|
|
|
Indian Pediatr 2010;47: 911-920 |
 |
Objective Structured Clinical Examination (OSCE)
Revisited |
|
Piyush Gupta, Pooja Dewan and
Tejinder Singh*
From the Department of Pediatrics, University College of
Medical Sciences, Delhi, and *Department of Pediatrics,
Christian Medical College, Ludhiana, India.
Correspondence to: Dr Piyush Gupta, Block R 6 A, Dilshad
Garden, Delhi 110 095.
Email: [email protected]
|
Objective structured clinical examination (OSCE) was introduced in
1975 as a standardized tool for objectively assessing clinical
competencies - including history-taking, physical examination,
communication skills, data interpretation etc. It consists of a circuit
of stations connected in series, with each station devoted to assessment
of a particular competency using pre-determined guidelines or
checklists. OSCE has been used as a tool for both formative and
summative evaluation of medical graduate and postgraduate students
across the globe. The use of OSCE for formative assessment has great
potential as the learners can gain insights into the elements making up
clinical competencies as well as feedback on personal strengths and
weaknesses. However, the success of OSCE is dependent on adequacy of
resources, including the number of stations, construction of stations,
method of scoring (checklists and/or global scoring), the number of
students assessed, and adequate time and money. Lately, OSCE has drawn
some criticism for its lack of validity, feasibility, practicality, and
objectivity. There is evidence to show that many OSCEs may be too short
to achieve reliable results. There are also currently no clear cut
standards set for passing an OSCE. It is perceived that OSCEs test the
student’s knowledge and skills in a compartmentalized fashion, rather
than looking at the patient as a whole. This article focuses on the
issues of validity, objectivity, reliability, and standard setting of
OSCE. Presently, the Indian experiences with OSCE are limited and there
is a need to sensitise the Indian faculty and students. A cautious
approach is desired before it is considered as a supplementary tool to
other methods of assessment for the summative examinations in Indian
settings.
Key words: Assessment, Clinical, Competency, India, OSCE,
Reliability, Validity.
|
|
That ‘learning is driven by assessment’
is a well known fact. This is also referred to as the ‘steering effect
of examinations’. To foster actual learning, assessment should be
educative and formative. Medical education aims at the production of
competent doctors with sound clinical skills. Competency encompasses six
inter-related domains as developed by Accreditation Council for Graduate
Medical Education (ACGME): knowledge, patient care, professionalism,
communication and interpersonal skills, practice based learning and
improvement, and systems based practice(1). Epstein and Hundert have
defined competence of a physician as "the habitual and judicious use of
communication, knowledge, technical skills, clinical reasoning, emotions,
values and reflection in daily practice for the benefit of the individuals
and the community being served"(2). The community needs to be protected
from incompetent physicians; and thus there is a need for summative
component in the assessment of medical graduates.
Looking Beyond the Traditional Tools
The traditional tools for assessment of medical
students have mainly consisted of written exams (essay type, multiple
choice, and short-answer type questions), bedside viva and clinical case
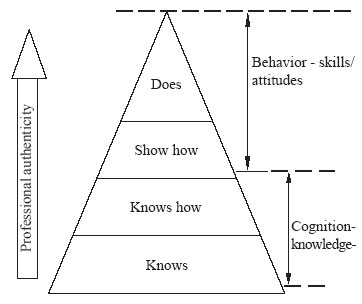
presentation. These have focussed on the "knows" and "knows how"
aspects, i.e., the focus has been on the base of the ‘Miller’s pyramid
of competence’ (Fig.1). These methods of assessment
however have drawn a lot of criticism over the years because of their
inability to evaluate the top levels of the pyramid of competency in a
valid and reliable manner. The following flaws were realised:
• They test only the factual knowledge and
problem-solving skills of students, which may be appropriate only in the
early stages of medical curriculum. These methods do not evaluate the
clinical competence of students. Important aspects like performing a
particular physical examination (shows how), clinical maneuver, and
communication-skills are not tested. Only the end result is tested and
not the process of arriving at a result.
• The students are tested on different patients
(patient variability). Each student is adjudged by only one or two
examiners, thereby a scope for marked variation in the marking by
different examiners (examiner variability). These factors increase the
subjectivity of marking (lack of reliability).
• There is often a lack of clarity on what is
actually being tested (lack of validity). Assessment is usually global
and not competency based.
• Students are not examined systematically on core
procedures.
• There is no systematic feedback from the students
and teachers.
To obviate the drawbacks of conventional clinical
evaluation, objective structured clinical examination (OSCE) was first
introduced by Harden in 1975, as a more objective, valid, and reliable
tool of assessment(3). In an ideal OSCE, all domains of competencies are
tested, specially the process part; the examination is organized to
examine all students on identical content by the same examiners using
predetermined guidelines; and a systematic feedback is obtained from both
students and the teachers. OSCE is meant to test the ‘shows how’
level of the Miller’s pyramid(4).
|
What Is An OSCE?
Objective
• Structured• Clinical• Examination
1. Ensures evaluation of set of predetermined
clinical competencies.
2. Each clinical competency is broken down into
smaller components; e.g., taking history, performing examination,
interpreting investigations, communicating, etc.
3. Each component is assessed in turn and marks are allotted
according to predetermined checklists.
|
 |
|
Fig.1 Miller’s pyramid.
|
Content and Process of OSCE
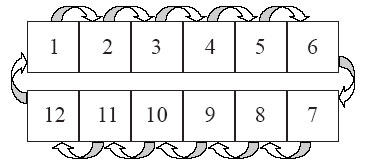
OSCE consists of a circuit of stations which are
usually connected in series (Fig. 2). Each station is
devoted to evaluation of one particular competency. The student is asked
to perform a particular task at each station. These stations assess
practical, communication, technical, and data interpretation skills and
there is a predetermined decision on the competencies to be tested.
Students rotate around the complete circuit of stations, and keep on
performing the tasks at each of the stations. All students move from one
station to another in the same sequence. The performance of a student is
evaluated independently on each station, using a standardized checklist.
Thus, all students are presented with the same test; and are
assessed by the same or equivalent examiners. Students are marked
objectively on the checklist(5) by the examiner.
 |
|
Fig.2 OSCE consists of a circuit of
stations which are usually connected in series. |
Types of OSCE stations: The stations are
categorized as ‘procedure station’ or ‘question station’.
Procedure stations are observed by the examiner while question stations
are unobserved (only a written answer is desired). Student performance on
a Procedure station is observed and marked there and then only while the
Question stations can be evaluated later. The details of these stations
along with specific examples have been described previouly(5). Procedure
station and a question station can also be used together. In the original
description of OSCE by Harden, every Procedure station was followed by a
Question station. Students are given a task to perform in Station 1 (which
is observed and assesses the process of performing the task) and the
questions are presented later (in Station 2). Questions in station 2 are
related to station 1 only. This has two advantages: (a) different
domains of learning can be assessed by them; and (b) the effect of
cueing is minimized. It is also advisable to incorporate a rest station
for every 30-40 minutes into the exam, to give a break to the students,
the observers and the patients. They also allow time to substitute
patients at a clinical station, or to complete the written left over task
from the previous stations.
OSCE setup: The number of stations can vary
from 12 to 30 though usually 20 stations suffice(1). The usual time
allotted is 5 minutes for each station; ACGME however recommends station
duration of 10-15 minutes. Giving more time per station allows more
competencies to be tested in relation to the given task. All students
begin simultaneously. The number of students appearing in the exam should
not exceed the number of stations. In case, the number of students is
more, one or more parallel sessions can be organized, subject to
availability of space, examiners and patients. If facilities do not permit
this, then two sessions can be planned. All students should commence the
examination from a procedure station. The entire exam is usually completed
within 60-150 minutes. Details of microplanning of OSCE have been
described earlier(6).
Blueprinting: Preparing the Stations
Once the consensus is reached on the number and type of
stations to be included, the next task is to formulate the questions,
model keys, and checklists for each station. When planning an OSCE, the
learning objectives of the course and the students’ level of learning need
to be kept in mind. The test content need to be carefully planned against
the learning objectives - this is referred to as "blueprinting"(7).
Blueprinting ensures a representative sample of what the student is
expected to have achieved. Blueprinting in practice consists of preparing
a two-dimensional matrix: one axis represents the competencies to be
tested (for example: history taking, clinical examination, counseling,
procedure) and the second axis represents the system or problems on which
these competencies are to be shown (for example: cardiovascular system,
nutritional assessment, managing cardiac arrest, etc.)(8).
Blueprinting is essential for building a higher
construct validity of OSCE by defining the problems which the student
will encounter and the tasks within the problem which he is expected to
perform. By laying down the competencies to be tested in a grid, the
correct balance between different domains of skill to be tested can be
obtained (Fig. 2).
Clinical competencies (including psychomotor skills and
certain affective domains) should be primarily identified and included in
the OSCE setup. OSCE can test a wide range of skills ranging from data
gathering to problem solving(4). Although it can be used for this purpose,
OSCE is not very suited for evaluating the cognitive domain of learning,
and certain other behaviors like work ethics, professional conduct, and
team-work skills. For these objectives, it is appropriate to use other
modes of assessment. Feasibility of the task is equally important. Real
patients are more suited to assessing the learner’s examination skills
while simulated patients are more suited to evaluate the communication
skills of the learner.
Occassionally, faculty members designing OSCEs run out
of ideas and end up preparing OSCEs assessing only the recall and by
repeating an earlier OSCE station. The key to ensure that students’
learning is not restricted to 5 or 6 stations commonly used in a subject,
is to have a good blueprint of competencies to be tested and the stations
should be rotated in different examinations.
| |
History |
Examination |
Procedure/data interpretation |
| CVS |
Chest pain |
Cardiovascular system |
ECG interpretation; BP |
| Chest |
Fast breathing and cough |
Respiratory system |
Chest physiotherapy/ Peak flow |
| Abdomen |
Abdominal distension |
Abdomen examination |
Ascitic tap |
| CNS |
Headache |
Nervous system/ Eyes |
Fundoscopy |
| Cardiac arrest |
|
|
CPR |
Fig.3 Grid showing the OSCE blueprint to
assess final year medical students.
Setting the Standard
A major impediment in the success of OSCE remains ‘setting
the pass mark’. The standards for passing OSCE can be either
relative (based on norm-referencing) or absolute (based on
criterion-referencing). Both have their own utility as well as merits and
demerits.
Norm-referencing
‘Angoff approach’ and ‘borderline approach’
are commonly used to set relative standards for OSCE. In the former,
expert judges determine pass marks based on their estimates of the
probability that a borderline examinee will succeed on each item in a
test(9). A major drawback of this method is that the overall performance
of a candidate is not judged. Also the estimates are based keeping a
hypothetical candidate in mind and therefore may be incorrect. This way,
different pass marks will be set across different medical
institutions(10). In addition, this is a time-consuming process and
requires greater commitment from the examiners. A minimum of 10 judges are
required to obtain reliable results (11).
The borderline approach (formulated by Medical Council
of Canada)(12) is a simpler and more commonly accepted method for setting
the pass marks. In this method, the expert judges score examinees at each
station according to a standardized checklist and then give a global
rating of each student’s overall performance. The student can be rated
as pass, borderline, fail, or above expected standard. The mean scores of
examinees rated as borderline becomes the pass mark for the station and
the sum of the means becomes the overall pass mark(13). To increase the
reliability of this method all the expert judges should be subject experts
and several examiners should examine at each station. The Otago study(14)
showed that 6 examiners per station and 180 examinees are needed to
produce valid and reliable pass marks. This method has gained wider
acceptance because the pass marks set are actually an average of
differences in opinion of examiners unlike the ‘Angoff marks’ which
are obtained by arguing out the differences in opinion of the examiners.
Whatever method of standard setting it used, a fine tuning of the
‘experts’ is necessary so that they view the performance of the students
appropriate to his level (e.g. undergraduate or postgraduate) and not from
a specialist perspective.
Wass, et al.(7) state that "Norm-referencing is
clearly unacceptable for clinical competency licensing tests, which aim to
ensure that candidates are safe to practice. A clear standard needs to be
defined, below which a doctor would not be judged fit to practice. Such
standards are set by criterion-referencing."
Criterion-referencing
An absolute clear-cut minimum accepted cut-off is
decided beforehand(15). For example, Medical Council of India (MCI)
recommends 50% as the minimum pass marks for all summative examinations in
medical specialities. National Board of Examination (NBE), India also
accepts overall 50% marks as minimum acceptable for passing in OSCE
examinations. A problem with using the overall pass mark as a benchmark
for competence may not be acceptable as exceptional performance in a few
stations would compensate for poor performance in other stations. It would
be more appropriate to decide upon a minimum total score and a defined
proportion of stations which the examinee must pass in order to pass the
OSCE(13). Certain institutions also make it mandatory to pass the critical
stations. However, it should be kept in mind that OSCE allows students to
score much higher marks as compared to case presentation and adding the
two to decide a pass percentage may be inappropriate. As a good practice,
scores obtained at OSCE should be reported separately from the scores
obtained at case presentations. Correlation between the two sets of scores
is generally poor(16).
Checklists vs Global Rating
Checklists were designed and incorporated into OSCE to
increase the objectivity and reliability of marking by different
examiners. However, scoring against a checklist may not be as effective as
it was thought to be(17). Evidence is accumulating that global rating by
an experienced physician is as reliable as the standardised checklist.
Regehr, et al.(18) compared the psychometric properties of
checklists and global rating scales for assessing competencies on an OSCE
format examination and concluded that "global rating scales scored by
experts showed higher inter-station reliability, better construct
validity, and better concurrent validity than did checklists. Further the
presence of checklists did not improve the reliability or validity of the
global rating scale over that of the global rating alone. These results
suggest that global rating scales administered by experts are a more
appropriate summative measure when assessing candidates on performance
based assessment." Use of global ratings, however, mandates that only
people with subject expertise can be used as examiners. However, there is
still no consensus on the gold standard for the same. A balanced approach
is suggested by Newble(8) wherein checklists may be used for practical and
technical skills stations and global rating scales are employed for
Stations pertaining to diagnosis, communication skills and diagnostic
tasks. Another approach could be to use checklists during early part of
clinical training and global ratings during final summative years.
Example of a global rating scale for assessing
communication skills
|
Task: Counsel this 35 year old woman
who is HIV positive about feeding her newborn baby.
The student is rated on a scale of 1-5. The
examiner score sheet would read as follows:
1.
Exceptional
*
2. Good
*
3.
Average *
4.
Borderline *
5.
Poor/Fail *
|
Note: A checklist can be provided to assist the
examiner in making his judgement of the student’s performance, though no
marks are decided for each item on the checklist. Using a checklist for a
global rating can enhance the validity and reliability of OSCE.
The Concerns
OSCE, now into 35 th
year of its existence, has had its share of bouquets and brickbats.
Despite controversies, it has stood the test of the time and has come to
be recognized as a standard tool of assessment of medical competencies.
OSCE has been used for both formative and summative examination at
graduate and postgraduate level, across the globe.
|
General
VENUE:
Suitable spacious hall with sound proof partitions, or multiple
adjacent rooms, waiting rooms for back up patients, rest rooms,
refreshment area, briefing room
FURNITURE:
Tables, chairs (for patient, examiner and examinee at each station),
beds or examination couches, patient screen, signages, room heater or
cooler
TIMING
DEVICE: Stop watch or bell
STATIONERY:
Score sheets, checklists, answer scripts, pens/ pencils
MANPOWER:
Nurses, orderlies, simulated/ real patients, helpers/marshals
CATERING:
Drinking water and food (snacks and lunch)
Station Specific |
|
Station |
Station description |
Basic equipment |
Specific needs |
Patient |
| No. |
|
|
|
requirement |
| 1 |
Data interpretation |
Table, 1 chair |
Calculator |
– |
| 2 |
Clinical examination of CNS |
Patient screen, examination |
Patellar hammer, |
4
simulated |
| |
|
couch/ warmer, 2 chairs, |
cotton wisps, tuning |
patients, |
| |
|
heater/blower, handrub, |
fork, |
|
| |
|
paper
napkins |
|
|
| 3 |
Equipment: Phototherapy |
Writing desk, 1 chair |
Phototherapy equipment |
|
| |
|
|
with duly labeled |
|
| |
|
|
parts/components |
– |
| 4 |
Rest station |
Table, 1chair |
A
tray with biscuits, |
|
| |
|
|
napkins |
– |
| 5 |
Clinical photographs |
Mounting board, writing |
A
chart with affixed |
|
| |
|
desk, 1
chair |
and
labeled photographs |
– |
TABLE II
Factors Affecting the Usefulness of OSCE as an Assessment Tool
| Factor |
Limitation |
| Number of stations |
Requires min 14-18 stations(1). Lesser
the number-lesser the reliability(29), and lesser the content validity |
| Time for assessment |
Lesser the time-lesser the reliability. A
10 minute station is more reliable as compared to a 5 minute
station(25, 30) |
| Unreliably standardised patients |
Limits reliability and validity |
| Individualised way of scoring |
Limits reliability |
| Assessing only one component at a time |
Limits validity(4) |
| Lack of item-analysis |
Affects reliability(26) |
| Skill of the person preparing the
checklist |
May hamper objectivity; limits validity
and reliability |
| Number of procedure stations |
Lesser the number, lesser the clinical
competencies that can be tested. Content specificity of stations
limits reliability |
| Identification and deletion of problem
stations |
Increases reliability(26) |
| Task specific checklists |
May not exactly replicate an actual
clinical encounter, limits validity(13) |
| Blueprinting |
Increases the content validity(10) |
| Competencies assessed |
Not useful for assessing the learning
behaviour, dedication to patients, and longitudinal care of
patients(4) |
| Expensive and labor-intensive |
Limits practicality and feasibility(31) |
However, there is a Mr Hyde side to this Dr Jekyll.
Table II outlines the factors that can affect the
generalisabilty, validity, reliability and practicality of OSCE. The OSCE
remains a toothless exercise if these factors are not taken care of.
Unfortunately that is what is happening at most of the places where OSCE
is now being introduced.
Feasibility and Practicality
It is agreed that setting and running an OSCE is very
resource intensive in terms of manpower, labor, time, and money; requires
very careful organization; and meticulous planning(4). Training of
examiners and patients, and preparation of stations and their checklists
is a time consuming affair. Cost is high, both in human resource needs and
money expended - patient (actor) payment, trainer payment, building
rental or utilities, personnel payment, student time, case development,
patient training, people to monitor, video taping etc. Most OSCEs are
administered in medical center outpatient facilities. A separate room or
cubical is needed for each station and this may be difficult to administer
in smaller set-ups.
The problem is more acute in the developing countries
and resource poor settings where a medical teacher has to assume the role
of a consultant, service provider, researcher and administrator. This way,
there is not much time the educator can spend on planning, preparing and
executing an OSCE. This results in an OSCE which is more of an artefact
and less of a true assessment.
Objectivity
The objectivity of OSCE is determined by the skill of
the experts who prepare the OSCE stations and the checklists. Over the
years, however, enthusiasm in developing detailed checklist (for
increasing the objectivity) has led to another problem i.e. "trivialisation."
The task is fragmented in to too many small components; and all of them
may not be clinically relevant for managing a patient. A higher
objectivity also does not imply higher reliability and that global ratings
(which are by and large subjective) are a superior tool for assessment,
especially in the hands of experienced examiners. An agreement has to be
reached whether replacing the checklists by global rating on particular
stations would improve the overall reliability, and then the OSCE can
include both types of assessment tools.
Validity
Content validity can only be ensured by proper
blueprinting(8). Following this, each task must be standardized and there
must be itemization of its components using appropriate scoring
checklists. Blueprinting also ensures multimodality OSCE that increases
the content validity(19). Feedback from the examiners and the students can
help in further improving the validity.
OSCE is not suited to assess the competencies related
to characteristics like longitudinal care of patients, sincerity and
dedication of the examinee to patient care and long-term learning habits
(consequential validity)(20,21).
Mavis, et al.(21) have questioned the validity
of OSCE by arguing that "observing a student perform a physical
examination in OSCE is not performance based assessment unless data from
this task is used to generate a master problem list or management
strategy." Brown, et al.(23) have questioned the predictive and
concurrent validity of OSCE by observing that the correlation between the
students’ result on OSCE and other assessment tools is low.
It would be appropriate to use OSCE to assess specific
clinical skills (psychomotor domain) and combine it with other methods to
judge the overall competency. Verma and Singh(24) concluded that OSCE
needs to be combined with clinical case presentation for a comprehensive
assessment. Panzarella and Manyon(25) have recently suggested a model for
integrated assessment of clinical competence studded with supportive
features of OSCE (ISPE: integrated standardized patient examination) to
increase the overall validity.
Reliability of OSCE on its own is less than desirable
There are some issues related to reliability which need
to be cleared for a proper understanding. Reliability does not simply mean
reproducibility of results (for which, objectivity is a better term)-
rather, reliability refers to the degree of confidence that we can place
in our results (i.e. if we are certifying a student as competent, then how
confident we are that he is really competent). This way of looking at
reliability of educational assessment is different from the way we look at
the reliability of say a biochemical test. It also needs to be understood
that reliability is not the intrinsic quality of a tool; rather it refers
to the inferences we draw from the use of that tool.
Reliability is generally content specific, meaning
thereby that it is difficult to predict that if a student has done well on
a case of CNS, he will do well on a case of anemia also.
Various factors can make results of OSCE less reliable
include fewer stations, poor sampling, trivialization of the tasks,
inappropriate checklists, time constraints, lack of standardized patients,
trainer inconsistency, and student fatigue due to lengthy OSCEs. Leakage
of checklists and lack of integrity of both examiners as well as students
can seriously compromise the validity as well reliability. A lot of
variation has been reported when different raters have observed a station,
and also between the performance from one station to another.
High levels of reliability (minimum acceptable defined
as the reliability co-efficient of 0.8, maximum achievable: 1.0) can be
achieved only with a longer OSCE session (of 4-8 h)(19). The reliability
of a 1 and 2 h session is as low as 0.54 and 0.69, respectively; which is
lower than the reliability of a case presentation of similar duration; but
which can be increased to 0.82 and 0.9 in a 4 or 8 h session,
respectively(21). However, it is impractical to conduct an OSCE of more
than 3 hours duration. Newble and Swanson(26) were able to increase the
reliability of a 90 min OSCE from 0.6 to 0.8 by combining it with a 90
minute free-response item written test.
Item analysis of OSCE stations and exclusion of problem
stations is a useful exercise to improve the reliability(27). By ensuring
content validity and by increasing the number of stations so that enough
items can be sampled, reliability can be improved. All students should
encounter similar test situation and similar real or simulated patients.
Where it is difficult to arrange for similar real patients, it would be
better to use simulated patients. However, arranging for children as
simulated patients is usually not possible.
Students’ perception of OSCE
Care should be exercised when introducing OSCE,
specially if students have not experienced earlier (e.g. in basic
sciences) because performing a procedure in front of an observer can be
threatening to many students. Although the examiner is not required to say
anything while observing the student, his/her body language can convey lot
of anxiety. There have been reports to suggest that students do feel
anxious initially(24,28). However, once explained the purpose and utility
of direct observation in providing a good feedback and making learning
better, acceptance is generally good.
Traditional OSCE does not integrate competencies
The OSCE model suggested by Harden revolves around the
basic principle of "one competency-one task-one station." Skills were
assessed in an isolated manner within a short time span. This does not
happen in a real life scenario where the student has to perform all his
skills in an integrated manner with the ultimate aim to benefit the
individual and the community. The modern educational theory also
stipulates that integration of tasks facilitates learning(21). It is thus
imperative that the OSCE moves towards integrated assessment. For example
dietary history taking and nutritional counseling can be integrated at one
Station; similarly, chest examination and advising chest physiotherapy
(based on the physical findings) can be integrated.
There are important implications of these aspects in
the design of OSCE. There is a general agreement now that everything that
is objective is not necessarily reliable; and conversely, all that is
subjective is not always unreliable. It is also accepted that the
advantages of OSCE do not relate to its objectivity or structure. If it
was so, then the reliability of even a one hour OSCE would also have been
high. Rather, the benefits seem to accrue from a wider sampling and use of
multiple examiners, both of which help to overcome the threats to validity
and reliability of assessment.
OSCE should not be seen as a replacement for something
- for example, a case presentation or viva; rather it should be
supplementing other tools. Using multiple tools helps to improve the
reliability of assessment by taking care of content specificity and
inter-rater variability. At the same time, one should not be
over-enthusiastic to use OSCE type examination for competencies, which can
be effectively tested by means of a written examination.
Indian Experiences with OSCE
OSCE has been by and large used as an assessment tool
for formative assessment of undergraduate medical students at a few
centers(5,24,29). Most of the faculty is not oriented to its use, and not
many universities have incorporated it in summative assessment plan for
the undergraduates. Probably this is because the Medical Council of India
has yet to recognise and recommend it as an acceptable tool for summative
assessment. Another main reason for hesitancy, we feel, is the lack of
training and time required on part of the faculty to initiate and sustain
a quality OSCE.
National Board of Examination, Ministry of Health and
Family Welfare, India has been using OSCE for summative assessment of
postgraduate students for certification in the subjects of Otolaryngology,
Ophthalmology, and Pediatrics for last few years. However, we feel that
there are concerns as to the validity, reliability, scoring pattern and
setting the standard in these examinations. For examples, there are only 6
procedure (observed) stations in a 24-30 station OSCE. The rest are based
on recall and application of knowledge; for which more cost-effective
testing tools are available. Many OSCE stations sample a very basic skill
without relating them to a real life clinical situation. Most of the time,
normal individuals are used as patient material. The standardized
simulated patients include student nurse or a resident, who has not been
trained specifically for this task. He/she is picked up only a few minutes
before the exam. It is difficult to obtain uniformity in marking and
inter-rater variability is likely to be more since the test is run
concurrently at more than one center, spread all over India. There is no
formal feedback given to the students or to the examiners to improve their
performance. Finally, the passing standard is set arbitrarily at 50% which
is not only not in conformity either with the accepted Angoff or
Borderline approach but also obtained by adding the scores of multiple
tools of variable reliability. Thus the OSCE pattern has limited validity
and reliability and there is need for a re-look – either the present
system be strengthened, or alternative methods should replace them.
Conclusions
It is generally agreed that OSCE is a tool of
assessment that tests competency in fragments and is not entirely
replicable in real life scenarios. OSCE is useful for formative
assessment, however on its own, it cannot be relied upon to fulfil the
three necessary pre-requisites for a summative assessment as laid down by
Epstein(30) i.e., promote future learning, protect the public by
identifying incompetent physicians, and choosing candidates for further
training. Limited generalizability, weak linkages to curriculum, and
little opportunity provided for improvement in examinees’ skill have been
cited as the reasons for replacing OSCE with alternative methods in
certain medical schools(22).
On a closer look there are gaps with respect to
objectivity, validity and reliability of this assessment, especially in
resource poor settings. It is costly and time consuming. It requires
special effort and money to design OSCE stations needed to measure the
essential professional competencies including ability to work in a team,
professional ethical behavior, and ability to reflect on own
(self-appraisal). For a summative assessment, OSCE should not constitute
more than one-third of the total evaluation scheme and as far as possible,
its grades should be reported separately. The need of the hour is an
integrated multiplanar (3 dimensional) 360° assessment in its true
perspective, of which OSCE can be a vital component.
Funding: None.
Competing interests: None stated.
References
1. Accreditation Council for Graduate Medical
Education (ACGME). Outcome Project. http://acgme.org/Outcome/. Accessed
on 23 July, 2009.
2. Epstein RM, Hundert EM. Defining and assessing
professional competence. JAMA 2002; 287: 226-235.
3. Harden RM, Stevenson W, Downie WW, Wilson GM.
Assessment of clinical competence using an objective structured clinical
examination. Br Med J 1975; 1: 447-451.
4. Harden RM, Gleeson FA. Assessment of clinical
competence using objective structure clinical examination (OSCE). Med
Edu 1979; 13: 41-54.
5. Gupta P, Bisht HJ. A practical approach to running
an objective structured clinical examination in neonatology for the
formative assessment of undergraduate students. Indian Pediatr 2001; 38:
500-513.
6. Boursicot K, Roberts T. How to set up an OSCE.
Clin Teach 2005; 2: 16-20.
7. Waas V, van der Vleuten CPM. The long case. Med
Edu 2004; 38: 1176-1180.
8. Newble D. Techniques of measuring clinical
competence: objective structured clinical examination. Med Edu 2004; 38:
199-203.
9. Angoff WH. Scales, norms and equivalent scores.
In: Thorndike RL, ed. Educational Measurement. Washington, DC:
American Council on Education; 1971. p. 508-600.
10. Boursicot KAM, Roberts TE, Pell G. Using
borderline methods to compare passing standards for OSCEs at graduation
across three medical schools. Med Edu 2007; 41: 1024-1031.
11. Kaufman DM, Mann KV, Muijtjens AMM, van der
Vleuten CPM. A comparison of standard setting procedures for an OSCE in
undergraduate medical education. Acad Med 2001; 75: 267-271.
12. Dauphinee WD, Blackmore DE, Smee SM, Rothman AI,
Reznick RK. Using the judgements of physician examiners in setting the
standards for a national multi-center high stakes OSCE. Adv Health Sci
Educ: Theory Pract 1997; 2: 201-211.
13. Smee SM, Blackmore DE. Setting standards for an
objective structured clinical examination: the borderline group method
gains ground on Angoff. Med Edu 2001; 35: 1009-1010.
14. Wilkinson TJ, Newble DI, Frampton CM. Standard
setting in an objective structured clinical examination: use of global
ratings of borderline performance to determine the passing score. Med
Edu 2001; 35: 1043-1049.
15. Cusimano MD. Standard setting in medical
education. Acad Med 1996; 71(suppl 10): S112-120.
16. Verma M, Singh T. Experiences with objective
structured clinical examination (OSCE) as a tool for formative
assessment in Pediatrics. Indian Pediatr 1993; 30: 699-702.
17. Reznick RK, Regehr G, Yee G, Rothman A, Blackmore
D, Dauphinee D. Process-rating forms versus task-specific checklists in
an OSCE for medical licensure. Acad Med 1998; 73: S97-99.
18. Regehr G, MacRae H, Reznick RK, Szalay D.
Comparing the psychometric properties of checklists and global rating
scales for assessing performance on an OSCE-format examination. Acad Med
1998; 73: 993-997.
19. Walters K, Osborn D, Raven P. The development,
validity and reliability of a multimodality objective structured
clinical examination in psychiatry. Med Edu 2005; 39: 292-298.
20. Barman A. Critiques on the Objective Structured
Clinical Examination. Ann Acad Med Singapore 2005; 34: 478-482
21. van der Vleuten CPM, Schuwirth WT. Assessing
professional competence: from methods to programmes. Med Edu 2005; 39:
309-317.
22. Mavis BE, Henry RC, Ogle KS, Hoppe RB. The
Emperor’s new clothes: OSCE reassessed. Acad Med 1996; 71: 447-453.
23. Brown B, Roberts J, Rankin J, Stevens B, Tompkins
C, Patton D. Further developments in assessing clinical competence.
In: Hart IR, Harden RM, Walton HJ, eds. Further developments in
assessing clinical competence. Montreal: Canadian Health Publications;
1987 .p. 563-571.
24. Verma M, Singh T. Attitudes of Medical students
towards objective structured clinical examination (OSCE) in pediatrics.
Indian Pediatr 1993; 30: 1259-1261.
25. Panzarella KJ, Manyon AT. A model for integrated
assessment of clinical competence. J Allied Health 2007; 36: 157-164.
26. Newble D, Swanson D. Psychometric characteristics
of the objective structured clinical examination. Med Edu 1988; 22:
325-334.
27. Auewarakul C, Downing SM, Praditsuwan R,
Jaturatamrong U. Item analysis to improve reliability for an internal
medicine undergraduate OSCE. Adv Health Sci Edu 2005; 10: 105-113.
28. Natu MV, Singh T. Student’s opinion about OSPE in
pharmacology. Indian J Pharmacol 1994; 26: 188-89.
29. Mathews L, Menon J, Mani NS. Micro-OSCE for
assessment of undergraduates. Indian Pediatr 2004; 41: 159-163.
30. Epstein RM. Assessment in medical education. N Engl J Med 2007;
356: 387-396.
|
|
|
 |
|

