|
|
|
Indian Pediatr 2014;51: 863-868 |
 |
Programmatic Response to Malnutrition in
India: Room for More Than One Elephant?
|
|
Rajib Dasgupta, Dipa Sinha and Veda Yumnam
From Center of Social Medicine & Community Health,
Jawaharlal Nehru University, New Delhi, India.
Correspondence to: Dr Rajib Dasgupta, Centre of Social
Medicine & Community Health, Jawaharlal Nehru University, New Delhi 110
067, India.
Email: [email protected]
|
Programming platforms need to
recognize the diversity of malnutrition epidemiology in India and
choose appropriate implementation designs. With severe chronic
malnutrition as the dominant epidemiologic entity, the net needs to
be cast wide, focusing on: food security, health care, agriculture,
water and sanitation, livelihoods and women’s empowerment.
Community-based malnutrition treatment and prevention programs need
to collaborate to complement treatment with socioeconomic and
preventive interventions. Expansion of nutrition rehabilitation
centers should be limited to areas/districts with high wasting.
Pediatric services with nested nutrition services (including
counseling) requires urgent strengthening. Continuum of Care is a
weak link and requires strengthening to make both hospital and
community-based models meaningful.
Keywords: Nutrition, Prevention, Protein
energy malnutrition, Rehabilitation.
|
|
T
he modest decline of undernutrition levels
between the last two rounds of the National Family Health Survey is well
known and India continues to remain off-track from the Millennium
Development Goal (MDG-1) target. The third National Family Health Survey
(NFHS-3) reported 6.4% under-five children in India as severely wasted
and 19.8% as wasted, translating to about 8.1 million children with
severe acute malnutrition (SAM) [1]. The efficacy of WHO guidelines and
regimens for reduction of mortality through hospitalized management of
SAM children in Africa (compared with conventional treatment) is well
established [2-4]. This led to Nutritional Rehabilitation Centers (NRC)
/ Malnutrition Treatment Centers (MTC) emerging as the strategy of
choice in India for institutionalized management of malnourished
children. More recently, the global consensus is shifting towards
community-based management of acute malnutrition for uncomplicated cases
of SAM (estimated to be about 85% of all SAM cases). This is also based
on African experiences of treating acute malnutrition by large scale use
of ready to use therapeutic foods (RUTF) in community settings [5,6].
Efforts are ongoing in India to frame guidelines for community-based
management of acute malnutrition [7].
Severe Chronic Malnutrition: Saying the Unsaid
Examination of SAM management in India through NRCs
draws attention to three key issues: (i) need for community based
strategies that take a continuum of care approach addressing all
children [8]; (ii) inappropriateness of current cut-offs of mid
upper arm circumference (MUAC) measurement as a screening tool for
identification [9]; and (iii) poor treatment outcomes at NRCs in
terms of recovery, cure, defaulter and secondary failure rates [10]. We
have argued that stunting levels in India are higher than African
children and exceedingly so among chronically poor populations. Put
differently, there is a uniquely high prevalence of both stunting and
wasting; both SAM and Severe Chronic Malnutrition (SCM) co-exist,
and, SCM is the dominant epidemiologic entity.
In the light of the emerging evidence, this paper
pursues two specific objectives: (i) re-examine national level
data to deconstruct the distribution of SAM/SCM scenario – this is
relevant for a layered understanding of the inter-state distribution of
wasting and stunting; and (ii) examine whether programmatic
responses are consistent with epidemiologic realities.
Bergeron and Castleman examined the phenomenon of
acute and chronic malnutrition often coexisting in same locations
[11,12]. They established that the type and severity of malnutrition
vary within countries, and responses at sub-national levels ought to
depend on the specific nutrition situation and other factors such as
health system capacity, food availability, enabling environment and
resource availability. India, along with D R Congo, Ethiopia, Nepal,
Nicaragua, and Niger were found to have high rates of both stunting and
wasting.
Following their methodology, we have undertaken an
analysis of the Indian NFHS-3 data to map inter-state distribution of
acute and chronic malnutrition by computing terciles for wasting and
stunting.
Distribution of Wasting and Stunting
Distribution of wasting vs. stunting across
states is uneven. The results presented (Table I) is the
distribution for rural areas while that for the ‘total’ is closely
similar. Large states, with high levels of chronic poverty – Bihar,
Jharkhand and Madhya Pradesh – also have high levels of both
stunting and wasting. States with high levels of stunting (including
large states such as Assam, Uttar Pradesh, West Bengal, Chhattisgarh,
Gujarat, Karnataka and Maharashtra) are evenly spread among low, medium
and high wasting terciles. However, there are no states that show high
wasting but low stunting. While there are a large number of states with
high or medium stunting, only a few have high wasting and these are the
ones with concomitant high stunting. On the other hand, states with
medium prevalence of wasting are spread across low, medium and high
stunting prevalence. It thus becomes fairly apparent that stunting and
SCM is the dominant epidemiologic entity. Consequently, the phenomenon
of wasting, typically an acute phenomenon in terms of weight loss due to
short term causes merits clarity in the Indian context.
TABLE I Inter-state Distribution of Wasting and Stunting Among Children Under 5 Years
|
Stunting
|
Wasting (-2WHZ)[Tercile] |
|
(-2HAZ) [Tercile]
|
Low |
Medium |
High |
|
Low |
Goa, Jammu & Kashmir,
|
Kerala, Tamil Nadu, Tripura |
– |
|
Med |
Andhra Pradesh, AP |
HP, Orissa, Rajasthan
|
– |
|
Manipur, Nagaland, Punjab, Sikkim |
|
|
|
High |
Assam, Delhi, Mizoram, UP, |
Chhattisgarh, Gujarat, Haryana, |
Bihar, Jharkhand, |
|
West Bengal |
Karnataka, Maharashtra, Uttaranchal
|
MP, Meghalaya |
|
Data source: [1]; MP: Madhya Pradesh; UP: Uttar Pradesh; HP:
Himachal Pradesh; AP: Arunachal Pradesh. |
Programmatic Responses to Severe Malnutrition
The main strategy for treatment of severe
malnutrition (all such cases being assumed and labelled as ‘SAM’)
in India has primarily been facility-based; a number of Nutrition
Rehabilitation Centers (NRC) / Malnutrition Treatment Centers (MTC) have
been set up across the country, especially in high priority states under
the National Rural Health Mission (NRHM). There is emerging evidence of
these models meeting with poor success in these states. Outcome data
from hospital- based treatment centers in countries (such as Burkina
Faso) with high levels of both stunting and wasting have revealed that a
small proportion actually qualify for admission, implying that the
dominant epidemiologic entity is SCM; low recovery rates also complement
this thesis [10,13-15]. It is no coincidence that these poorest Indian
states by the UNDP’s Multi-dimensional Poverty Index (MPI) have both
high stunting and wasting and are comparable to the African countries in
terms of high stunting and wasting, MPI scores as well as poor SAM
treatment outcomes [10,11,16]. It has been argued that poor treatment
outcomes are pathognomonic of a basic flaw in the approach itself
(failure to recognize SCM as an epidemiological entity) and not a marker
of poor implementation [10].
Towards Community-Based Management of Acute
Malnutrition
There is renewed thinking on facility-based
treatment, with opinion gradually veering towards Community-Based
Management of Acute Nutrition (CMAM) as a cost-effective high-impact
model. Hospital-based management of SAM lasts for 2-3 weeks (plus
follow-up) and involve substantial burden including opportunity costs
and social dislocation; CMAM offers an attractive alternative to these
challenges. CMAM comprises of three key elements: (i)
ready-to-use therapeutic food (RUTF), (ii) community engagement
and mobilization, and (iii) screening for malnutrition in
communities [17,18]. There are three treatment modalities: (i)
inpatient management at the stabilization center established near target
communities, (ii) outpatient management, and (iii)
supplementary feeding; the appropriate choice is dependent on the
severity of malnutrition and its associated complications. In India,
Bihar has initiated a CMAM program with technical support from
Médecins Sans Frontières; children are given take-home
ready-to-use therapeutic food (RUTF), following a model similar to that
the organization pursues in Africa [19].
Drawing upon the WHO UNICEF Joint Statement, the
Indian Academy of Pediatrics (IAP) Consensus Statement 2013 also
advocated that children with SAM who do not have any criterion for
inpatient-care can be managed under an Outpatient therapeutic program
(OTP) center close to the child’s home and that such a program needs to
be a part of the current health service system, viz. Integrated
Child Development Scheme (ICDS) and the National Rural Health Mission
(NRHM) and involve frontline health worker cadres such as the
Anganwadi Worker (AWW), Accredited Social Health Activist (ASHA) and
the Auxiliary Nurse Midwife (ANM) [20, 21]. The National Guidelines of
Bangladesh are also pursuing a similar line [22]. DFID-UK, adapting from
the African models, is providing technical support for piloting CMAM in
Madhya Pradesh and Odisha [23].
The Rajmata Jijau Mother-Child Health and Nutrition
Mission in Maharashtra has adopted a three tier system: (i)
Village Child Development Center (VCDC) for community-based management
of SAM, (ii) Child Treatment Centre (CTC) for facility-based
management of SAM/MAM children (at PHC level), and (iii)
Nutrition Rehabilitation Centre (NRC) for facility-based management of
SAM/MAM children (at the level of Rural/District Hospital). Analysis of
the program data revealed relapse "due to lack of adequate training of
mothers". The program thus decided to switch to a ‘Home-based VCDC
model’ [24].
Most of these CMAM projects are yet to be
systematically evaluated, specifically for their impact in the context
of high prevalence of stunting. We do not have adequate information on
either proximate outcomes such as mortality and failure rates, or long
term ones such as relapse rates.
Paradoxes and Dilemmas
SAM is precipitated by acute crises situations such
as deprivation due to seasonal shortages, sudden catastrophes such as
crop failure or civilian unrest, and acute episodic illnesses. SAM,
associated with a high risk of mortality, constitutes both medical and
humanitarian emergencies. SCM, in contrast, is an outcome of latent
poverty, chronic food insecurity, poor feeding practices and protracted
morbidities with long term implications for educability, future work
capacity, earning capabilities and susceptibility to chronic diseases.
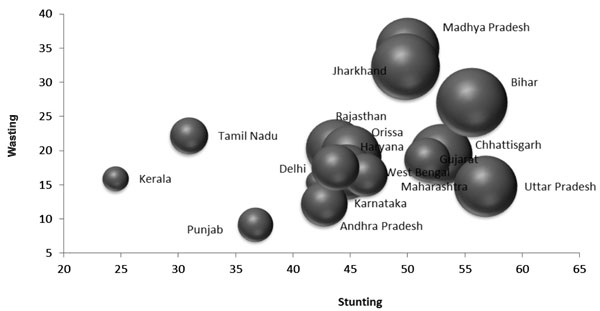
Fig. 1 captures the inter-relationship of the
anthropometric indicators (from NFHS-3) and the Multi-Dimensional
Poverty Index (MPI) scores for the major Indian states [16]. The size of
the bubbles represents MPI scores and correlate well with the
distribution expounded in Table I. SCM thus represents
profound individual and societal deprivations but is rarely a
direct cause of mortality (the raison d’être of facility-based
treatment models) [10,11].
 |
|
Fig. 1 Anthropometric indicators
and Multi-dimensional Poverty Index (MPI) scores for major
Indian states.
|
In situations of SAM with high probability of
mortality, the treatment of choice is a clinical/facility-based approach
[11,20] CMAM with its advantages over the NRC model is being
increasingly propagated for SAM management in India. However, this is on
account of a relatively small proportion of children who meet the
admission criteria for NRCs, or are sick and at a high risk of mortality
– largely because they are cases of SCM [10]. The current programmatic
choices in India are limited to either the NRC/MTC approach or the CMAM
approach, barring some isolated projects with multi-sectoral components.
Thus, the questions arises: Are NRC/MTC and/or CMAM appropriate
strategies for states/population with high levels of chronic
malnutrition? Put differently, to what extent and in what manner can
these approaches (essentially designed to address acute malnutrition)
deal with the epidemiologic reality of SCM?
Programmatic interventions for SCM require a far
wider spectrum of interventions beyond clinical management and need to
focus on multi-sectoral actions (to combat multi-dimensional
deprivations) for promoting adoption of practices to improve quality of
local diets, improving child feeding practices, and reducing exposure to
illnesses; these imply broad-based commitment of resources and local
capacities and leaderships (requiring sustained nurturing) are critical
[25].
The key indicator for SCM is height/age while those
for SAM include weight/height or MUAC. The Integrated Child Development
Services (ICDS), however, uses weight/age for identification of SAM
which has been shown to be a poor proxy [8]. While correlation between
weight/age and height/age is generally understood to be high, they
measure different outcomes. Significantly, whether or not weight/age is
a good screening method for stunting in chronically poor populations,
and in the lack of pediatric body composition data, has not been
convincingly tested [13]. SCM, therefore, lacks a good screening tool at
the field level while calling for community based preventive and multi-sectoral
programs.
The Way Forward
CMAM and prevention programs need to collaborate to
complement treatment services with socio-economic and other preventive
interventions. This is often hindered by strategic and technical divides
between diverse departments and organizations that need to collaborate
very closely. Further, there is evidence that donor priorities may
choose one intervention over the other [25]. There is an urgent need for
‘tailored’ strategies for different states, and specifically districts,
depending on their wasting and stunting profiles. This calls for
investing in obtaining appropriate data (as a starting point) including
regular nutrition surveillance at the district level.
Expansion of NRCs in states with low or medium
wasting is unwarranted. Strengthening pediatric services and nesting
nutrition services (including counseling) within such settings ought to
be the preferred strategy. In states/districts with high wasting, there
is a need to shift to more community-based strategies (including CMAM),
while NRCs may take care of complicated cases. At the same time doctors
and pediatricians need to move beyond their perception of NRCs as a
‘feeding program’ and engage more with treatment of sick children and
minimize referral [10]. Continuum of care (CoC) is weak and fails to
sustain weight gains made during the stay at the NRC. While shift to
community based models is in general desirable, CoC requires
considerable strengthening to make both hospital- and community- based
interventions meaningful [26].
Emerging evidence from village studies in areas with
chronic malnutrition indicate variation in availability, consumption and
composition of food across households depending on their resource base –
a constant struggle to produce, earn and procure food; as well as
seasonal variation in food availability and dietary intake within
households. Such populations suffer from chronic food insecurity,
worsening during lean seasons that are marked additionally by higher
levels of: (i) growth faltering; (ii) referrals for
nutritional rehabilitation and illnesses; and (iii) mortality
among children [27].
While chronic malnutrition during the rest of the
year signifies children who are hungry and not sick, these lean seasons
are periods of crisis that bring into focus episodes of wasting (acute
malnutrition) over and above underlying stunting (chronic malnutrition).
We propose that this phenomenon be recognized as an acute-on-chronic
category of malnutrition; such acute-on-chronic entities (beyond the
conventional dichotomous categories of acute and chronic) are
increasingly recognized in other conditions such as acute-on-chronic
liver failure and acute-on-chronic kidney disease.
These windows (of crisis) require not just nutrition
rehabilitative services (CMAM or NRC) but, more importantly, have
greater need for pediatric care too; shortfall of pediatricians range up
to 90-95% in rural and tribal areas of states with high malnutrition.
Management of chronic malnutrition calls for
sustained interventions addressing all children. Universal growth
monitoring, protocols of addressing growth faltering with referrals for
treatment of illnesses, prevention of infections, and feeding
calorie-dense foods are essential direct interventions. Women’s
workforce participation (both paid and unpaid) is high and contributes
to poor child care and feeding practices. With the Integrated Child
Development Services (ICDS) continuing to lag in its quest for ‘universalization
with quality’, the lack of adequate child care/ day-care/ crèche- based
services for children under three years of age contributes to worsening
chronic malnutrition.
A crèche program with components of community
mobilization backed by systems strengthening and access to better food
and livelihoods can help ameliorate the situation. The Fulwari
Scheme in Chhattisgarh has been independently assessed to demonstrate
improvement of anthropometric indicators through multi-sectoral actions:
feeding and care of under-three children, pregnant and lactating women;
day-care for children; promotion of household level production of
diverse foods; and panchayatled strengthening of health, ICDS and
agricultural sectors [28]. The Action Against Malnutrition (AAM) project
being implemented by a consortium of NGOs in seven blocks of states with
high SCM is also seeking to address these elements; results are awaited
regarding its efficacy [29].
Concluding Thoughts
Contemporary wisdom maintains that the distinction
between acute and chronic malnutrition is blurred; and that mortality is
high in chronic malnutrition as well [30]. Rigid and blinkered, such
arguments are at best intuitive but oblivious to the epidemiology of
chronic malnutrition in India. A reductionist zeal considers ‘SAM’ in
India as ‘a major public health issue’, the proverbial elephant in the
room; first offering NRCs as a solution and now CMAM, little realizing
that the epidemiology is complex and the need to recognize other
elephants too [21]. The international dogma of SAM is a powerful idea
with a compelling logic for urgent technical and humanitarian action;
the consequences for our context: they distract attention and resources
away from the big picture. Seemingly obvious observations come with a
caution: it looks exactly the same whether the earth goes around the
sun, or, had the sun been going around the earth!
Our previous analyses point to three clear
conclusions: (i) differences in the anthropometric ‘spread’ of
malnutrition across different states of India (and the need for tailored
strategies); (ii) SCM and stunting (and not MAM/SAM) as an
overwhelmingly large epidemiologic reality; and, (iii) episodes
of wasting (acute malnutrition) as a seasonally nested entity within
chronic malnutrition, what we term acute-on-chronic malnutrition. The
challenge is to arrive at the common purpose of tackling SCM over and
above sectoral priorities. Recognizing and addressing these complexities
are both programmatic and ethical imperatives.
Acknowledgements: This work was supported by a
grant of the Indian Council of Medical Research (ICMR). Sincere thanks
to: Dr Vandana Prasad and Dr Ganapathy Murugan, PHRN, New Delhi; Mr
Haldhar Mahato, PHRN Jharkhand; Mr Sachin Jain, Vikas Samvad, Bhopal. Ms
Shalini Ahuja, New Delhi deserves special appreciation for her all-round
support.
An earlier version of this paper was presented at the
South Asia Conference on Policies and Practices to Improve Nutrition
Security, July 30-31, 2014, New Delhi.
Contributors: RD: conceptualized and led the
study. All authors participated in data collection, analysis, manuscript
writing and approved the final draft.
Funding: Indian Council of Medical Research,
Grant No.: PAC-SSS-RD-ICMR-017120714-688. Competing Interests:
None stated. Ethics Approval: JNU IERB
References
1. International Institute for Population Sciences
(IIPS) and Macro International. 2007. National Family Health Survey
(NFHS-3), 2005-06;I:273.
2. Ashworth A, Chopra M, McCoy D, Sanders D, Jackson
D, Karaolis N, et al. WHO guidelines for management of severe
malnutrition in rural South African hospitals: effect on case fatality
and the influence of operational factors. Lancet. 2004;363:1110-5.
3. Deen JL, Funk M, Guevara VC, Saloojee H, Doe JY,
Palmer A, Weber MW. Implementation of WHO guidelines on management of
severe malnutrition in hospitals in Africa. Bull World Health Org.
2003;81:237-43.
4. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K,
Giugliani E, et al. Maternal and Child Undernutrition Study
Group. What works? Interventions for maternal and child undernutrition
and survival. Lancet. 2008;371:417-40.
5. Dibari F, Bahwere P, Huerga H, Irena AH, Owino V,
Collins S, et al. Development of a cross-over randomized trial
method to determine the acceptability and safety of novel ready-to-use
therapeutic foods. Nutrition. 2013;29:107-12.
6. Community Based Management of Severe Acute
Malnutrition. A Joint Statement by the World Health Organization, the
World Food Programme, the United Nations System Standing Committee on
Nutrition and the United Nations Children’s Fund. Available from:
http://www.cmamforum.org/Pool/Resources/Community-based-management-of-acute-malnutrition-Joint-Statement-WHO-SCN-UNICEF-2007.pdf.
Accessed June 29, 2014.
7. Community based management of Acute Malnutrition.
Proposal for the Community-based Management of SAM in Madhya Pradesh.
Available from:
http://www.cmamforum.org/Pool/Resources/India-Madhya-Pradesh-management-of-acute-maln-OP-GUIDELINES-2012.pdf.
Accessed June 29, 2014.
8. Prasad V, Sinha D, Sridhar S. Falling between two
stools: operational inconsistencies between ICDS and NRHM in the
management of severe malnutrition. Indian Pediatr. 2012;49:181-5.
9. Dasgupta R, Sinha D, Jain S, Prasad V. Screening
for SAM in the community: Is MUAC a ‘simple tool’? Indian Pediatr.
2013;50:154-5.
10. Dasgupta R, Ahuja S, Yumnam V. Can Nutrition
Rehabilitation Centers Address Severe Malnutrition in India? Indian
Pediatr. 2014;51:95-9.
11. Bergeron G, Castleman T. Program responses to
acute and chronic malnutrition: divergences and convergences. Adv Nutr.
2012;3:242-9.
12. Richard SA, Black RE, Checkley W. Revisiting the
relationship of weight and height in early childhood. Adv Nutr.
2011;3:250-4.
13. Somassé YE, Bahwere P, Laokri S, Elmoussaoui N,
Donnen P. Sustainability and scaling-up analysis of community-based
management of acute malnutrition: lessons learned from Burkina Faso.Food
Nutr Bull. 2013;34:338-48.
14. Collins S, Sadler K. Outpatient care for severely
malnourished children in emergency relief programmes: A retrospective
cohort study. Lancet. 2002; 360:1824-30.
15. Taneja G, Dixit S, Khatri AK, Yesikar V,
Raghunath D, Chourasiya S. A study to evaluate the effect of
intervention measures on admitted children in selected nutrition
rehabilitation centres of Indore and Ujjain divisions of the state of
Madhya Pradesh (India). Indian J Community Med. 2012;37:107-15.
16. Alkire S, Santos ME. Acute Multidimensional
Poverty: A New Index for Developing Countries. United Nations
Development Programme Human Development Reports Research Paper 2010.
17. Park SE, Kim S, Ouma C, Loha M, Wierzba TF, Beck
NS. Community management of acute malnutrition in the developing World.
Pediatr Gastroenterol Hepatol Nutr. 2012;15:210-9.
18. Brown KH, Nyirandutiye DH, Jungjohann S.
Management of children with acute malnutrition in resource-poor
settings.Nat Rev Endocrinol. 2009;5:597-603.
19. Medecins Sans Frontiers. India: A step
closer to effective treatment of severe acute malnutrition in Bihar.
Available from:
http://www.msf.org/article/india-step-closer-effective
-treatment-severe-acute-malnutrition-bihar. Accessed April 26, 2014.
20. WHO, UNICEF. WHO child growth standards and the
identification of severe acute malnutrition in infants and children A
Joint Statement by the World Health Organization and the United Nations
Children’s Fund, 2012.
21. Dalwai S, Choudhury P, Bavedkar SB, Dalal R,
Kapil U, Dubey AP, et al. Consensus Statement of the Indian
Academy of Pediatrics on integrated management of severe acute
malnutrition. Indian Pediatr. 2013;50:399-404.
22. National Guidelines for the Management of
Severely Malnourished Children in Bangladesh. Available from:
http://www.unicef.org/bangladesh/SAM_Guideline.pdf. Accessed May 04,
2014.
23. DFID. Scaling up community based management of
acute malnutrition; but doing it differently. Available from:
www.coverage-monitoring.org. Accessed May 01, 2014.
24. Government of Maharashtra. Home based VCDC model.
Available from:
http://www.nutritionmissionmah.gov.in/Site/Common/homebasedVCDC.aspx.
Accessed May 02, 2014.
25. FANTA-2. Title II Technical Reference Materials.
TRM-01: Preventing Malnutrition in Children under 2 Approach (PM2A): A
Food-assisted Approach. Revised November 2010; Washington, DC: Food and
Nutrition Technical Assistance II Project (FANTA-2).
26. Dasgupta R, Yumnam V, Ahuja S, Roy S. The
Conundrum of continuum of care: Experiences from the NRC model, Madhya
Pradesh. Oral presentation at the South Asia Conference on Policies and
Practices to Improve Nutrition Security, SAC-OP-07-05; 2014 July 30-31,
New Delhi, India. Available from:
http://www.nutritioncoalition.in/thematic-oral-presentations.
Accessed June 16, 2014.
27. Chaand I, Dasgupta R. Mapping transitions in food
insecurity in ‘pure’ tribal villages: village studies in Latehar,
Jharkhand. Poster presentation at the South Asia Conference on Policies
and Practices to Improve Nutrition Security, SAC-PP-01-04; 2014 July
30-31, New Delhi, India. Available from:
http://www.nutritioncoalition.in/thematic-poster-presentations.
Accessed June 16, 2014.
28. Garg S, Mishra JP. Caregiver Managed Nutrition
and Day Care Centres Panchayat-Led Fulwari Scheme of Chhattisgarh State.
Oral presentation at the South Asia Conference on Policies and Practices
to Improve Nutrition Security, SAC-OP-07-02; 2014 July 30-31, New Delhi,
India. Available from:
http://www.nutritioncoalition.in/thematic-oral-presentations.
Accessed June 16, 2014.
29. Action Against Malnutrition: A multi-strategy
intervention in six blocks of three states. Available from:
http://www. phrnindia.org/our_work/actionAgainst Malnutrition.html.
Accessed June 16, 2014
30. World Bank. Improving Nutrition Through
Multisectoral Approaches. 2013. Available from:
file:///C:/Users/a/Downloads/751020WP0Impro00Box374299B00 PUBLIC0.pdf
. Accessed May 12, 2014.
|
|
|
|
|
 |
|

