment is said to be the driving force behind
learning. It directs and guides learning, and provides a degree of
importance to a given area. Professionalism is no exception. Without a
system to assess professionalism, acquisition of professional values
will be rated low in priority [13]. Furthermore, without assessment,
teachers and students will have no yardstick to gauge the level of
learning [21].
There are several impediments to the assessment of
professionalism. The first is the common belief that "professionalism is
caught and not taught". There is no evidence for or against this belief
so far. However, by saying that professionalism is not taught, we accept
the fallout of this idea that this learning is haphazard, not guided by
any specific objectives and not amenable to assessment. This approach is
likely to promote negligence of professionalism in assessment planning.
The second issue is the cultural acceptance (or
non-acceptance) of unprofessional behaviour. In India, so far,
unprofessional behaviour has been viewed rather leniently by society. In
our society, it may be difficult to penalize a student on the basis of
deviations from professional behaviour. Unless society demands strict
professional behaviour from doctors, lapses in professionalism may be
difficult to control. For this, to be effective, we need to identify and
respond appropriately to each unprofessional behaviour [3].
The third issue is our obsession with objectivity in
assessment. Given the present state of our understanding, we may not be
able to objectively measure professionalism. However, we could take
steps to blunt the effect of subjectivity (e.g. by increasing the
number of tests and raters, or by faculty training).
Lastly, behaviour is greatly influenced by the local
context and organizational factors. What is considered professional in
one organization may be considered unprofessional in another [22]. This
explains why we have not been able to develop standardized tools to
assess professionalism. Further, when an institution or a faculty member
in an institution demonstrates unprofessional behaviour and goes
unpunished, then it may really be difficult to penalize students for
similar behaviour. Despite these odds, it is prudent to assess
professionalism.
Many of issues of professionalism faced by doctors or
patients relate to their conduct rather than to their competence. There
is evidence to suggest that since professionalism is learnt, it can be
moulded in a particular direction. This teaching - as argued above -
cannot happen without a supportive assessment. Like assessment of
knowledge and skills, assessment of professionalism has be both,
formative and summative. However, such assessment should be defensible
[23].
What should be assessed under professionalism?
The best way to answer this question is to use
Miller's pyramid and assess each level as appropriate to the stage of
the training (Table I). Thus new students should be
assessed to find out what they know about professionalism, while final
year students and interns may be assessed at the 'shows' and 'does'
levels [22]. It needs to be emphasized that the base of knowledge should
not be undermined, because the students have to first know "what is
professionalism'', before they can demonstrate professional behaviours
in different contexts. This is not to say that assessment should be
limited only to written tests. Assessment should include behavioural
aspects as well.
TABLE I: Tools Used for Assessment of Professionalism
Level of Miller's pyramid
|
Tools
|
|
Does |
Multi Source Feedback (MSF), healthcare outcomes, critical
incident report |
|
Shows |
Observed real or standardized patient encounter (m-CEX; PMEX;
OSCE) |
|
Knows how |
Reflective/narrative portfolio, Case based discussion |
|
Knows |
Multiple Choice Questions (MCQ)/ Short Answer Questions (SAQ)/
Vignettes with professional conflicts |
|
M-CEX-Mini clinical evaluation exercise;
PMEX-Professionalism mini evaluation exercise; OSCE-Objective structured
clinical examination. |
As far as possible, assessment of professionalism
should take place in actual work settings i.e. Workplace-based
Assessment (WPBA) rather than in the controlled artificial settings of
formal examinations [19]. At this juncture, issues of reliability of
workplace based assessment are likely to be raked. However, going by the
experience of using individual tools of WPBA, as well as the composite
program - it should be possible to get fairly reliable results by having
6-8 assessments per year by different assessors [24]. In the beginning,
for several years, such assessments will happen only for formative
purposes. This is useful, as here one does not aim for a very high
reliability. Experience and faculty training will also help to improve
the reliability of such assessments [25].
Vague definitions and lack of unanimous standards may
make the assessment of professionalism challenging. Additionally, some
teachers may be hesitant to give negative ratings, while others may tend
to inflate summative ratings (like what happens with internal assessment
now). However, these kinds of issues should not be taken against
professionalism, as we happily accept the assessment of knowledge and
skills by the same teachers, many of whom are likely to be as much
influenced by the conflict in the role of a teacher and an assessor.
It may be worthwhile to relook at the concept of
utility of assessment, which is a notional concept and is represented as
a product of its validity, reliability, feasibility, acceptability and
educational impact [26]. Assessments which are low on one parameter can
still be very useful by being high on others. Even though numerical
reliability of professionalism assessment might be low, its educational
impact can be fairly high. Relative importance to various attributes of
assessment should be guided by purpose of assessment rather than by a
pursuit of objectivity.
Tools for assessing professionalism
Professionalism is a multi-dimensional concept and no
single tool may be able to capture it in entirety. A number of tools
have been developed for assessing professionalism (Table I).
These include observing patient encounters (mini-CEX, professionalism
mini assessment tool PMEX, standardized direct observation tool);
simulations (OSCE using standardized patients); reporting of
unprofessional incidents (critical incident method); paper and pencil
tests (MCQs, critical incident reports); observer ratings (multi source
feedback, global ratings); self-reported scales and patient satisfaction
surveys [14,19]. We need to select the appropriate tools from this
toolkit to suit our purpose.
Most of the tools mentioned above have been described
in an earlier paper on WPBA [27]. However, PMEX needs some elaboration.
It is a structured observation tool and consists of 21 items, each of
which is rated on a 4 point scale (unacceptable, below expectations, met
expectations and exceeded expectations) [28]. In addition, it has space
for recording of an incident which has shown a clear breach of
professional boundaries. The assessment is discussed with the trainee,
who signs the form at the end of this discussion. The forms become a
part of the learning portfolio and can be used to show the development
of professionalism over a period of time [23]. Factor analysis has
confirmed that it assesses four important factors viz. doctor-patient
relationship, reflection, time management and inter-professional
relationship. A generalizability coefficient of 0.82 (SEM 0.08) is
attainable by 12 forms [28].
Assessment of professionalism needs to be linked to
the overarching assessment of knowledge and skills. While it usually
remains formative, it may need to be made summative, especially at
decision points (e.g. graduation). Compilation of data over a period of
time should help students to attempt to acquire professional values in
areas found lacking and also help teachers to take remedial action.
Irrespective of which tool is used for assessment of professionalism,
the basic premise remains the same i.e. direct observation in authentic
settings followed by feedback and an opportunity to reflect. While there
may not be a consensus on the best tool for assessing professionalism,
there is agreement on the fact that without solid assessment tools,
questions about the efficacy of approaches to educating learners about
professional behaviour will not be effectively answered [24].
A model blueprint for learning and assessing
professionalism in the Indian scenario (for undergraduates) is proposed
in Table II. It is possible to incorporate assessment of various
elements of professionalism in the existent internal assessment
programs, and its reliability can be improved by adopting the Quarter
model of In-training Assessment [29].
Conclusions
Professionalism is integral to the medical profession
and it should be an explicit part of the medical curriculum. Each
country and institution needs to develop its own definition of
professionalism, according to the societal norms of the times and
identify the core elements of professionalism. A judicious combination
of teaching and learning methods need to be incorporated in a
longitudinal manner using a stepwise approach to teach professional
values to students of all levels. Assessment of professionalism needs
priority for it to be taken seriously. Assessment of professionalism is
best done in authentic workplace-based settings, where supervisors have
an opportunity to provide feedback after direct observation of students
and allow them a chance to reflect on their behaviour.
1. Sohl P, Bassford HA. Codes of medical ethics:
Traditional foundations and contemporary practice. Social Sci Med.
1986;22:1175-9.
2. van Mook WK, van Luijk SJ, O'Sullivan H, Wass V,
Zwaveling JH, Schuwirth LW, et al. The concepts of professionalism and
professional behaviour: Conflicts in both definition and learning
outcomes. Eur J Intern Med. 2009;20:e85-9.
3. van Mook WN, Gorter SL, De Grave WS, van Lujk SJ,
Wass V, Zwaveling JH, et al. Bad apples spoil the barrel: Addressing
unprofessional behavior. Med Teach. 2010;32:891-8.
4. Papadakis MA, Arnold GK, Blank LL, Holmboe ES,
Lipner RS. Performance during internal medicine residency training and
subse- quent disciplinary action by state licensing boards. Ann Intern
Med. 2008;148:869-76.
5. Regulations on Graduate Medical Education 1997.
Medical Council of India website. Available from:http://www.mciindia.org/Rules-and-Regulation/GME_REGULATIONS.pdf.
Accessed June 22, 2014.
6. Medical Council of India. Post Graduate Medical
Education Regulations 2000. Available from: http://www. mciindia.org/RulesandRegulations/PGMedical
EducationRegulations2000.aspx. Accessed July 8, 2014.
7. Epstein RM, Hundert EM. Defining and assessing
professional competence. JAMA. 2002;287:226-35.
8. O'Sullivan H, Van Mook W, Fewtrell R, Wass V.
Integrating professionalism into the curriculum: AMEE Guide No. 61. Med
Teach. 2012;34:e64-7.
9. Steinert Y, Cruess S, Cruess R, Snell L. Faculty
development for teaching and evaluating professionalism: from programme
design to curriculum change. Med Educ. 2005;39:127-36.
10. Madhok R. The Global Indian Doctor: Workshop on
Promoting Professionalism and Ethics - Brief Notes and Next Steps. 2014
Jan 10; Kolkata, India. Available
from:http://leadershipforhealth.com/wp-content/uploads/2014/02/Event-report.pdf
Accessed September 29, 2014.
11. Hawkins RE, Katsufrakis, Holtman MC, Clauser BE.
Assessment of medical professionalism: Who, what, when, where, how, and
…why? Med Teach. 2009; 31:348-61
12. Cruess SR, Cruess RL. Professionalism must be
taught. BMJ. 1997;315:1674-6.
13. Ponnamperuma G, Ker J, Davis M. Medical
professionalism: Teaching, learning, and assessment. South East Asian
Journal of Medical Education. 2007;1:42-8.
14. Wilkinson TJ, Wade Wb, Knock LD. A blueprint to
assess professionalism: Results of a systematic review. Acad Med.
2009;84:551-8.
15. Goldie J. Integrating professionalism teaching
into undergraduate medical education in the UK setting. Med Teach.
2008;30:513-27.
16. Cruess SR, Cruess RL. Teaching professionalism -
Why, what and how? Facts Views Vis Obgyn. 2012;4:259-65.
17. Jochemsen-van der Leeuw HG1, van Dijk N, van
Etten-Jamaludin FS, Wieringa-de Waard M. The attributes of the clinical
trainer as a role model: A systematic review. Acad Med. 2013;88:26-34.
18. Cruess R, Cruess S. Teaching professionalism:
General principles. Med Teach. 2006;28:205-8.
19. Passi V, Doug M, Peile E, Thistlethwaite J,
Johnson N. Developing medical professionalism in future doctors: A
systematic review. Int J Med Educ. 2010;1:19-29.
20. Perry M, Maffuli N, Wilson S, Morrissey D. The
effectiveness of art-based interventions in medical education: A
literature review. Med Educ. 2011;45:141-8.
21. Arnold L. Assessing professional behaviour:
Yesterday, today and tomorrow. Acad Med. 2002;77:502-15.
22. Goldie J. Assessment of professionalism:
Consolidation of current thinking. Med Teach. 2013;35:e952-6.
23. Hodges BD, Ginsburg S, Cruess R, Cruess S,
Delport R, Hafferty F, et al. Assessment of professionalism:
Recommendations from the Ottawa 2010 conference. Med Teach.
2011;33:354-63.
24. Norcini J, Burch V. Workplace-based assessment as
an educational tool: AMEE Guide No.31. 2007;29:855-71.
25. Adkoli BV. Assessment of Professionalism and
Ethics. In Principles of Assessment in Medical Education. (Ed: Singh T,
Anshu) Jaypee Brothers Medical Publishers. New Delhi. 2012:.p. 180-190.
26. van der Vleuten CPM. The assessment of
professional competence: Developments, research and practical
implications. Adv Health Sci Educ. 1996;1:41-67.
27. Singh T, Modi JN. Workplace-based Assessment: A
step to promote competency based postgraduate training. Indian Pediatr.
2013;50:553-9.
28. Cruess R, McLlroy JH, Cruess S, Ginsburg S,
Steinert Y. The professionalism mini-evaluation exercise: A preliminary
investigation. Acad Med. 2006;81:S74-8.
29. Singh T, Anshu, Modi JN. The Quarter Model: A
proposed approach for in-training assessment of undergraduate students
in Indian medical schools. Indian Pediatr. 2012;49:871-8.

