Congenital Hypomyelinating Neuropathy (CHP) is
characterized clinically by infantile hypotonia, due to distal muscle
weakness, areflexia and very slow nerve conduction velocities(<10
m/s)(1). Very few cases have been reported in literature(2-8). To our
knowledge no case is reported from India till date. We report a case of
congenital hypomyelinating neuropathy and its apparent good response to
steroids.
Case Report
An 11-month-old female baby born out of
nonconsanguineous marriage was admitted to our institution for
evaluation of delayed motor milestones and deformities in the limbs.
Both the parents and the sibling (3 years, male) were clinically normal.
The daughter of her paternal aunt died at the age of 3 years because of
pneumonia, that child also had significant motor delay.
The pregnancy and delivery was uneventful. There was
no history of decreased fetal movements in the antenatal period. The
baby cried immediately after birth and was feeding normally. Mother did
not recognize any abnormality in the baby till she was admitted with
pneumonia at the age of 3 months. When the respiratory infection was
controlled, mother noticed decreased move-ments of the lower limbs. The
baby kept the fists closed even after 3 months of age. The head
steadiness was attained only at 6 months and she could not turn over or
sit up by herself. The baby attained social smile at 2 months and was
able to say two words with meaning (at 11 months of age). Her mental
milestones were appropriate for age.
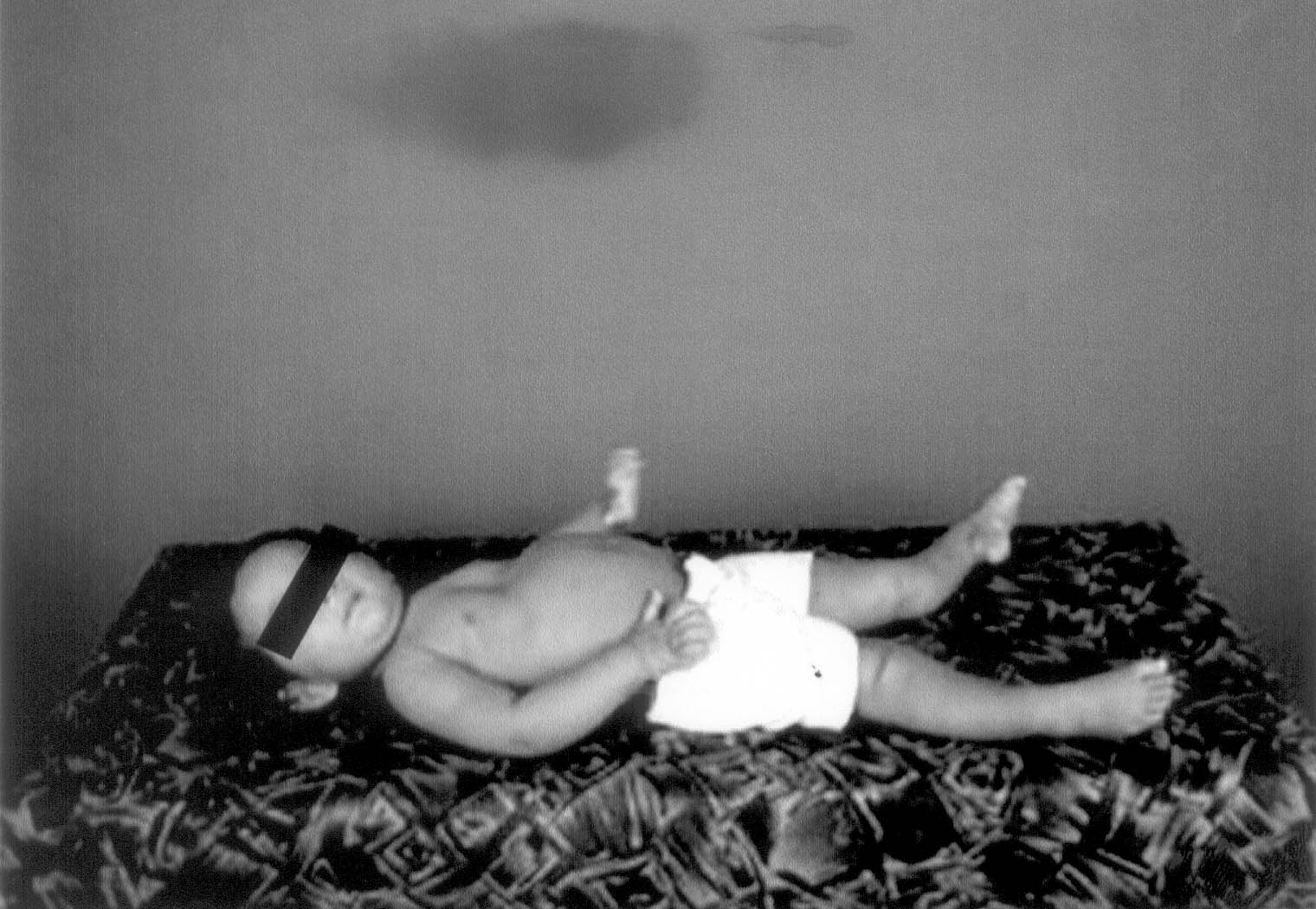
On examination the baby appeared alert, but
tachypneic. She had bilateral claw hands and talipes equinovarus with
contracture of tendoachilles. She was severely hypotonic and the knee
and hip joints were hyperextensible (Fig. 1). The weakness was
more for distal than proximal muscles and there was intercostal muscle
weakness. The deep tendon reflexes were absent bilaterally. Plantar
reflexes were flexor. There were no fasciculations over the tongue or
muscles. The baby cried when painful stimuli were given to the limbs.
The peripheral nerves were not palpably enlarged.
 |
|
Fig. 1. Note the intercostals weakness,
protuberant abdomen, claw hands, hyperextensible knee joints and
the clubfoot. |
The motor and sensory nerve potentials were
unobtainable in the upper and lower limbs. The needle EMG could not be
done, as the baby was too small to cooperate. Muscle enzymes were
normal. ECG, serum electro-lytes and urine aminogram were within normal
limits.
A muscle biopsy of the left gastronemius showed
relatively well-preserved architecture of muscle fascicles. The muscle
fibers showed mild degree of variation in fiber size, there was an
admixture of normal, atrophic as well as few hypertrophic fibers. There
were no evidence of inflammatory cellular infiltration or necrosis of
muscle fibers. NADH-TR preparation showed disarray in the mosaic pattern
of muscle fibers. The fibers were composed of both type 1 and type 2
fibers. The features were suggestive of changes due to denervation.
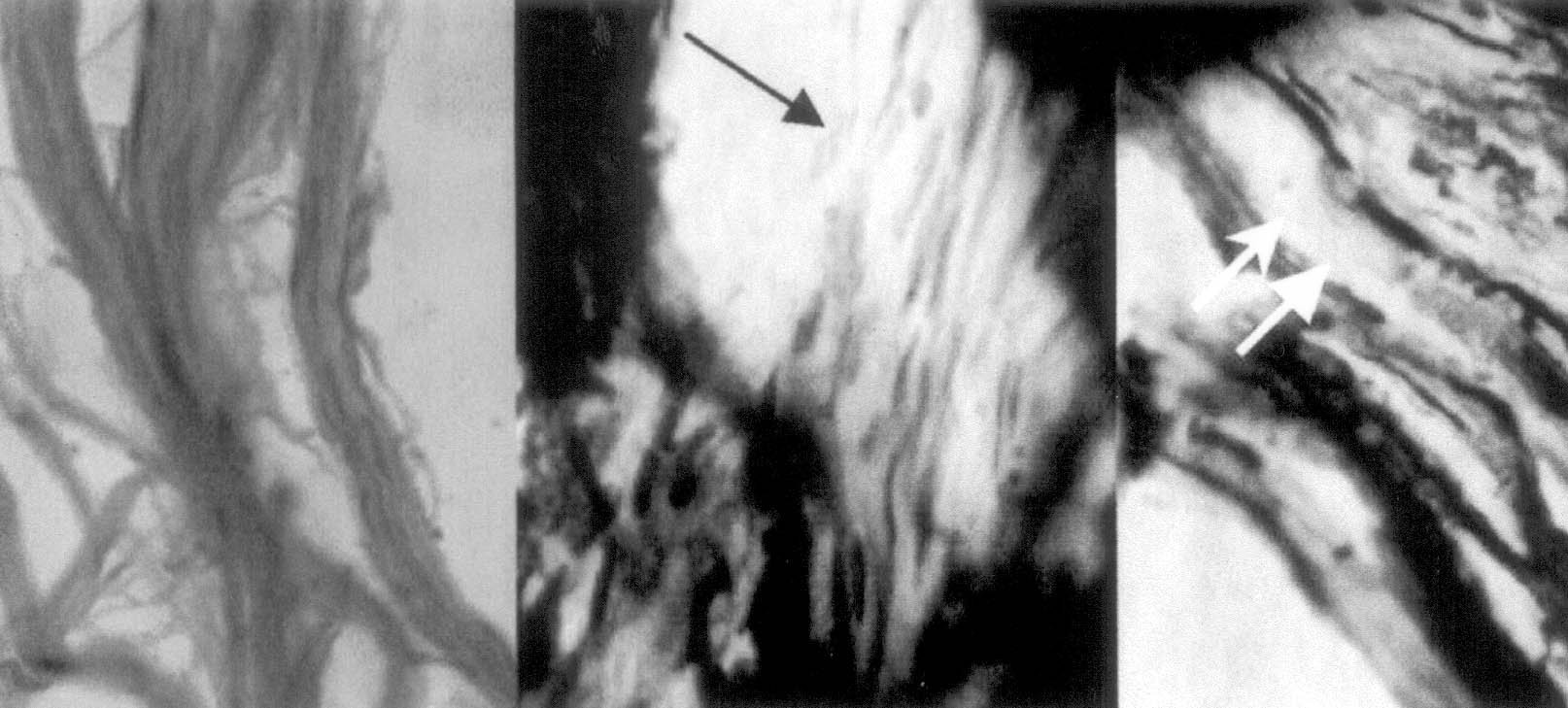
Sural nerve biopsy (Fig. 2) showed nerve
fibers with faintly discernible myelin and myelin was not visible at
many places. The axons appeared normal. There were no onion bulb
formation or features of demyelination or remyelination. Electron
microscopy was not done due to technical reasons. The clinical and
investigatory findings pointed towards a diagnosis of peripheral
neuropathy. Among the peripheral neuropathies presenting at this age,
Dejerine Sottas disease and congenital hypomyelinating neuropathy are
the important differential diagnoses. In Dejerine Sottas disease, the
nerve fibers are often palpably enlarged and nerve fibers show evidence
of demyelinatin and attempts at remyelination in the form of onion bulb
formation. The fact that myelin was not discernable in many of the nerve
fibers, the relative lack of myelination rather than the destruction of
already formed myelin in the biopsy specimen supports the diagnosis of
congenital hypomyelinating neuropathy.
 |
|
Fig. 2. Sural nerve biopsy, (H&E and Weigert
stain) showing nerve fibers with faintly discernible myelin in
areas (double arrow) and areas where myelin is not visible (single
arrow). |
The baby was put on steroids (Prednisolone lmg/kg/day
) in addition to the regular home physiotherapy. On follow up visit, one
month after starting steroid she did show improvement in motor
milestones. She was able to sit without support and the clawing was
reduced. However nerve conduction velocities remained unobtainable.
Discussion
In 1969 Lyon described a case of infantile neuropathy
whose nerve biopsy showed absence of myelin and normal axon(2). The baby
had marked delay of motor milestones, hypotonia, weakness of lower
limbs, areflexia and normal mental milestones. The peripheral nerves
were not palpable and nerve conduction velocities were unmeasurable.
Later various authors have described isolated reports. The most severe
cases are associated with decreased fetal movement(4) and may present as
arthrogryposis multiplex congenita at birth(5). Most of these children
die in infancy or early childhood with respiratory muscle weakness and
pneumonia. Some cases are slowly progressive or nonprogressive. They
attain milestones at a slow pace, but will have residual disability and
ataxia due to involvement of large myelinated sensory fiber(3).
In CHP, there is primary hypomyelination of
peripheral nerve secondary to a defect in Schwann cells. The axons are
normal, there is only minimal onion bulb formation. The level of myelin
lipid is found to be low in this condition(3). The condition has
similarities with the hereditary motor sensory neuropathy of Dejerine
and Sottas. But in this condition there is evidence for
demyelination-remyelination with typical Schwann cell onion bulb
formation and myelin breakdown. The nerves are often hypertrophied and
palp-ably enlarged in this condition(9). Some consider congenital
hypomyelinating neuro-pathy as a subset of Dejerine Sottas syndrome.
The commonest differential diagnoses in a floppy baby
with normal mental milestones are spinal muscular atrophy and certain
congenital myopathies. But the weakness is more proximal than distal in
these conditions. Areflexia and fasciculations of the tongue are common
in SMA; ankle jerk is retained till late in myopathies. The nerve
conduction velocities remain normal and the EMG shows a neuropathic or
myopathic pattern respectively. The muscle biopsy with histo-chemistry
is diagnostic in both these conditions.
The inheritance pattern in congenital hypomyelinating
neuropathy has been described as autosomal dominant or recessive. The
cousin of this child died of similar illness at 3 years of age. As no
genetic studies were done in our case no inference could be obtained.
Mutation in myelin protein zero gene and the early growth response gene
has been described in CHP(8).
CHP is a disease, which shows wide variability in
progression. Many die in early infancy, some may gain milestones even
though the nerve conduction velocities remain low. Those who are able to
walk are ataxic due to affection of the large myelinated sensory
fiber(7). The role of steroids is inconclusive. There are isolated case
reports showing beneficial effect with steroids(10). Our patient showed
significant improvement within one month of low dose steroids and is
still on steroids.
Contributors: SRC was involved in acquisition,
analysis and interpretation of clinical data, and final approval of the
version and will act as the guarantor of the paper. DK was involved in
the clinical work up and investigations and drafting of manuscript. VVR
and SRS analyzed the muscle and nerve biopsy respectively, interpreted
the results and helped in drafting the article.
Funding: None.
Competing interests: None stated.
