|
|
|
Indian Pediatr 2011;48: 897-899 |
 |
ASHA’s Involvement in Newborn Care: A
Feasibility Study |
|
P Stalin, Anand Krishnan, Sanjay K Rai and *Ramesh K
Agarwal
From the Centre for Community Medicine; and *Division of
Neonatology, Department of Pediatrics;
All India Institute of Medical Sciences, New Delhi, India.
Correspondence to: Dr Anand Krishnan, Additional
Professor, Centre for Community Medicine,
All India Institute of Medical Sciences, New Delhi 110 029, India.
Email: [email protected]
Received: August 19, 2010;
Initial review: November 29, 2010;
Accepted: February 01, 2011.
Published online:
2011 May 30.
PII:S09747559INPE1000446-2
|
|
Abstract
Quality of life was assessed in 108 epileptic
children (6-15 years) using a hindi translation of Quality of Life in
Children with Epilepsy (QOLCE) questionnaire. The questionnaire consist
of 76 items with 16 subscales covering five domains of life: physical
function, social function, cognition, emotional and behavioral well
being. Overall score was 62.62±21.32. Chronbach’s-a
for all 13 multi-item subscales was above 0.70, indicating good internal
consistency and reliability. Pearson correlation revealed good construct
validity. Overall quality of life was affected by age, type of epilepsy,
seizure frequency and maternal education (P<0.05). Energy levels,
language and attention (P<0.05) were better in older children
whereas younger children had better self esteem and lower levels of
anxiety. Seizure frequency compromised all fields except stigma,
attention, and energy levels (P>0.05).
Key words: Children, Epilepsy, Hindi, India, Quality of
Life.
|
|
E
very year in India over one
million newborns die before they complete their first month of life,
accounting for 30% of the world’s neonatal deaths [1]. Prematurity, sepsis
and birth asphyxia contribute to 85% of neonatal mortality [2]. In India,
only 40.7% deliveries were institutional and only 36.3% mothers received
postnatal care within 2 days of delivery [3]. Till the above programmatic
bottlenecks are removed, it would be difficult to prevent neonatal deaths.
One of the ways to address these issues under National Rural Health
Mission (NRHM) could be by utilizing Accredited Social Health Activists (ASHAs)
for providing newborn care. They are already being used to promote
institutional delivery under Janani Suraksha Yojana (JSY). Under the
guidelines of NRHM, it is mentioned that states could explore the
possibility of involvement of ASHAs in providing care for newborn through
graded training [4]. This study was done as a pilot study to assess the
feasibility of involvement of ASHAs in newborn care after training.
Methods
The study area was Primary Health Center (PHC) Dayalpur
which is under the Comprehensive Rural Health Services Project (CRHSP) of
Centre for Community Medicine (CCM), All India Institute of Medical
Sciences (AIIMS) located in the Ballabgarh block in Faridabad district of
Haryana.
The study design was Interventional (pre and post
training comparison) and conducted from December 2008 to June 2009.
Informed oral consent was taken from all ASHAs. All the ASHAs (n =
33) of Primary Health Centre Dayalpur were trained in providing newborn
care by community physicians at Civil Hospital, Ballabgarh. This was
followed by two refresher training at three months interval and supportive
supervision. Twenty eight ASHAs had studied upto eighth standard, four
were 10th standard pass and only one was 12th standard pass. They had
undergone two rounds of induction training for five days each under the
routine program.
The components included under newborn care were
weighing of the newborn, identification and referral of low birth weight
babies and sick neonates, and counseling of mothers on neonatal issues
like breastfeeding, warmth, cord care etc. The training by medical
officers included both didactic and demonstration session. The training
manual consisted of chapters which corresponded to different components of
neonatal care listed above as well as ante-natal care, intranatal care,
and recording and repor-ting. All the ASHAs were provided a book and a
spring balance weighing scale at the end of the training.
The outcome variables assessed were related to
knowledge assessment, performance assessment and skill assessment. ASHA’s
knowledge related to all the components of newborn care was assessed using
a questionnaire which consisted of 11 multiple choices questions. They
were assessed before training and immediately after the training, after 3
months and after 6 months. The mean knowledge score was calculated.
 |
|
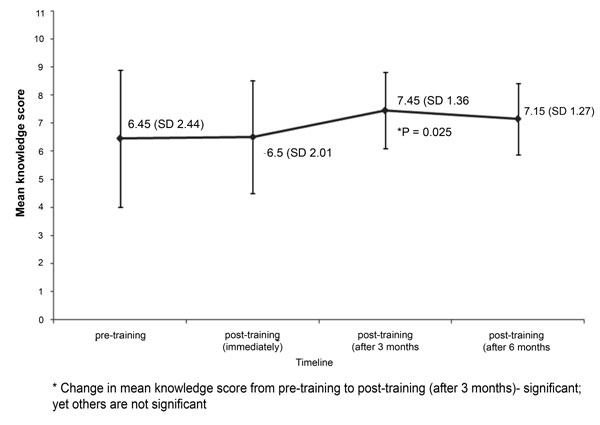
Fig.1 Mean knowledge scores of twenty
ASHAs who attended all assessments before and after training. |
ASHA’s performance was assessed for 6 months. The
performance indicators were related to different activities they were
expected to perform and are listed in Table I. Monthly
reports were submitted by ASHA through health workers, who cross-checked
the reports.
TABLE I Performance of ASHAs for Neonatal Care in 6 Months Period After Training
| Indicators |
Frequency |
| Mother counseled |
|
| Breast feeding |
330 |
| Weaning |
339 |
| Hospital delivery (n=219) |
|
| Escorted |
124 |
| Home delivery (n=112) |
|
| Newborn weighed on 1st d |
54 |
| Newborn weighed 2nd – 3rd d |
39 |
| Performance |
|
| Sick Neonates |
|
| Identified |
22 |
| Referred |
16 |
| Escorted |
3 |
| Follow up after 2 days |
14 |
| Birth wt <2 kg |
|
| Identified |
10 |
| Referred |
6 |
| Escorted |
2 |
| Follow up after 2 d |
6 |
ASHAs’ skill of weighing the neonates was assessed
using a checklist with 8 items. The precision of each ASHA’s measurement
of neonate weight was compared to that of the author (SP) using the same
weighing scale.
All the data were entered in MS Excel 2007 and analysis
done using Stata 9. Repeated measures ANOVA test was used to detect any
significant change in mean knowledge score from baseline and was
considered significant at P<0.05.
Results
Out of 33 ASHAs, thirty one attended the training, and
30 attended the pre-training assessment. Post training assessment
immediately after training was attended by 29 ASHAs. At the end of 3 and 6
months, 24 and 25 ASHAs attended the assessment, respectively. At the end
of 6 months, 25 ASHA’s skill of weighing the neonates was assessed (Fig.1).
Ony 20 ASHAs attended all the assessments. Out of 219 hospital deliveries,
124 (56.6%) were escorted by ASHAs. Out of 112 newborns born at home
during the six months period, 93 (83%) were weighed within 3 days of birth
(Table I). ASHAs identified and referred six low birth
weight babies and 16 sick neonates over a period of six months.
All the 8 steps of measuring the infant’s weight were
done correctly by almost all ASHAs except for the fourth step which was a
critical step of ensuring no zero error (Table II). Eleven
ASHAs weighed the newborns within ± 250 grams of the weight recorded by
the author.
TABLE II Performance of ASHAs in Correctly Following Eight Steps Of Weighing the Newborn
During Six Months After Training
| Steps |
n (%) |
| Remove the extra clothes |
15 (60) |
| Spread the baby carrier in a surface |
25 (100) |
| Make the baby lie down on the baby carrier |
25 (100) |
| Ensure the pointer is in zero
position, if not then do it |
4 (16) |
| Height of the machine should be at
the level of observer’s eyes |
24 (96) |
| Fix the baby carrier with the baby
to the hook of the weighing machine |
25 (100) |
| While reading the weight, nobody
should touch the baby |
23 (92) |
| When the baby is quiet and the
pointer is stable, note the weight |
25 (100) |
Discussion
Our study showed that the knowledge did not increase
immediately after training. This could be because pre-training knowledge
of ASHAs was high. This could be attributed to the induction trainings
under routine program and working experience for more than 2 years. In
addition, this could be due to shorter duration of training. Three months
after training, there was significant increase in the knowledge of ASHAs.
This could be attributed to learning by doing and indicates the need for
practical training for ASHAs.
We did not attempt to validate the performance of the
ASHAs. The validity of identification of sick neonates by community health
worker was demons-trated in Bangladesh and showed a sensitivity of 73% and
a specificity of 98%, against physician diagnosis [5]. In contrast to our
study, they received training for 36 days, which is not replicable as per
NRHM guidelines.
The limitations of the study were not validating the
ASHA’s performance and lack of denominators on low birth weight babies and
sick neonates. So we could not measure the efficacy of ASHA’s performance.
However, in our study, the proportion of birth weight < 2000 g was 10.7%.
The denominator was only 93 home delivered newborns weighed by ASHAs. This
is comparable with 22% of low birth weight babies (<2500 g) where only 34%
of newborns were weighed [6]. No incentives were provided to ASHAs during
this exercise and it is to be expected that the performance will improve
if these are linked to explicit incentives as is being done for their
other activities. In conclusion, ASHAs could be involved in providing care
for newborn. However such efforts should ensure a stronger focus on skill
development and practical experience. This also calls for a stronger
monitoring and supervision of their activities by the health system.
Contributors: All authors contributed to the study
design, data collection, analysis and drafting the manuscript.
Funding: AIIMS, New Delhi. Competing interests:
None stated.
|
What This Study Adds?
• ASHAs could be involved in providing some components of
neonatal care like taking birth weight and advising about neonatal
health at the domiciliary level.
|
References
1. USAID. Maternal and Child Health – 2004. USAID
Battles Neonatal Deaths in India. (Online) 2005: Available from: http://www.usaid.gov/our_work/global_health/home/News/ghachievements.html.
Accessed March 23, 2010.
2. Bang AT, Paul VK, Reddy HM, Baitule SB. Why do
neonates die in rural Gadchiroli, India? (Part I): primary causes of death
assigned by neonatologist based on prospectively observed records. J
Perinatol. 2005;25:s29-s34.
3. International Institute for Population Sciences (IIPS)
and Macro International. 2007. National Family Health Survey (NFHS-3),
2005–06: India. Mumbai: IIPS. Available from: http://www.nfhsindia.org/pdf/IN.pdf.
Accessed April 28, 2010.
4. Ministry of Health and Family Welfare. Government of
India. National Rural Health Mission. Guidelines on Accredited Social
Health Activist. Available from: http://www.mohfw.nic.in/NRHM/RCH/guidelines/ASHA_guidelines.pdf.
Accessed April 12, 2010.
5. Darmstadt GL, Baqui AH, Choi Y, Bari S, Rahman SM,
Mannan I, et al. Validation of community health workers’ assessment
of neonatal illness in rural Bangladesh. Bull World Health Organ.
2009;87:12-9.
6. International Institute for Population Sciences (IIPS)
and Macro International. 2007. National Family Health Survey (NFHS-3),
2005–06: India. Mumbai: IIPS. Available from: http://www.nfhsindia.org/NFHS-3Data/VOL-1/Summary
of Findings.pdf. Accessed on January 4, 2011.
|
|
|
 |
|

