|
|
|
Indian Pediatr 2012;49:
889-895 |
 |
Risk Factors for Mortality in Community
–Acquired Pneumonia Among Children Aged 1-59 Months Admitted in
a Referral Hospital
|
|
Padmanabhan Ramachandran, Krishnamoorthi Nedunchelian, Appasamy
Vengatesan and
Saradha Suresh
From the Institute of Child Health and Hospital for
Children, Egmore, Chennai, Tamilnadu.
Correspondence to: Dr P Ramachandran, G3 Murugan
Apartments, #18 Sivasailam Street, T Nagar, Chennai, Tamilnadu 600 017,
India. [email protected]
Received: October 27, 2010;
Initial review: December 21, 2010;
Accepted: February 07, 2012.
Published
online: 2012, March 30.
PII:S09747559100381-1
|
|
Objective: To determine the case fatality rate and factors for death
in community acquired pneumonia among children aged 1 month to 59 months
admitted in a referral Hospital.
Design: Hospital based retrospective study.
Setting: Institute of Child Health and Hospital
for Children, Chennai.
Patients: Case records of children aged 1 month
to 59 months of age with pneumonia (clinically diagnosed pneumonia,
radiologically diagnosed pneumonia, and clinically and radiologically
diagnosed pneumonia), from January 2006 to December 2008.
Outcome measures Case fatality rate (CFR) was
calculated. Risk factors for mortality analyzed were young age of 1 to 6
months old, female sex, wheeze, respiratory rate
³70/min,
chest indrawing, altered level of consciousness, convulsions, shock,
associated heart disease, recent measles, weight for age <-2 Z
score and need for assisted ventilation. The association of risk factors
to mortality was arrived at for all three categories of pneumonia cases
separately.
Results: Case fatality rate was 8.2% (95% CI:
7.37- 8.99%). There was no significant difference in the CFR among the
three study groups. Need for assisted ventilation alone was found to be
an independent risk factor for mortality in children with pneumonia
among all the study groups. Other risk factors like young age, weight
for age <-2 Z score, altered level of consciousness, and
congenital heart disease were also observed among these groups.
Conclusion: Among 1 month to 59 months old
hospitalized children with pneumonia, CFR was 8.2%. Need for assisted
ventilation was a significant risk factor associated with mortality.
Key words: Case fatality rate, Children, Community acquired
pneumonia, Risk factors.
|
|
Pneumonia is one of the leading causes of
mortality among under five children in most developing countries. It is
estimated to cause 1.9 million deaths each year [1]. According to
official estimate from the WHO for the year 2000, two thirds of all
these deaths were in just 10 countries and were maximum in India [2].
More than 20% of world’s pneumonia deaths still occur in India,
resulting in greater than 370,000 child deaths annually [3]. Different
studies, both community as well as hospital based, have highlighted a
variety of factors contributing to mortality in childhood pneumonia such
as young age, low birth weight, under nutrition, anemia, lack of
parental education, overcrowding, pollution at home, lack of exclusive
breast feeding, lack of measles immunization, and severe disease at
presentation [4-9]. With socio-economic progress and improvement in
health awareness and referral services, an increasing proportion of
pneumonia deaths will occur in hospitals [7]. Hence, the profile of
pneumonia in tertiary care centers is likely to reflect the burden in
the community. Only a few studies have performed such an evaluation in
developing countries [4, 9-11]. More studies are required to analyze the
contributing factors for mortality in childhood pneumonia in young
children. This information may help in optimal utilization of scarce
resources for the most effective preventive and early management
strategies. Data on pneumonia from sentinel centres may also serve as
baseline information to assess the trend when some of the vaccines such
as pneumococcal and H. influenzae type b vaccines are introduced
in the national immunization program. We conducted a retrospective study
on pneumonia among children aged 1 month to 59 months admitted in a
tertiary care hospital, to determine the case fatality rate and factors
responsible for death.
Methods
Institute of Child Health and Hospital for Children,
Chennai is a referral pediatric institute and a 537 bedded
multi-specialty hospital attached to Madras Medical College, Chennai. It
caters to health needs of children up to 12 years of age from the city
of Chennai and neighbouring districts. We conducted a retrospective
chart review of all children in the age group of 1 month to 59 months
admitted between January 2006 and December 2008 in our hospital with a
final diagnosis of pneumonia. These cases were classified in to 3 groups
(i) clinically diagnosed pneumonia {WHO diagnostic criteria for
pneumonia (fast breathing defined by respiratory rate
≥60/min in <2 months
of age,
≥50/min
in 2- 11 months of age and
≥40/min
in 12-59 months of age) or severe pneumonia (pneumonia with chest
retraction) as per IMCI guidelines} [12], (ii)
radiologically diagnosed pneumonia (based on the consensus finding of
chest infiltrate(s) by a qualified radiologist and treating clinician),
and (iii) clinically and radiologically diagnosed pneumonia (when
both criteria were present). Children whose final diagnosis was
tuberculous pneumonia or chemical pneumonitis following kerosene
ingestion were excluded. Those in whom the data were incomplete
(discharged against medical advice, absconded) were also excluded.
A pre-designed proforma was used to record the
demographic profile (age and sex), symptoms (fever, cough, difficulty in
breathing, altered sensorium, convulsions, inability to feed and
wheezing), physical findings (weight, temperature, level of
consciousness, cyanosis, shock, respiratory rate, chest retraction,
grunting, auscultatory signs such as crackles and wheeze, associated
congenital heart disease), radiologic findings(chest radiograph findings
were available for all cases), oxygen saturation, need for assisted
ventilation and final outcome. The possible outcomes were
"Discharged"(those children who recovered) as per the treating physician
or "Death". Risk factors for mortality analyzed were young age of 1-6
months, female sex, presence of wheeze, respiratory rate
≥70/min, chest
retraction (lower chest indrawing), altered level of consciousness
(ALOC) as denoted by unresponsiveness to voice or pain, convulsion at
the time of presentation, shock as defined by Pediatric Advanced Life
Support (PALS) guidelines [13], associated congenital heart disease
(CHD) confirmed by echocardiogram, measles infection within past three
months, weight for age <-2 Z score, and need for assisted ventilation at
the time of presentation. Need for assisted ventilation was based on the
treating clinician’s decision. Nutritional status was recorded by using
the Z score as per WHO standards of weight for age [14]. Risk factors
for all the three study groups of pneumonia were analyzed separately.
Statistical analysis: Data collected from
hospital records were entered in case report forms. These data were
entered in SPSS 11.5 for statistical analysis. After entering the data,
they were checked for accuracy and also checked statistically and
inconsistencies were resolved with the raw data. For the analysis of
pneumonia related mortality, comparison was carried out among the above
described three groups. Cases and controls (discharged) in the
ratio of 1:2 were selected by arranging the discharged cases serially
according to admission among the three groups and every 5 th
discharged child was included as a control. The calculated sample size
was 1320 in each group based on the previous reported least Odds Ratio
of 1.4 for the risk factor of age less than six months, with 80% power
and 95% confidence, assuming 40% of exposure in control group.
Chi square test was used to study the association between the
contributory factors and outcome (mortality). The association was
studied by univariate analysis by Pearson Chi square test initially and
risk was assessed by using Odds Ratio with 95% Confidence Interval [OR
(95% CI)]. Stepwise multiple regression analysis was used to identify
independent factors associated with the outcome. To find out the
association of the various grades of under nutrition, with mortality,
Chi Square test for trend was applied. All hypothesis testing was two
tailed and P value of £0.05
was considered statistically significant.
Results
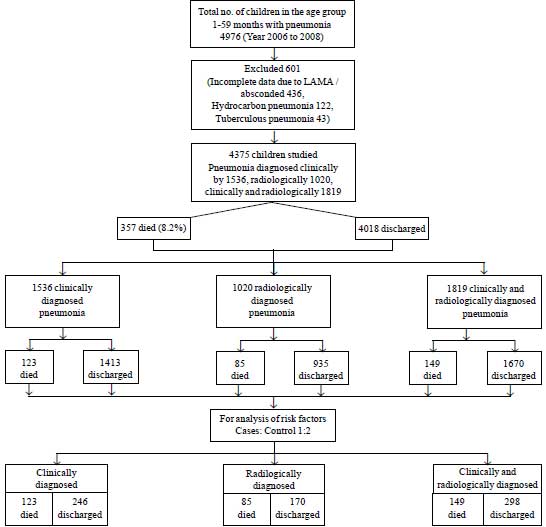
In the period between January 2006 and December 2008,
there were 4976 children admitted in the age group of 1month to 59
months with a final diagnosis of pneumonia. 4375 children (42% girls)
were included in the study after excluding those with chemical
pneumonitis or tuberculous pneumonia and those in whom the data were
incomplete There were 1536 children who were diagnosed to have pneumonia
based on clinical features alone, 1020 children who were diagnosed by
radiological findings alone and 1819 children who had clinical as well
as radiological evidence of pneumonia (Fig. 1). Total
cases of pneumonia constituted 8% of hospital admissions in this period.
There were 1176, 1670 and 1529 children with pneumonia in the years
2006, 2007 and 2008, respectively.
 |
|
Fig.1 Flow chart of study subjects.
|
Majority of the children (2175; 48%) were in the age
group 1-6 months (Table I). 357 children died providing an
over all case fatality rate of 8.2 % (95% CI: 7.37 - 8.99%). The all
cause mortality in the age group of 1 month to 59 months was 3.9% in
this period as per the hospital statistics.
TABLE I Age and Case Fatality Rate Among Pneumonia Cases
|
Age group |
Clinical |
Radiological |
Clinical and radiological |
Total |
|
death, n (%) |
death, n (%) |
death, n (%) |
death, n (%) |
|
1-6 m |
83/735 (11.3) |
49/404 (12.1) |
96/1036 (9.3) |
228/2175 (10.5) |
|
7-<12 m |
13/244 (5.3) |
16/219 (7.3) |
20/335 (6.0) |
49/798 (6.1) |
|
12-<24 m |
14/324 (4.3) |
9/201 (4.5) |
11/270 (4.1) |
34/795 (4.3) |
|
24-59 m |
13/233 (5.6) |
11/196 (5.6) |
22/178 (12.4) |
46/607 (7.6) |
|
Total |
123/1536 (8.0) |
85/1020 (8.3) |
149/1819 (8.2) |
357/4375 (8.2) |
The difference in mortality due to pneumonia among
male and female children was not statistically significant (P=0.12).
The mortality rate was lower in older children as compared to younger
ones (P=0.001) (Table I). The difference in CFR
among the three study groups was not significant, except in clinically
and radiologically diagnosed cases in the age group of 24 to 59 months,
which was higher compared to clinically diagnosed and radiologically
diagnosed cases (Table II).
TABLE II Comparison of Case Fatality Among Study Groups
|
Clinically vs radiologically diagnosed
pneumonia
|
Clinically vs clinically and
radiologically diagnosed pneumonia |
Radiologically vs clinically and
radiologically diagnosed pneumonia
|
|
OR (95%CI) |
P value |
OR (95%CI) |
P value |
OR (95%CI) |
P value |
|
1-6 months |
0.92 (0.62-1.37) |
0.67 |
1.25 (0.90-1.72) |
0.16 |
1.35 (0.92-1.98) |
0.10 |
|
7 -<12 months |
0.71 (0.31-1.61) |
0.38 |
0.89 (0.41-1.91) |
0.74 |
1.24 (0.60-2.57) |
0.53 |
|
12 - <24 months |
0.96 (0.38-2.46) |
0.93 |
1.06 (0.45-2.56) |
0.88 |
1.10 (0.41-2.93) |
0.83 |
|
24 -59 months |
0.99 (0.41-2.44) |
0.99 |
0.42 (0.19-0.90) |
0.01** |
0.42 (0.19-0.95) |
0.02* |
|
Total |
0.96 (0.71-1.29) |
0.77 |
0.98 (0.75-1.26) |
0.84 |
1.02 (0.76-1.36) |
0.89 |
In the case control analysis by univariate analysis
of risk factors contributing to mortality, young age of 1-6 months,
altered level of consciousness, weight for age <-2 Z score,
shock, CHD and need for assisted ventilation were significantly
associated with mortality among the clinically diagnosed pneumonia
cases. Among radiologically diagnosed cases, convulsion was found to be
an additional factor. In clinically and radiologically diagnosed
pneumonia cases, wheeze was found to be more commonly seen among those
who got discharged when compared to those who died. The proportion of
female children and those who had measles in the past, presence of chest
retraction and respiratory rate ³70/min
were similar among ‘discharged’ as well as ‘died’ in all the three study
groups.
On multivariate analysis, need for assisted
ventilation was found to be the only independent risk factor for death
among all the three study groups of pneumonia. In addition young age of
1-6 months, weight for age < - 2Z score, altered level of
consciousness (ALOC) and CHD among clinically diagnosed pneumonia cases;
ALOC and CHD among radiologically diagnosed pneumonia cases; and weight
for age <-2Z score among clinically and radiologically diagnosed
pneumonia cases were found to be significant independent risk factors
for death (Tables III, IV and V).
TABLE III Risk Factors for Mortality Among Clinically Diagnosed Pneumonia Cases
|
Risk factors |
Status |
Unadjusted OR
|
P value |
OR (95%CI)# |
P value |
|
Discharged
(n=246) No (%) |
Death
(n=123) No (%) |
(95%CI)*
|
|
|
|
|
Age (1-6 months) |
120 (48) |
83 (67.5) |
2.18 (1.35-3.52) |
0.001 |
1.15 (1.06-1.24) |
0.001 |
|
Female sex |
94(38.2) |
53 (43.1) |
1.22 (0.77-1.95) |
0.37 |
|
|
|
Wheeze |
18(7.3) |
4 (3.2) |
0.43 (0.12-1.38) |
0.12 |
|
|
|
RR (³70 per min) |
164(66.7) |
81 (65.9) |
0.96 (0.60-1.56) |
0.87 |
|
|
|
Chest retraction |
111(45.1) |
43 (35.00) |
0.65 (0.41-1.05) |
0.06 |
|
|
|
Altered consciousness |
8(3.2) |
18 (14.6) |
5.10 (2.02-13.25) |
0.001 |
1.56(1.20-2.04) |
0.001 |
|
Convulsions |
9(3.7) |
10 (8.1) |
2.33 (0.85-6.44) |
0.06 |
|
|
|
Weight for age<-2Z score |
112 (45.5) |
76 (61.8) |
1.80 (1.12-2.91) |
0.01 |
1.12(1.03-1.21) |
0.007 |
|
Need for assisted ventilation
|
4 (1.6) |
61 (49.6) |
59.52 (19.78-200.65) |
0.001 |
1.97(1.77-2.19) |
0.001 |
|
Measles |
3 (1.2) |
1 (0.8) |
1.69 (0.80-3.57) |
0.13 |
|
|
|
Shock |
15 (6.1) |
16 (13.0) |
2.30 (1.04 -5.13) |
0.01 |
|
|
|
CHD |
7 (2.8) |
9 (7.3) |
2.70 (1.01-8.27) |
0.05 |
1.39(1.02-1.92) |
0.04 |
|
*Univariate #Multivariate; RR:
Respiratory rate, CHD: Congenital heart disease. |
TABLE IV Risk Factors for Mortality Among Radiologically Diagnosed Pneumonia Cases
|
Risk factors |
Status |
Unadjusted OR |
P value |
OR (95% CI)# |
P value |
|
Discharged
(170) n (%) |
Death
(85) n (%) |
(95%CI)* |
|
|
|
|
Age (1-6 months) |
56 (32.9) |
49 (57.7) |
2.77 (1.57-4.91) |
0.001 |
|
|
|
Female sex |
82 (48.2) |
43 (50.6) |
1.10 (0.63-1.91) |
0.72 |
|
|
|
Wheeze |
6 (3.5) |
2 (2.4) |
0.67 (0.09-3.76) |
0.62 |
|
|
|
Altered consciousness |
4 (2.4) |
22 (25.9) |
14.49 (4.49-51.88) |
0.001 |
1.56 (1.24-1.87) |
0.001 |
|
Convulsions |
4 (2.4) |
22 (25.9) |
11.15 (3.38-40.59) |
0.001 |
|
|
|
Weight for age<-2Z score |
76 (44.7) |
49 (57.6) |
1.85 (1.03-3.32) |
0.02 |
|
|
|
Need for assisted ventilation
|
9 (5.3) |
58 (68.2) |
115.89 (38.43-94.71) |
0.001 |
1.96 (1.78-2.17) |
0.001 |
|
Measles |
4 (2.4) |
0 |
– |
0.15 |
|
|
|
Shock |
15 (8.8) |
4 (4.7) |
0.51 (0.14 -1.72) |
0.23 |
|
|
|
CHD |
4 (2.4) |
10 (11.8) |
5.53 (1.53-21.72) |
0.001 |
1.39 (1.07-1.82) |
0.016 |
|
*Univariate #Multivariate; RR:
Respiratory rate, CR: Chest retraction; CHD: Congenital heart
disease. |
TABLE V Risk Factors for Mortality Among Clinically and Radiologically Diagnosed Pneumonia Cases
|
Risk factors |
Status |
Unadjusted OR |
P value |
OR (95% CI)# |
P value |
|
Discharged |
Death |
(95%CI)* |
|
|
|
|
(298) n (%) |
(149) n (%) |
|
|
|
|
|
Age(1-6 months) |
161 (54.0) |
96 (64.4) |
1.54 (1.01-2.36) |
0.04 |
|
|
|
Female sex |
132 (44.3) |
68 (45.6) |
1.06 (0.70-1.60) |
0.78 |
|
|
|
Wheeze |
22 (7.4) |
3 (2) |
0.26 (0.06-0.93) |
0.02 |
|
|
|
RR(³70 per min) |
298 (100.0) |
149 (100) |
– |
1.00 |
|
|
|
Chest retraction |
150 (50.3) |
84 (56.4) |
1.28 (0.84-1.93) |
0.22 |
|
|
|
Altered consciousness |
9 (3.0) |
19 (12.8) |
4.69 (1.95-11.55) |
0.001 |
|
|
|
Convulsions |
9 (3.0) |
10 (6.7) |
2.31 (0.84-6.35) |
0.06 |
|
|
|
Weight for age<-2Z score |
128 (43) |
85 (57) |
2.00 (1.29-3.11) |
0.001 |
1.13(1.05-1.21) |
0.001 |
|
Need for assisted ventilation |
7 (2.4) |
70 (47) |
36.84 (15.56-91.23) |
0.001 |
2.01(1.82-2.22) |
0.001 |
|
Measles |
1 (0.3) |
0 |
– |
0.39 |
|
|
|
Shock |
28 (9.4) |
11 (7.4) |
0.77 (0.35 -1.67) |
0.47 |
|
|
|
CHD |
9 (3.0) |
15 (10.1) |
3.59 (1.44-9.15) |
0.001 |
|
|
|
*Univariate; #Multivariate;
RR: Respiratory rate, CHD: Congenital heart disease. |
There was a trend of increase in death rate with
worsening nutritional status (Table VI). Poor nutritional
status was strikingly associated with mortality in children younger than
24 months of age, as mortality was seen only in children with - Z
score in this age group.
TABLE VI Nutritional Status and Outcome in Pneumonia
|
Weight for age Z score |
Case fatality |
OR (95%) (I) |
|
<–3.0 |
127/908 (14%) |
2.25 (1.66-3.04) |
|
<–3 to –2.0 |
83/1120 (7.4%) |
1.1 (0.8-1.54) |
|
<–2 to –1.0 |
81/1200 (6.7%) |
1.0 |
|
<-1 to 0 |
33/586 (5.6%) |
0.82 (0.53-1.27) |
|
0-1 |
9/246 (3.7%) |
0.52 (0.24-1.1) |
|
1-2 |
2/59 (3.4%) |
0.48 (0.0-2.07) |
|
2-3 |
1/40 (2.5%) |
0.35 (0.02-2.44) |
|
P=0.001 per trend; #Odds ratio with 95%
confidence interval; *significant at P
≤0.05. |
Discussion
Averting pneumonia deaths will significantly
contribute to realizing Millennium Development Goal 4 (MDG4) of reducing
under five mortality [13]. This retrospective analysis was conducted to
identify the demographic and clinical variables associated with deaths
in hospitalized children of 1 month –59 months of age with a diagnosis
of pneumonia. The case fatality rate (CFR) of pneumonia was 8.2%
compared to 3.9% for all cause mortality in this age group in the same
period. CFR of childhood pneumonia in various Indian studies ranges
between 8.9% to 47% [4,5,9,10,15,16,] and 3.4% to 12% in other
developing countries [6,7,17].
The risk factors for deaths due to pneumonia vary
between countries, regions and communities. Frequently studied factors
are young age, low birth weight, under nutrition, anemia, lack of
parental education, over-crowding, indoor air pollution, lack of
exclusive breast feeding, lack of measles immunization, co-morbidities
such as congenital heart diseases and other congenital anomalies and
severity at presentation to hospital [4-9,11]. In this study, need for
assisted ventilation was found to be independently associated with fatal
pneumonia of clinically, radiologically, as well as clinically and
radiologically diagnosed pneumonia cases. Need for assisted ventilation
at the time of presentation is likely to indicate the severity. In
another study, cyanosis and head nodding were the determining factors
for mechanical ventilation [4]. Other factors like young age of 1- 6
months, weight for age <-2 Z score, altered level of
consciousness and CHD were found to be associated with mortality in
pneumonia, even though these factors were not observed in all the three
study groups. The different combination of risk factors among these
groups may be due to ambiguity in clinical features for pneumonia,
associated wheeze, CHD, etc. Young age has been reported to be a risk
factor for mortality in studies from India and other developing
countries [7-9, 11]. Malnutrition was another significant contributory
factor for mortality in other studies also [9,11, 17]. Not only that
malnutrition was associated with increased fatality, there was an
incremental effect in pneumonia mortality with increasing degree of
malnutrition when all the cases were considered together. CHD was a risk
factor for pneumonia mortality in a study [7] while not so in another
study [4].A more detailed analysis with reference to the type(cyanotic
or acyanotic) and severity of CHD is needed to clarify its role in
pneumonia deaths.
Limitations of the study are that specific etiology
of pneumonia could not be identified by blood culture or other methods
and radiological diagnosis was by the radiologist and clinician by
consensus and not as per WHO criteria [18]. Other potentially relevant
risk factors such as lack of exclusive breast feeding, indoor air
pollution, hypoxia, increased C-reactive protein and head nodding were
not studied due to non availability of these data in view of
retrospective nature of the study. The sample studied also was less than
calculated sample size. A strength of the study was the study period of
three years preventing the effect of epidemic outbreak and seasonality.
Case fatality rate among children 1 month to 59
months of age hospitalized with community acquired pneumonia was 8.2%.
Need for assisted ventilation was found to be independently associated
with mortality in children aged 1-59 months admitted with pneumonia.
Young age (1- 6 months), malnutrition (<-2 Z weight for age),
altered level of consciousness and associated congenital heart disease
are other factors and hence more aggressive monitoring and management
are required in children with these risk factors.
Contributors: PR: Conceived,
designed the study and collected the data. PR and KN: Drafted the
article. KN: Revised it critically for important intellectual content.
AV: managed data, analyzed and interpreted the results. SS:
Co-ordinated and guided the research.
Funding: Nil; Competing interests: None
stated.
|
What is Already Known?
•
Identified risk factors for mortality with pneumonia are young
age, low birth weight, under nutrition, anemia, illiteracy of
parents, over crowding, indoor air pollution, lack of exclusive
breast feeding, lack of measles immunization, congenital heart
diseases, congenital anomalies, severity at presentation and
altered level of consciousness.
What This Study Adds?
•
The case fatality rate due to
pneumonia among hospitalized children aged 1 month to 59 months
during the period 2006 to 2008 was 8.2%.
• An additional risk
factor independently associated with mortality in cases of
childhood pneumonia is need for assisted ventilation.
|
References
1. Williams BG,Gouws E, Boschi-Pinto C, Bryee J, Dye
C. Estimates of world wide distribution of child deaths from acute
respiratory infections. Lancet Infect Dis. 2002;2:25-32.
2. World Health Statistics Geneva WHO; 2007 available
from http://www.who.int/whosis/whostat 2007.pdf
3. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I,
Bassani DG, et al. For the Child Health Epidemiology Reference
Group of WHO and UNICEF. Global, Regional, and National causes of child
mortality in 2008: a systematic analysis. Lancet. 2010; 375:1967-87.
4. Tiewsoh K, Lodha R, Pandey RM, Broor S, Kalaivani
M, Kabra SK. Factors determining the outcome of children hospitalized
with severe pneumonia. BMC Pediatrics. 2009;9:15.
5. Agrawal PB, Shendurnikar N, Shastri NJ. Host
factors and pneumonia in hospitalized children. J Indian Med Assoc.
1995;93:271-2.
6. Suwanjutha S, Ruandkanchanasetr S,
Chantarojanasini T, Ttotrakitya S. Risk factors associated with
morbidity and mortality of pneumonia in children under 5 years.
Southeast Asian J Trop Med Public Health. 1994;25:60-6.
7. Djelantik IG, Gessner BD, Sutanto A, Steinhoff M,
Linehan M, Moulton LH, et al. Case fatality proportions and
predictive factors for mortality among children hospitalized with severe
pneumonia in a rural developing country setting. J Trop Pediatr.
2003;49:327-32.
8. Rudan I, Boschi-Pinto C, Biloglav Z,
Mulholland K, Campbell H. Epidermiology and etiology of childhood
pneumonia. Bull World Health Organ. 2008;86:408-16.
9. Sehgal V, Sethi GR, Sachdev HP, Satyanarayana
L. Predictors of mortality in subjects hospitalized with acute lower
respiratory tract infections. Indian Pediatr. 1997;34:213-9.
10. Patwari AK, Aneja S, Mandal RN, Mullick DN.
Acute respiratory infections in children: a hospital based report.
Indian Pediatr. 1988;25:613-7.
11. Deivanayagam N, Nedunchelian K, Ramasamy S,
Ratnam SR. Risk factors for fatal pneumonia: a case control study.
Indian Pediatr. 1992;29:1529-32.
12. World Health Organization. Handbook IMCI.
Integrated management of childhood illness. Geneva: World Health
Organization 2000.
13. Ralston M, Hazinski MF, Zaritsky AL,
Schexnayder SM, Kleinman ME. PALS Provider Manual. American Heart
Association, Dallas, Texas. 2006. p.66-68.
14. WHO Multicentre Growth Reference Study
Group.WHO Child Growth Standards:length/height-for-age,weight-for-age-weight-for-length,weight-for-height
and body mass index-for-age:methods and development.Geneva: World
Health Organization,2006.
15. Berman S, McIntosh K. Acute Respiratory
infection. In. Walsh JA, Warren KS (eds). Strategies for
primary health care. Technologies Appropriate for the control of
disease in the developing world. The University of Chicago press,
1986. p.29-46.
16. Roy P, Sen PK, Das KB, Chakraborty AK. Acute
respiratory infections in children admitted in a hospital of
Calcutta. Indian J Public Health. 1991;35:67-70.
17. Banajeh SM. Outcome for children under 5
years hospitalized with severe Acute Lower Respiratory Infections in
Yemen. A 5 year Experience. J Trop Pediatr. 1998;44:343-6.
18. World Health Organization Pneumonia Vaccine Trial Investigators
Group. Standardization of interpretation of chest radiographs for the
diagnosis of pneumonia in children. Geneva, WHO; 2001
|
|
|
 |
|

