|
|
|
Indian Pediatr 2016;53: 435-436 |
 |
High Mobility Group Box 1 in Preterm Infants
with Intraventricular Hemorrhage
|
|
Jianglin Ma and #*Hongyan
Lu
Department of Pediatrics, The First Affiliated
Hospital, College of Medicine, Zhejiang University, Hangzhou, and #Department
of Pediatrics, The Affiliated Hospital of Jiangsu University, Zhenjiang,
Jiangsu; China.
Email: *[email protected]
|
|
We studied the level of high mobility
group box 1(HMGB1) in preterm infants with intraventricular hemorrhage
(IVH). Using enzyme-linked immunosorbent assay (ELISA), the
concentration of HMGB1 in cord blood obtained from 41 infants with IVH
and 67 infants without IVH were measured. The cord blood concentration
of HMGB1 in infants with IVH were significantly higher than those
without IVH (P=0.041). Increased levels of HMGB1 might be
associated with IVH in preterm infants.
Keywords: HMGB1, Intraventricular Hemorrhage,
Prematurity.
|
|
Intraventricular hemorrhage (IVH) often occurs in
premature infants and results in increased morbidity and mortality in
survivors [1]. Intrauterine infection may predispose to IVH through
inflammation [2]. In this pathophysiological process, many
pro-inflammatory cytokines such as High mobility group box 1 (HMGB1) may
be involved. We conducted this study to explore relationship between
HMGB1 and IVH in preterm infants.
All infants enrolled in this study were delivered
less than 32 weeks of gestation and treated in the neonatal intensive
care unit (NICU) of the First Affiliated Hospital, College of Medicine,
Zhejiang University, China, between April 2012 and July 2014. Umbilical
venous blood was obtained from all infants immediately after birth, and
centrifuged at 2000 rpm for 10 min. The serum was separated and stored
at -70 şC before analysis. HMGB1 was measured with commercially
available ELISA kits (Shino-Test, Kanagawa, Japan) according to the
manufacturer’s recommendations.
The clinical data were collected from the infants’
records. Diagnosis of IVH was made by cranial ultrasonography. IVH was
classified in four grades [3]. Written informed consent was obtained
from one of the parents. The study was approved by the ethics committee
of the Affiliated Hospital of Jiangsu University.
Forty-one infants with IVH and 67 infants without IVH
were enrolled in this study. Of the 41 infants with IVH, 21 had grade I,
12 had grade II, 6 had grade III, and 2 had IV IVH. Other
characteristics of the participants are shown in Table I.
There were no significant differences in baseline characteristics
between the two groups.
TABLE I Characteristics of Participants in The Study
|
Intraventricular hemorrhage |
|
P value
|
|
Present (n=41) |
Absent (n=67) |
|
|
Gestational age (wk) |
30.6 (1.37) |
30.3 (1.15) |
0.656 |
|
Birth weight (g) |
1647 (207) |
1671 (187) |
0.813 |
|
Male |
25 |
39 |
0.776 |
|
Cesarean birth |
31 |
40 |
0.091 |
|
1 min Apgar |
8 (5-8) |
9(5-9) |
0.882 |
|
5 min Apgar |
9 (5-9) |
9(6-9) |
0.892 |
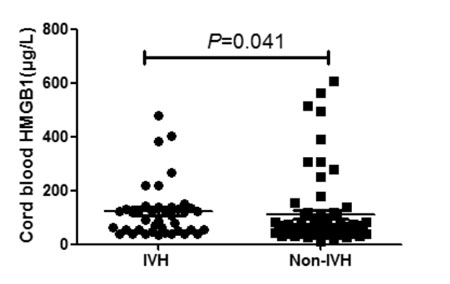
The levels of HMGB1 were 108.6 (37.3, 400.9) µg/L in
infants with IVH, and 61.5 (26.8,508.3) µg/L in infants without IVH. As
shown in Fig. 1, the levels of HMGB1 in infants with IVH
were significantly higher than in those without IVH (P=0.041).
There was no significant difference of HMGB1 levels among infants with
different grades of IVH.
 |
|
Fig. 1 Serum HMGB1 levels in
neonates with and without IVH.
|
In recent years, HMGB1 has been proposed as a late
mediator during inflammation [4]. Some researches demonstrated that
HMGB1 could play a critical role in inflammatory diseases, such as
tissue injury or sepsis [5]. However, the role of HMGB1 in IVH is not
exactly known. Our data suggest that HMGB1 might be involved in the
pathophysiology of IVH in preterm infants.
Contributors: Both authors have contributed,
designed and approved the study.
Funding: Jiangsu Province’s Scientific and
Technological Supporting Program (grant number BL2012058).
Competing interests: None stated.
References
1. Su BH, Hsieh WS, Hsu CH, Chang JH, Lien R, Lin CH.
Neonatal outcomes of extremely preterm infants from taiwan: Comparison
with Canada, Japan, and the USA. Pediatr Neonatol. 2015;56:46-52.
2. Gagliardi L, Rusconi F, Da Fre M, Mello G,
Carnielli V, Di Lallo D, et al. Pregnancy disorders leading to
very preterm birth influence neonatal outcomes: results of the
population- based ACTION cohort study. Pediatr Res. 2013;73:794-801.
3. Papile LA. Incidence and evolution of subependymal
and intraventricular hemorrhage: A study of infants with birth weights
less than 1,500 gm. J Pediatr. 1978;92:529-34.
4. Lee W, Kwon OK, Han MS, Lee YM, Kim SW, Kim KM,
et al. Role of moesin in HMGB1 stimulated severe inflammatory
responses. Thromb Haemost. 2015;114:350-63.
5. Yang H, Antoine DJ, Andersson U, Tracey KJ. The
many faces of HMGB1:Molecular structure-functional activity in
inflammation, apoptosis, and chemotaxis. J Leukoc Biol. 2013;93:865-73.
|
|
|
 |
|

