Khuram Arif
Zulfiqar Ahmed Bhutta
From the Department of Pediatrics, The Aga Khan University, Karachi.
Reprint requests: Dr. Zulfiqar Ahmed Bhutta, Professor of Child Health
and Neonatology, Department of Pediatrics, The Aga Khan University Hospital, Stadium Road, PO Box 3500, Karachi 74400, Pakistan.
Manuscript received: March 26,1998; Initial review completed: April 29, 1998;
Revision accepted: December
2, 1998.
Neonatal jaundice is a fairly common cause of morbidity in Pakistan and accounts for almost 25% of all newborn admissions(1). However, much of the data on neonatal hyperbilirubinemia
from Pakistan is based on outpatient referrals(2) and little information is
available on patterns of neonatal jaundice in birth cohorts. This may also
account for the wide variation in the etiology of jaundice from various reports
in Pakistan(2,3). Thus, although G6PD deficiency is a prominent cause of neonatal jaundice in the region( 4,5), there is scarce information about its significance in birth cohorts in Pakistan. This study was designed to describe the etiology of neonatal jaundice in a birth cohort at the Aga Khan University Medical Center (AKUMC) in
Karachi, Pakistan and to identify factors determining the severity of hyperbilirubinemia.
Subjects and Methods
We retrospectively evaluated all consecutive births at the AKUMC from January
1992 to December 1994. All newborn infants delivered at AKUMC during this period were evaluated and managed according to a standardized management protocol(6). As such, significant jaundice was defined as jaundice requiring phototherapy and/or exchange transfusion within the first seven days of life, and thus newborns with physiological or mild jaundice not requiring therapy were excluded from this analysis. Investigations obtained in all cases with significant jaundice included maternal and neonatal blood groups, Coombs test, serial levels of total serum bilirubin, direct bilirubin, hemoglobin and hematocrit, reticulocyte count, and peripheral blood smear. G6PD deficiency was screened in red cells by a qualitative, visual colorimetric method using dichlorophenol as dye (Sigma Diagnostics, USA).
Case records of all newborn infants were evaluated for details of the maternal antenatal history, labor, mode of presentation and therapy of jaundice in the first seven days of life. Cases were categorized according to the principal diagnosis based on the International Classification of Diseases (ICD V3.00- V39.01)(7). Patients. were divided into mutually exclusive diagnostic categories. For patients who had more than one contributory cause for jaundice, the 'principal diagnosis'
was used to categorize the primary etiology of their jaundice. Patients who could not be satisfactorily categorized to a single primary etiology were classified to have jaundice of 'Mixed' etiology. An etiology of 'Infection' was ascribed to jaundice in newborn infants with positive blood cultures and/or features of
infection necessitating antibiotics for
≥ 7 days, in the absence of other attributable causes. Newborn infants < 37 wks gestational age with significant hyperbilirubinemia who could not be categorized into any other major etiological category were considered to have 'Prematurity' associated jaundice. Newborn infants with 'Miscellaneous hemolyses' were defined as newborn infants with a Coombs positive test and/or abnormal peripheral smear who were neither ABO or Rh incompatible nor G6PD deficient. 'Exaggerated physiological jaundice' was defined as jaundice occurring after the 3rd day of life in a healthy, full term, breastfed infant who had no identifiable risk factors for jaundice and which settled by 10-14 days of age. Jaundiced newborn infants who could not be categorized into any of the aforementioned criteria were placed in an "Unknown" category.
Data was analyzed using SPSS (Statistical Package for Social Sciences version 6.1 SPSS Inc., Chicago, USA). Dichotomous variables were analyzed by univariate analysis, computation of odds ratios and corresponding 95% confidence intervals. Continuous data was analyzed using ANOV A and the unpaired two tailed t-test. Non-parametric data was analyzed using the Mann-Whitney U Test. Marginal and significant variables associated with severe jaundice requiring exchange transfusion were further evaluated in a logistic regression model with estimation of odds ratios and corresponding 95% confidence intervals. Significance was set at 5%.
Results
Of a total 5570 births during the study period the number of newborn infants requiring phototherapy and/or exchange transfusion was 869 (15.6/1000 live births) with a male to female ratio of 1: 1.3. The mean gestational age and birth weights were 37.2
± 2.8 wks and
2754
±
735 g, respectively. The diagnostic
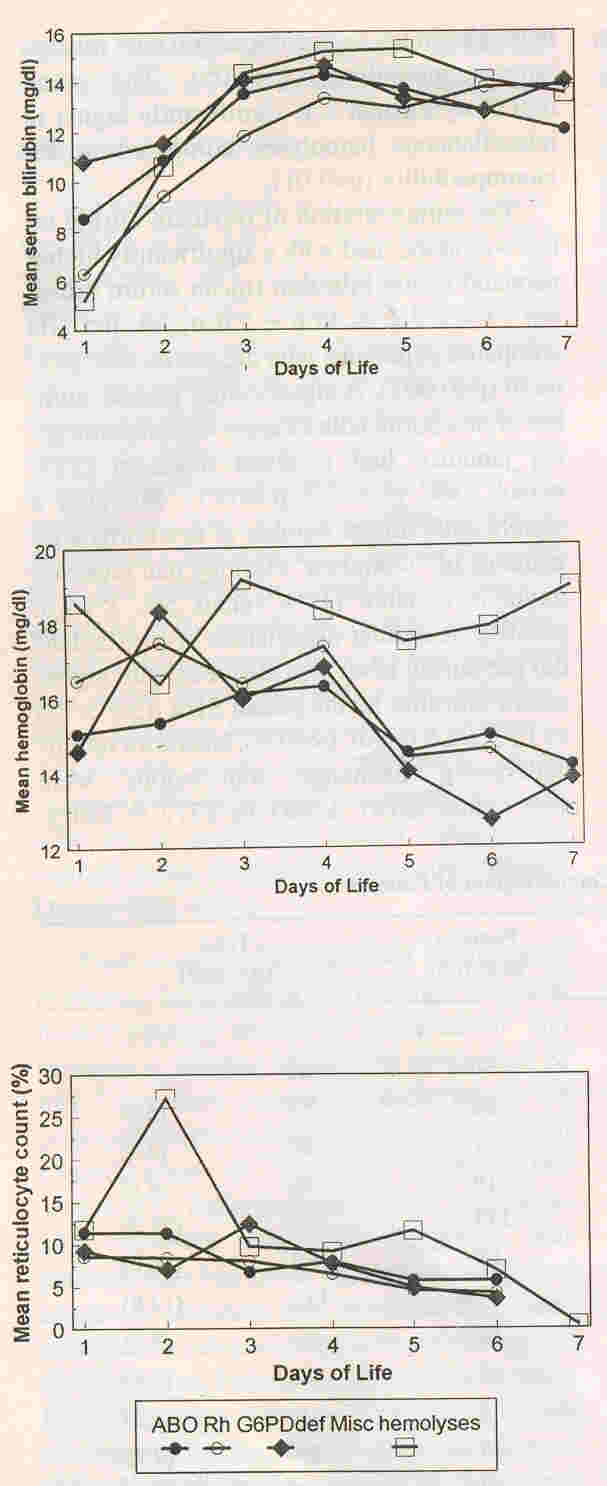
categories are shown in Table I. A large proportion (27.2%) of patients
did not have an ascribable pathology and were labeled as exaggerated physiological jaundice. Hemolytic jaundice comprised 19.9% and G6PD deficiency accounted for 2% of the study group. Double phototherapy was provided in 215 (24.7%) newborns and 27 (3%) required exchange transfusions. Figure 1 illustrates the trends for maximum serum bilirubin, minimum hemoglobin and maximum reticulocyte count in the subcategories of hemolytic jaundice. In Rhesus incompatibility patients mean serum bilirubin levels were significantly lower than in those with ABO incompatibility (p<0.01),
G6PD deficiency (p<0.05) and the miscellaneous subgroups (p<0.001). The mean
hemoglobin levels in ABO incompatibility were significantly lower than with Rh
incompatibility (p<0.01) and the miscellaneous hemolyses (p<0.001). Newborn
infants with ^PD deficiency also has lower mean hemoglobin levels in comparison with miscellaneous hemolyses
(p<0.05). The mean reticulocyte count was significantly higher in miscellaneous hemolyses compared to Rh incompatibility (p<0.01).
 |
|
Fig. 1 Trends
for mean serum bilirubin, hemoglobin and reticulocyte count over
days of life 1-7. |
Table I
Diagnostic Categorisation of Patients
|
Diagnostic Category |
Males (n-484) |
Females |
Total |
|
Hemolytic jaundice |
|
|
|
(%) |
|
ABO Incompatibility |
26 |
30 |
56 |
(6.4) |
|
Rh incompatibility |
28 |
29 |
57 |
(6.6) |
|
G6PD deficiency |
19 |
1 |
20 |
(2.3) |
|
Miscellaneous hemolyses |
21 |
19 |
40 |
(4.6) |
|
Exaggerated physiological |
123 |
113 |
236 |
(27.2) |
|
Infection |
96 |
69 |
165 |
(19.0) |
|
Prematurity |
64 |
47 |
111 |
(12.8) |
| Infants
of diabetic mother |
17 |
12 |
29 |
(3.3) |
|
Polycythemia |
16 |
6 |
22 |
(2.5) |
|
Metabolic |
7 |
3 |
10 |
(1.2) |
|
Dehydration |
11 |
14 |
25 |
(2.9) |
| Mixed |
17 |
14 |
31 |
(3.6) |
| Unknown |
39 |
28 |
67 |
(7.7) |
The administration of oxytocin during labor was associated with a significantly higher neonatal serum bilirubin (mean serum bilirubin 13.4
± 2.2 vs 12.6
± 2.6 mg/dl, p
versus 23%, X2
=
7.7, P <0.01). Similarly a
significantly higher number of newborns with jaundice of "unknown" etiology had received oxytocin in labor (11 % versus 5%,
X2=7.6, p<0.01).
A Similar association of prostaglandin use during labor was also seen with
higher serum bilirubin levels (mean SBR 13.5±2.0
vs 12.8±2.5
mg/dl, p<0.01). Newborn infants undergoing exchange transfusions were also
lightr 2181±
963 vs 2772±
720 g, p<0.001), of a lower gestational age (34.3±4.1 vs 37.3±2.7 weeks
p<0.001) and had lower Apgar scores at 1 and 5 minutes,
respectively (one minute Apagar score 5.6±2.1 vs 7.0±1.6, p<0.001 and 5 minutes
Apgar score 8.1±1.1 vs 8.6±1.0, p<0.01).
Table II shows the association of various factors with the need for an exchange transfusion within this cohort. Low birth weight, birth asphyxia, hypothermia at admission and a diagnosis of hemolytic jaundice due to Rh, ABO incompatibility and G6PD deficiency were independently associated with significantly increased risk of requiring an exchange transfusion.
TABLE II
Association of Various Factors with the Need for an Exchange Transfusion
|
Factors |
Not
Exchanged
(n=842) |
Exchanged
(n=27) |
Univariate analysis
|
Multivriate
analysis |
|
OR |
(95% CI) |
OR |
(95% CI) |
| Previous History of
neonatal jaundice |
15 |
3 |
6.9 |
(1.5-27.8) |
5.0 |
(0.9-28.7) |
| Maternal oxytocin
use |
372 |
7 |
0.4 |
(0.2-1.1) |
0.6 |
(0.2-1.6) |
| birth asphyxia |
188 |
17 |
5.9 |
(2.5-14.1) |
3.9 |
(1.0-10.2) |
| Low birth weight |
261 |
16 |
3.2 |
(1.4-7.6) |
1.6 |
(0.6-4.2) |
| ABO incompatibility |
52 |
4 |
2.6 |
(0.7-8.5) |
6.0 |
(1.8-22.6) |
| Rh incompatibility |
50 |
7 |
5.5 |
(2.0-14.7) |
9.0 |
(2.8-22.6) |
| G6PD deficiency |
18 |
2 |
3.7 |
(0-17.8) |
14.5 |
(2.7-78.7) |
| Sepsis |
38 |
6 |
6.1 |
(2.1-17) |
3.8 |
(1.2-12.4) |
| Hypothermia |
24 |
5 |
7.8 |
(2.4-24.1) |
10.1 |
(2.9-35.4) |
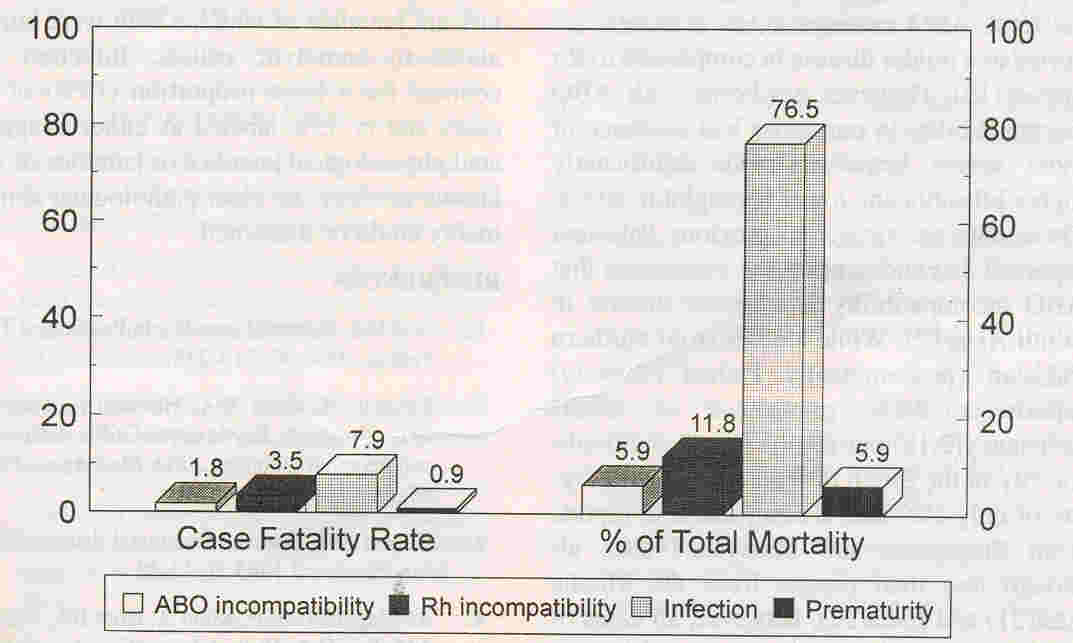
A total of 17 (2%) newborns with significant hyperbilirubinemia died, with infection accounting for 77% of all deaths. Figure 2 illustrates the pattern of neonatal deaths during the study period.
 |
|
Fig. 2.
Neonatal Mortality over the study period (1992-1994) |
Discussion
Our data highlight the importance of prematurity, infection and ABO and Rh incompatibility in newborns with significant jaundice in Karachi and the relative rarity of G6PD deficiency in this birth cohort. In addition birth asphyxia, hypothermia and infection were identified as independent risk factors for severe hyperbilirubinemia requiring ex- change transfusion.
Several limitations should be considered in evaluating our data. The main limitation of this study is that it is retrospective. Secondly because of the paucity of sophisticated laboratory facilities, we could not further analyze the subcategory of miscellaneous hemolyses
to determine specific etiologies. It is also possible that multiple etiologies operated in several newborns, e.g., infection and prematurity whereas we primarily ascribed the dominant etiology in our analysis, i.e., our data was not discrete.
The prevalence of neonatal jaundice requiring therapy (15.6%) is lower than previous reports from Pakistan(l-3) which were mostly based on outpatient admissions. These figures though higher than those cited from birth cohorts from India(8), and elsewhere(9), are comparable to other cohorts studied in
Australia(10), China(ll) and Thailand(12).
Although, infection (19%) was the second most common etiology, it was still less
than a figure of 53% previously reported from Pakistan(l). This is probably because of the selective nature of previously reported case series. While the rate of infection is much lower than
in Africa(13) and comparable to data from the Middle East and India( 4,8), it still remains much higher than developed countries, where sepsis accounts for less than 5% of significant hyperbilirubinemia( 1 0, 14). Infection was also the main cause of death associated with jaundice (77%). This indicates the need for aggressively treating infection associated with jaundice. We have no satisfactory explanation for the absence of cases of congenital hypothyroidism within this birth cohort as all newborn infants had TSH screening after birth.
Hemolytic jaundice accounted for almost 20% of all significant jaundice, with ABO and Rh incompatibility comprising two thirds of the total. ABO incompatibility is usually re- ported as a milder disease in comparison to Rh disease(15). However newborns with ABO incompatibility in our series had evidence of more severe hemolysis with significantly higher bilirubin and lower hemoglobin levels. These data are similar to previous Pakistani reports(1,16) and support the contention that ABO incompatibility is a severe disease in South Asia( 17). While studies from northern Pakistan (predominantly Path an ethnicity) reports a 7-8% prevalence of G6PD . deficiency(2, 18) our results from a multiethnic;
city in the South of Pakistan reveal a figure of only 2%. This is comparable to reports from Singapore, and Malaysia(19,20), al- though less than reports from the Middle East(21) and India(22). However, all cases of G6PD deficiency had evidence of severe hemolysis. Despite this low prevalence, given that G6PD deficiency comprised 12% of all hemolytic jaundice with comparable severity to ABO and Rh incompatibility, we would recommend a qualitative G6PD deficiency test in all Pakistani newborns with suspected hemolysis.
Univariate and logistic regression analysis
showed ABO and Rh isoimmunization, G6PD deficiency, sepsis, hypothermia and
birth asphyxia were independent risk factors for severe jaundice. However, the
95% confidence intervals were wide suggesting caution in interpreting these
data. The contribution of infection to the severity of jaundice suggested
previously(1), is also highlighted by this study. Our identification of birth
asphyxia as a risk factor for severe jaundice is similar to earlier observations(23) and highlights the importance of preventing birth asphyxia, early stabilization and active monitoring
of such infants for jaundice.
In summary, our data from a birth cohort in Karachi reveals a 15.6% prevalence of significant
jaundice of which a fifth were attributable to hemolytic causes. Infection ac- counted for a large proportion (19%) of all cases and in 35% labeled as either exaggerated physiological jaundice or jaundice of unknown etiology, no clear pathological abnormality could be discerned.
|
1.
ArifMA. Neonatal jaundice in Pakistan. J Trop Pediatr 1984; 30: 213-216.
2.
Rehman H, Khan MA, Hameed A, Roghani MT, Ahmad A. Erythrocyte G6PD deficiency and neonatal jaundice. J Pak Med Assoc 1995; 45: 259-260.
3.
Haneef SM. Pattern of neonatal disease. Paki- stan Paediatr J 1985; 9: 42-48.
4.
AI-Magamci MSF, Khan A, Bhat BA, Nadroo AM, Itoo B A. Neonatal jaundice: An etiological survey in the Madinah region. Ann Saudi Med 1996; 16: 221-223.
5.
Kuruvilla KA, Sakumar ST, Jana AK. Glucose-6-phosphate dehydrogenase deficiency in neonatal hyper-bilirubinemia in a south Indian referral hospital. Indian Pediatr 1998; 35: 52- 55.
6.
Fleming PJ, Bhutta ZA. Neonatal Jaundice. In: A Neonatal VAde-Mecum, 2nd edn. Eds.
Fleming PJ, Speidel BD, Marlow N, Dunn PM. 1987; pp 264-266.
7.
Puckett CD. The Educational Annotation of In- ternational Classification of Diseases
-
Ninth Revision Clinical Modification, 4th edn. Reno, Nevada, Channel Publications 1986; p 1209.
8.
Singh M, Deorari AK, Khajuria RC, Paul VK. A four year study on neonatal morbidity in a New Delhi hospital. Indian J Med Res 1991; 94: 186-]92.
9.
Maisels MJ, Gifford K, Antie CE, Lieb GR. Jaundice in the healthy newborn infant: A new approach to an old problem. Pediatrics 1988; 81: 505-511.
10.
Guaran RL, Drew JH, Watkins AM. Jaundice: Clinical practice in 88,000 liveborn infants. Aust NZ J Qbstet Gynecol 1992; 32:
186-192.
11.
Fok TF, Lau SP, Hui CWo Neonatal jaundice: Its prevalence in Chinese babies and associating factors. Aust PaediatrJ 1986; 22: 215-219.
12.
Phuapradit W, Chaturachinda K, Auntlamai S. Risk factors for neonatal hyperbilirubinemia. J Med Assoc Thailand. 1993; 76: 424-428.
13.
Ahmed H, Yukubu AM, Hendrickse RG. Neonatal jaundice in Zaria, Nigeria-A second
prospective study. West Afr J Med. 1995; 14: 15- 23.
14.
Maisels MJ, Kring E. Risk of sepsis in newborns with severe hyperbilirubinemia. Pediatrics 1992; 90: 741-743.
15.
Clarke CA. Scientific basis of clinical practice: Practical effects of blood group incompatibility between mother and fetus. Br Med J 1972; 2: 90-95.
16.
ArifMA. Neonatal jaundice due to Rhesus and AB isoimmunization and frequency of these antigens in Pakistani mothers. J Pak Med Assoc 1982; 2: 165-167.
17.
Lucas GN. Neonatal jaundice due to ABO in- compatibility in Sri Lanka. Indian J Pediatr 1996; 63: 381-384.
18.
Bouma MJ, Goris M, Akhtar T, Khan E, Kita E. Prevalence and clinical presentation of glu- cose-6-phosphate dehydrogenase deficiency in Pakistani Path an and Afghan refugee communities in Pakistan: Implications for the use of primaquine in regional malaria control pro- grams. Trans Royal Soc Trop Med Hyg 1995; 89: 62-64.
19.
Tan KL. Phototherapy for neonatal jaundice in erythrocyte. glucose-6-phosphate dehydrogenase deficient infants. Pediatrics 1977; 59: 1023-1026.
20.
Singh H. Glucose-6-phosphate dehydrogenase deficiency: A preventable cause of mental re- tardation. Br Med J 1986; 295: 297-298.
21.
Yaish HM, Niazi GA, Al Shalaan M, Khan S, Ahmed GS: Increased incidence of hyperbilirubinemia in 'unchallenged' glucose-6-phosphate dehydrogenase deficiency in term Saudi newborns. Ann Trop Paediatr 1991; 11: 259-266.
22.
Singhal PK, Singh M, Paul VK, Deorari AK, Ghorpade MG. Spectrum of neonatal hyperbilirubinemia: An analysis of 454 cases. Indian Pediatr 1992; 29: 319-325.
23.
Drew JH, Barrie J, Horacek I, Kitchen WH. Factors influencing jaundice in immigrant Greek infants. Arch Dis Child 1978; 53: 49-52.
|
