|
|
|
Indian Pediatr 2017;54: 373-376 |
 |
Contextual Factors for Stunting Among Children of Age 6 to 24
Months in an Under-Privileged Community of Dhaka, Bangladesh
|
|
Md Ashraful Alam, Mustafa Mahfuz, M Munirul Islam,
Dinesh Mondal, AMS Ahmed, Rashidul Haque,
Tahmeed Ahmed and Md Iqbal Hossain
From Nutrition and Clinical Services Division,
icddr,b, Mohakhali, Dhaka, Bangladesh.
Correspondence to: Dr Md Iqbal Hossain, Senior
Scientist, Nutrition Research and Clinical Services Division, icddr,b,
Mohakhali, Dhaka 1212, Bangladesh.
Email: [email protected]
Received: January 02, 2016;
Initial review: October 14, 2016;
Accepted: February 23, 2017.
Published online: March 29, 2017.
PII:S097475591600060
|
Objective: To determine factors associated with
stunting among children aged 6 to 24 months in a slum of Dhaka,
Bangladesh. Methods: We conducted this case control study during
November 2009 to December 2012. Children were classified as case if
length-for-age Z-score (LAZ) was <-2 and as control if LAZ was
>-1 SD. The logistic regression model was used to find the factors
associated with stunting. Results: The significant risk factors
for stunting were: childís age >12 months, maternal undernutrition,
motherís education <5 years, consumption of untreated drinking water and
monthly family income <100 USD. Conclusion: The findings of this
study reiterated the role of maternal undernutrition and less education,
consumption of untreated drinking water and poor family income as
important associated factors of childhood stunting in resource-poor
setting.
Keywords: Epidemiology, Risk Factors, Undernutrition.
|
|
C
hildhood malnutrition is one of the most common
causes of morbidity and mortality among under-Five children in the
world. Stunting is the most common form of undernutrition in Bangladesh
and other low-income countries. Stunting reflects the cumulative effect
of chronic undernutrition status and refers to low length- or
height-for-age that is a failure to reach linear growth potential due to
inadequate dietary intakes and health conditions accumulated during
early childhood [1]. It has long-term severe effects on individuals as
well as societies, including: decreased cognitive and physical
development, reduced productive capacity and poor health, increased risk
of degenerative diseases [2]. Globally the prevalence of stunting among
under-five children decreased from 39.7% to 26.7% and in developing
countries from 44.4% to 29.2% over a period of 1990 to 2010 [3]. In
Bangladesh, the prevalence of stunting among under-five children has
been decreasing slowly (from 63% in 1990 to 36% in 2014), but still it
is very high. Though stunting is a great public health concern in
Bangladesh, there are very few studies to identify the factors related
to stunting. Thus, the purpose of this study was to identify factors
associated with stunting in children of age 6 to 24 months in a slum of
Bangladesh.
Methods
This study was performed within the ongoing Mal-ED
(Etiology, Risk Factors, and Interactions of Enteric Infections and
Malnutrition and the Consequences for Child Health) study [4]. The
Mal-ED study (icddr,b protocol # 2008-020) was approved by the Research
Review Committee and the Ethical Review Committee of icddr,b in 2008.
For participation in this study, written informed consent was obtained
from the guardians of each participating child. With case-control
design, the study was conducted among residents of an under-privileged
urban community in Bauniabadh slum in Mirpur, Dhaka, Bangladesh [5].
Cases were stunted children length-for-age z-score (LAZ) < -2 of the
median of a WHO standard aged 6 to 24 months. Controls were
well-nourished children aged 6 to 24 months with LAZ > -1.
Field research assistants (FRAs) were trained to
identify source population of cases and controls, through obtaining the
anthropometric measurements of each child. FRAs measured child body
weight and length in the study clinic. Also FRAs measured mother body
weight and height. Child body weight was taken without any cloth by the
digital scale (Seca 354) to nearest 10 g and length by Infantometer/length
measuring board (Seca 416) to nearest 0.1 cm. Ages of children were
validated by checking the childís immunization card. Z-scores for
length-for-age (LAZ), weight-for-age (WAZ), and weight-for-length (WLZ)
were calculated using WHO Anthro Software version 3.1.0. Motherís body
weight and height were also recorded. Body mass index (BMI) was
calculated using the formula BMI = weight in kg/(height in m) 2.
FRAs also interviewed the mothers using a pretested,
structured questionnaire. Information collected from the interviews
included: age and sex of child, colostrum and breastfeeding practices,
motherís age at first pregnancy, parental education, family size,
information about drinking water and latrine, and monthly family income.
Household food security was evaluated using Household Food Insecurity
Access Scale (HFIAS) generic questions [6], and was categorized as per
HFIASís guideline [6].
Data were entered into Microsoft Office Access and
exported to STATA 13 for analysis. Dual data entry method was used to
minimize data entry error. Bivariate analysis was done for all
explanatory variables to identify those associated with children
stunting. Only significant variables in the bivariate analysis were
included in logistic regression model. Odds ratios (95% confidence
intervals) were calculated to identify the factors associated with
stunting, and P-value <0.05 was considered statistically
significant.
Results
Total 689 children (389 cases and 300 controls)
participated in this case control study. In bivariate analysis, we found
significant association of stunting with childís age, maternal
undernutrition and education, household headís education, treatment of
drinking water, sharing toilet, monthly family income, food insecurity,
and hand washing habits (Table I). No association was
found with childís gender, breastfeeding and complementary feeding
practice, motherís age at first pregnancy, family size, and morbidity (Table
I).
TABLE I Socio-demographic Characteristics, Nutritional Practice and Hands Washing Habits of Study Population
|
Characteristics |
Cases (%)
n=389 |
Controls (%)n=300 |
Crude OR
(95% CI) |
|
Age group (mo) |
|
|
|
|
6-11 |
133 (34.2) |
185 (61.7) |
Ref |
|
12-17 |
137 (35.2) |
68 (22.7) |
2.80 (1.94, 4.04) |
|
18-24 |
119 (30.6) |
47 (15.7) |
3.52 (2.35, 5.28) |
|
Child sex (female) |
174 (44.7) |
154 (51.3) |
0.77 (0.57, 1.04) |
|
Lack of exclusive breastfeeding (<180 d) |
305 (78.4) |
219 (73.0) |
1.34 (0.76, 1.41) |
|
Lack of practice optimum IYCF |
226 (58.1) |
189 (63.0) |
0.81 (0.60, 1.11) |
|
Colostrum not given |
26 (6.7) |
15 (5.0) |
1.36 (0.71, 2.62) |
|
Prelacteal feeding |
122 (31.4) |
83 (27.7) |
1.19 (0.86, 1.66) |
|
Breastfeeding started after one hour of birth |
180 (46.3) |
133 (44.3) |
1.08 (0.80, 1.46) |
|
Motherís BMI <18.5 |
147 (38.0) |
46 (15.4) |
3.36 (2.31, 4.88) |
|
Motherís education <5 y |
216 (55.5) |
120 (40.0) |
1.87 (1.38, 2.54) |
|
Household headís education <5 y |
197 (52.0) |
128 (44.0) |
1.37 (1.01, 1.87) |
|
Motherís age at first pregnancy <18 y |
142 (36.6) |
101 (33.8) |
1.13 (0.82, 1.55) |
|
Family size >4 |
161 (41.4) |
137 (45.7) |
0.84 (0.62, 1.14) |
|
Untreated drinking water |
157 (40.4) |
79 (26.3) |
1.89 (1.36, 2.63) |
|
Sharing toilet with other households |
357 (91.8) |
246 (82.0) |
2.45 (1.54, 3.90) |
|
Monthly family income <100 USD* |
233 (59.9) |
117 (39.0) |
2.34 (1.72, 3.18) |
|
Household food insecurity |
194 (49.9) |
110 (36.7) |
1.72 (1.26, 2.34) |
|
Sometime or never wash hands after helping child defecate |
149 (38.3) |
92 (30.7) |
1.4 (1.02, 1.93) |
|
Sometime or never wash hands before preparing food |
305 (78.4) |
227 (75.7) |
1.17 (0.82, 1.67) |
|
Sometime or never wash hands after using the toilet |
110 (28.3) |
61 (20.3) |
1.54 (1.08, 2.21) |
|
Diarrhea in last 3 d |
15 (3.9) |
20 (6.9) |
0.55 (0.28, 1.10) |
|
Cough in last 3 d |
124 (32.3) |
84 (28.9) |
1.18 (0.84, 1.64) |
|
Fever in last 3 d |
51 (13.3) |
30 (10.3) |
1.33 (0.83, 2.15) |
|
IYCF: Infant and young child feeding; *One USD = 78
Bangladeshi taka. |
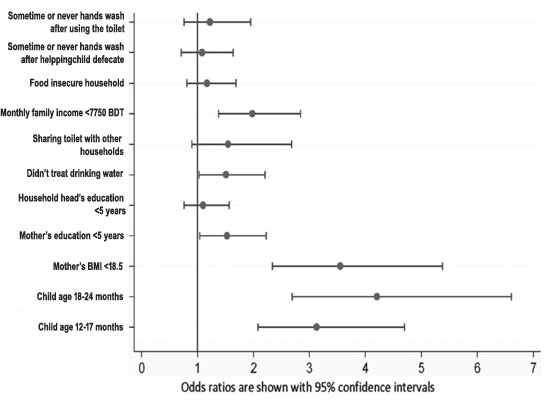
Logistic regression analysis revealed that the risk
factors for stunting were childís age >12 to 17 months (AOR 3.13, 95%
CI: 2.08, 4.70) and 18 to 24 months (AOR 4.21, 95% CI:2.69, 6.61);
motherís BMI <18.5 (AOR 3.55, 95% CI: 2.34, 5.38); motherís education <5
years (AOR1.53, 95% CI: 1.04, 2.23); consumption of untreated drinking
water (AOR 1.51, 95% CI: 1.03, 2.21); and monthly family income <100 USD
(AOR=1.98, 95% CI: 1.38, 2.84) (Fig. 1).
 |
|
Fig. 1 Adjusted odds ratios for risk
factors significantly associated with stunting.
|
Discussion
This study aimed to identify the factors associated
with stunting among children aged 6 to 24 months. Logistic regression
analysis identified that the factors significantly associated with
stunting were: (i) more than 12 months of childís age, ii)
motherís undernutrition (BMI <18.5), iii) motherís education less
than 5 years, iv) consumption of untreated drinking water, and v)
monthly family income less than 100 USD.
Limitation of the study is that there may be some
recall bias related to previous history recorded from mothers. Another
limitation is the data for this study emerged from only one slum of
Bangladesh.
Svefors, et al. [7] and Chowdhury, et al.
[8] also found that age group >12-24 months was a risk factor of
stunting. A recent study from Tanzania [9] also found maternal
under-nutrition as a risk factor. Less educated mother as a risk factor
of stunting is also echoed by other studies [9-11]. Educational level of
mother is vital because educated mothers can better access the health
services, usually provide better care, have better hygienic practices,
and also have higher status in the family. The effect of maternal
factors on infant outcomes has been described earlier [12]. We found
that untreated drinking water was another risk factor of stunting, and
the study by Chirande, et al. [9], from Tanzania also found
unsafe sources of drinking water as a risk factor of stunting.
The effect of income on stunting, as observed in our
study, can be explained by its importance in the purchase of food and
consumer goods that promote and protect the health of children. It is
also known that better economic conditions increase the living standard
of the families, which allow them to take essential care of the
children. The previous study from our group showed similar findings as
stunted children more often had short-statured, malnourished and
illiterate/less educated mothers, and were more often from lowest
quintile of asset index [13].
The findings of this study reiterate the role of
maternal nutritional status and education, quality of drinking water and
family income as important contextual factors of childhood stunting. Our
study recommends that to reduce the under-five stunting rate in the
slums, targeted programs should be developed to improve maternal
nutrition and education, drinking water and family income.
Acknowledgements: This research study was funded
by the Bill & Melinda Gates Foundation; the Foundation for the NIH; the
National Institutes of Health and Fogarty International Center funded
the MAL-ED project, and the core donors who provide unrestricted support
to icddr,b for its operations and research. Current donors providing
unrestricted support include: Government of the Peopleís Republic of
Bangladesh; the Department of Foreign Affairs, Trade and Development
(DFATD), Canada; Swedish International Development Cooperation Agency
(SIDA) and the Department for International Development (UK Aid). We
gratefully acknowledge these donors for their support and commitment to
icddr,bís research efforts.
Contributors: MAA, MM, MMI, DM, AMSA, RH, TA,
MIH: concept of study and data collection;. MAA, MM, TA, MIH: data
entry, cleaning and analysis.. All authors are responsible for writing
and revision of the draft.
Funding: Bill & Melinda Gates Foundation, and
icddr, b. Competing interest: None stated.
|
What This Study Adds?
ē
Maternal undernutrition and low education, low family
income, and poor quality of drinking water are associated with
stunting in 6-24 month old slum children in Bangladesh.
|
References
1. WHO Working Group. Use and interpretation of
anthropometric indicators of nutritional status. Bull World Health
Organ. 1986;64:929.
2. Winichagoon P, Kavle J, Mehanna S, Saleh G, Foaud
M, Ramzy M, et al. Global nutrition targets 2025: Stunting policy
brief. Food NutrBull. 2014;35:S27-33.
3. De Onis M, BlŲssner M, Borghi E. Prevalence and
trends of stunting among pre-school children, 1990-2020. Public Health
Nutr. 2012;15:142-8.
4. Acosta AM, Chavez CB, Flores JT, Olotegui MP,
Pinedo SR, Trigoso DR, et al. The MAL-ED Study: A multinational
and multidisciplinary approach to understand the relationship between
enteric pathogens, malnutrition, gut physiology, physical growth,
cognitive development, and immune responses in infants and children up
to 2 years of age in resource-poor environments. Clinical Infect Dis.
2014;59:193-206.
5. Ahmed T, Mahfuz M, Islam MM, Mondal D, Hossain MI,
Ahmed AS, et al. The MAL-ED cohort study in Mirpur, Bangladesh.
Clin Infect Dis. 2014;59:280-6.
6. Coates J, Swindale A, Bilinsky P. Household Food
Insecurity Access Scale (HFIAS) for Measurement of Food Access:
Indicator Guide. Washington, DC: Food and Nutrition Technical Assistance
Project, Academy for Educational Development. 2007.
7. Svefors P, Rahman A, EkstrŲm EC, Khan AI,
LindstrŲm E, Persson LŇ, et al. Stunted at 10 years. Linear
growth trajectories and stunting from birth to pre-adolescence in a
rural Bangladeshi cohort. PloS One. 2016;11:0149700.
8. Chowdhury MR, Rahman MS, Khan MM, Mondal MN,
Rahman MM, Billah B. Risk factors for child malnutrition in Bangladesh:
A multilevel analysis of a nationwide population-based survey. J Pediatr.
2016;172:194-201.
9. Chirande L, Charwe D, Mbwana H, Victor R, Kimboka
S, Issaka AI, et al. Determinants of stunting and severe stunting
among under-fives in Tanzania: evidence from the 2010 cross-sectional
household survey. BMC Pediatr. 2015;15:1.
10. Hasan MT, Soares Magalhaes RJ, Williams GM, Mamun
AA. The role of maternal education in the 15 year trajectory of
malnutrition in children under 5 years of age in Bangladesh. Matern
Child Nutr. 2016;12:929-39.
11. Semba RD, De Pee S, Sun K, Sari M, Akhter N,
Bloem MW. Effect of parental formal education on risk of child stunting
in Indonesia and Bangladesh: a cross-sectional study. Lancet.
2008;371:322-8.
12. Sinha S, Aggarwal AR, Osmond C, Fall CHD,
Bhargava SK, Sachdev HS. Maternal age of childbirth and perinatal and
under-five mortality in a prospective birth cohort from Delhi. Indian
Pediatr. 2016;53:871-7.
13. Ahmed AM, Ahmed T, Roy SK, Alam N, Hossain MI.
Determinants of under nutrition in children under 2 years of age from
Rural Bangladesh. Indian Pediatr. 2012;49: 821-4.
|
|
|
 |
|

