|
|
|
Indian Pediatr 2017;54: 204-207 |
 |
Effect of Recorded
Maternal Voice on Child’s Cooperation During Cardiac
Catheterization –
A randomized controlled trial
|
|
Daliya Rajan, Gopichandran Lakshmanan, *Saurabh Kumar
Gupta, *Ramakrishnan Sivasubramanian, *Anita Saxena, and *Rajnish Juneja
From College of Nursing and *Department of
Cardiology, AIIMS, New Delhi, India.
Correspondence to: Dr Saurabh Kumar Gupta, Department
of Cardiology, Room No. 9, 8th floor, Cardiothoracic Sciences Centre,
All India Institute of Medical Sciences, New Delhi 110 029, India.
[email protected]
Received: February 03, 2016; Initial review:
March 28, 2016; Accepted: January 11, 2017.
Published online: February 02, 2017.
PII:S097475591600037
|
Objective: To assess the effect of recorded
maternal voice on child’s cooperation during cardiac catheterization.
Design: Randomized placebo controlled trial.
Setting: Cardiac catheterization laboratory at a
tertiary care hospital.
Participants: 90 children with congenital heart
disease scheduled for cardiac catheterization between July 2014 and Dec
2014 randomized to maternal voice group and control group.
Intervention: During cardiac catheterization,
children in maternal voice group listened to a 3-min audio-recording of
their mother’s voice, played in loop, using head-phones. Children in the
other group wore headphones without auditory stimuli.
Main outcome measures: Child’s cooperation during
cardiac catheterization as assessed by Child Emotional Manifestation
Scale.
Results: Children in the maternal voice group
showed lower mean (SD) distress scores [13.2 (4.6) vs. 16 (5.6),
P=0.01]. The requirement of sedative agents during the procedure
was not different (P=0.09).
Conclusions: Allowing children to listen to
recorded voice of their mother is an effective strategy to improve
cooperation during cardiac catheterization.
Keywords: Anxiety, Cooperation, Distress, Congenital heart
disease.
|
|
A well performed cardiac catheterization is important for management of
a variety of congenital heart diseases (CHD). The accuracy of
information obtained during cardiac catheterization relies heavily on
achieving a steady hemodynamic state during the procedure and therefore
the child’s cooperation is mandatory. In most of the centers worldwide,
cardiac catheterization is performed under conscious sedation.
Pre-procedure counselling allay anxiety of most of the adolescents and
adults. However, this is not an option in young children. It is not just
fear of the procedure, but many other factors such as intravenous
cannulation and physical restrain to achieve optimal position for
vascular access during catheterization, that makes them anxious. To add
to the woes children are separated from their parents. This anxiety and
discomfort not only risks the validity of cardiac catheterization but
also result in stressful hospital experience. These adverse hospital
experiences are known to result in psychosocial adjustment problems in
children [1,2].
Anxiety can partly be allayed by administration of
intravenous analgesia and anesthesia before the procedure. Child’s
cooperation; however, remains far from desired in the majority. Among
other measures distracting child’s attention away from unpleasant
stimuli is effective in improving cooperation during painful invasive
procedures [3-6]. Although the presence of the parents is arguably most
reassuring to a distressed child, it involves the risk of radiation
exposure to parents. In addition, the potential of interference with
smooth functioning of healthcare professionals cannot be understated.
The use of parental voice eliminates these problems while successfully
distracting the child away from the stressful environment during various
non-invasive procedures [7-10]. This has not been studied in the setting
of cardiac catheterization. We undertook this randomized study to assess
the effect of maternal voice on child’s cooperation during cardiac
catheterization.
Methods
Children aged 2-5 years, scheduled for cardiac
catheterization between July 2014 and December 2014 were enrolled in
this randomized control trial. Children were excluded from the study if
they had significant hearing or learning deficits, or were not
accompanied by their mother. In addition, children who underwent the
procedure under general anesthesia, or were deeply sedated during the
procedure were also excluded from the analysis. The study was approved
by the Institutional ethics committee of our institute, and a written
informed consent was obtained from the parents. After enrolment,
children were randomized to Maternal-voice group arm and Control group
using a computer-generated sequence.
Mothers of children in the intervention group were
interviewed and explained the process of voice-recording one day prior
to the procedure. Mothers were encouraged to record conversation
unrelated to the cardiac catheterization. Maternal voice was recorded
for 3 minutes in their native language talking about pleasurable events
or activities by which the child was most likely to be happy. The
recording was performed in a quiet room using microphone and voice
recorder function incorporated within Samsung Galaxy GT 15510 mobile
smartphone (Seoul, South Korea) in which tele-communication was disabled
temporarily. Both mother and the researcher assessed for the quality of
the voice recorded. The voice recording was accepted when both mother
and the researcher were satisfied of the quality and content of the
recording. The voice recordings were then coded and saved within the
recording device.
As per institutional policy, children scheduled for
cardiac catheterization were fasting for at least four hours before the
procedure. Approximately 10 minutes before the procedure, intravenous
injection Morphine and Midazolam were administered at a dose of 0.1
mg/kg each for analgesia and sedation in the presence of either of the
parents. Thereafter, once children were sleepy they were restrained on a
radiolucent Bakelite board to obtain favorable position for femoral
vascular access and to avoid unwanted movement of the child during
cardiac catheterization. Children were then shifted inside the
catheterization laboratory for cardiac catheterization.
The headphones were placed over ears of children soon
after shifting inside the catheterization laboratory. The headphones
were connected to the same device that was used for recording maternal
voice. As per randomization, maternal voice was played in maternal voice
group while headphones did not emit any sound in control group. The
maternal voice was played in loop for continuous auditory stimulation.
It was ensured that the headphones did not interfere with the
interaction between the operator and the child. Pediatric cardiologist
performing the procedure and nursing staff were not aware of the
randomization.
During the procedure, children were administered
additional doses of intravenous sedation if deemed necessary by the
operator. The dose and frequency of additional doses of sedation were at
the discretion of the operator with no information to the person
handling voice recordings and headphones inside the catheterization
laboratory. The additional doses of intravenous sedation were recorded
by staff nurse.
The child’s cooperation was assessed using Children’s
Emotional Manifestation Scale (CEMS). CEMS is a simple, objective and
consistent clinical tool to assess children’s emotional behavior during
stressful medical procedures [11]. This scale includes five components -
facial expression, vocalization, activity, interaction and level of
cooperation (Web Fig. 1). Each component is
scored from 1- 5 with ‘1’ being the most cooperative behavior and ‘5’
being the least co-operative behavior thus giving a minimum score of 5
and a maximum score of 25 [11]. The pediatric cardiologist performing
the procedure scored CEMS based on child’s behavior in the initial 15
minutes of the procedure after obtaining vascular access.
Statistical analysis: A pilot study of ten
patients showed mean (SD) distress score of 17.1 (6.2) in control group
and 14 (4.3) in the maternal voice group. Considering 5% level of
significance and 80% power, the required sample size was 45 in each
group. Statistical data were analyzed using STATA version 11.1. For all
the statistical tests, P value <0.05 was considered significant.
Results
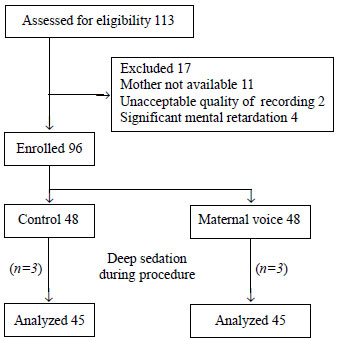
Ninety consecutive children, who were scheduled for
cardiac catheterization were enrolled with 45 children in each group for
analysis (Fig. 1). Various demographic and procedural
characteristics are summarized in Table I. Children in
both the groups were similar in age, sex and educational status of the
mother. Majority of the procedures in both the groups were diagnostic
catheterization.
TABLE I Demographic and Procedure-related Characteristics
|
Maternal |
Control |
|
voice group |
group |
|
(n = 45) |
(n = 45) |
|
School going children, n (%) |
21 (47) |
25 (56) |
|
Literate mother, n (%) |
42 (93) |
42 (93) |
|
Area of residence, n (%) Rural |
24 (53) |
31 (69) |
|
Patient characteristics |
|
|
|
Age (y), mean (SD) |
3.5 (1.05) |
3.9 (1.2) |
|
Male sex |
27 (60) |
35 (78) |
|
Height, mean (SD) |
76.9 (4.8) |
77.9 (4.3) |
|
Weight, mean (SD) |
11 (2.6) |
11.9 (2.4) |
|
Heart rate, mean (SD) |
145 (13) |
141 (12) |
|
Respiratory rate, mean (SD) |
40 (6) |
39 (7) |
|
*Acyanotic CHD, n (%) |
23 (51) |
33 (73) |
|
Procedural characteristics |
|
|
|
Procedure duration (min) mean (SD) |
27.6 (9.9) |
24.8 (9.9) |
|
Pre-procedure fasting time (h) mean (SD) |
4.4 (0.8) |
4.5 (1.2) |
|
Time from injection of local |
|
|
|
anesthesia to puncture for |
|
|
|
vascular access (min) mean (SD) |
3.04 (1.1) |
2.8 (1.1) |
|
*Diagnostic catheterization |
33 (73) |
41 (91) |
|
*P<0.05. |
 |
|
Fig. 1 Study flow chart.
|
Overall CEMS scores and scores for individual sectors
were lower in the maternal voice group as compared to in the control
group (P =0.01) (Table II). The heart rate and
respiratory rate during the procedure in both the groups were
comparable. Forty children in the control group and 34 in maternal voice
group required administration of additional doses of intravenous
sedation during the procedure (P= 0.09).
TABLE II Comparison of Child’s Emotional Manifestation Scale (CEMS) Scores in the two Group
|
Maternal |
Control |
P value |
|
voice group |
group |
|
|
(n=45) |
(n=45) |
|
|
Facial expression |
3 (1.1) |
3.6 (1.4) |
0.02 |
|
Vocalization |
2.7 (1.2) |
3.4 (1.3) |
0.01 |
|
Activity |
2.1 (1.0) |
2.8 (1.2) |
0.01 |
|
Interaction |
2.7 (1.2) |
3.2 (1.2) |
0.01 |
|
Level of cooperation |
2.4 (0.8) |
2.9 (.02) |
0.01 |
|
Total |
13.2 (4.6) |
16 (5.6) |
0.01 |
|
Values in mean (SD). |
Discussion
In this randomized control trial, children who
listened to the maternal voice during the procedure showed improved
cooperation. Overall mean distress scores as well as scores in
individual sector of CEMS were lower in children listening to recorded
maternal voice.
Our findings are consistent with the previous studies
on distraction techniques during other invasive medical procedures
[9-12]. The requirement of additional doses of sedatives did not differ
in two groups. This may be related to more number of therapeutic
catheterizations in the maternal voice group. This is similar to the
study by Kim, et al. [9] and colleagues while studying the effect
of recorded maternal voice on perioperative anxiety in children. In
their study maternal voice resulted in lower anxiety scores but did not
result in reduction in the requirement of injection Ketamine [9].
During therapeutic procedures pediatric
cardiologists tend to use more sedation to minimize unwanted movement of
the child. This, however, is unlikely to affect CMES assessment as it
was based on the child’s behavior during first 15 minutes of the cardiac
catheterization when majority of patients have not received top-up
sedatives. Similar to the findings of Ozcetin, et al. [12]
maternal voice did not change heart rate and respiratory rate of
children in our study.
CEMS is a simple, reproducible and objective tool but
overall evaluation in individual sectors is subjective [11]. The
operators assessing child’s cooperation were blinded to the
randomization and therefore, the CEMS scores are unlikely to reflect
bias. CEMS assessment was performed only once, although the child’s
cooperation varied throughout the procedure.
In conclusion, in this randomized trial involving
children with CHD undergoing cardiac catheterization, use of recorded
maternal voice achieved better cooperation of children than standard
patient care in catheterization laboratory. This practice is expected to
make cardiac catheterization more acceptable to children with CHD in
addition to improving the yield of cardiac catheterization.
|
What is Already Known?
•
Use of distraction techniques
improve child’s cooperation during invasive procedures.
What This Study Adds?
•
Recorded maternal voice improves child’s cooperation during
cardiac catheterization.
|
References
1. LeRoy S, Elixson EM, O’Brien P, Tong E, Turpin S,
Uzark K. Recommendations for Preparing Children and Adolescents for
Invasive Cardiac Procedures: A Statement from the American Heart
Association Pediatric Nursing Subcommittee of the Council on
Cardiovascular Nursing in Collaboration with the Council on
Cardiovascular Diseases of the Young. Circulation. 2003;108:2550-64.
2. Utens EM, Verhulst FC, Meijboom FJ, Duivenvoorden
HJ, Erdman RA, Bos E, et al. Behavioural and emotional problems
in children and adolescents with congenital heart disease. Psychol Med.
1993;23:415-42.
3. Caire JB, Erickson S. Reducing distress in
pediatric patients undergoing cardiac catheterization. Child Health
Care. 1986;14:146-52.
4. Fowler-Kerry S, Lander JR. Management of injection
pain in children. Pain. 1987;30:169-75.
5. Usman LS, Chambers CT, McGrath PJ, Kisely S. A
systematic review of randomized controlled trials examining
psychological interventions for needle-related procedural pain and
distress in children and adolescents: An abbreviated cochrane review. J
Pediatr Psychol. 2008;33:842-54.
6. Birnie KA, Noel M, Parker JA, Chambers CT, Uman
LS, Kisely SR, et al. Systematic review and meta-analysis of
distraction and hypnosis for needle-related pain and distress in
children and adolescents. J Pediatr Psychol. 2014;39:783-808.
7. Gonzalez JC, Routh DK, Armstrong FD. Effects of
maternal distraction versus reassurance on children’s reactions to
injections. J Pediatr Psychol. 1993;18:593-604.
8. Moon EC, Chambers CT, McGrath PJ. "He says, she
says": A comparison of fathers’ and mothers’ verbal behaviour during
child cold pressor pain. J Pain. 2011;12:1174-81.
9. Kim SJ, Oh YJ, Kim KJ, Kwak YL, Na S. The effect
of recorded maternal voice on perioperative anxiety and emergence in
children. Anaesth Intensive Care. 2010; 38:1064-9.
10. Johnston CC, Rennick JE, Filion F, Campbell-Yeo
M, Goulet C, Bell L, et al. Maternal touch and talk for invasive
procedures in infants and toddlers in the paediatric intensive care
unit. J Pediatr Nurs. 2012;27:144-53.
11. Li HC, Lopez V. Children’s Emotional
Manifestation Scale: development and testing. J Clin Nurs.
2005;14:223-9.
12. Ozcetin M, Suren M, Karaaslan E, Colak E, Kaya S,
Guner O. Effects of parent’s presence on pain tolerance in children
during venipuncture: A randomised controlled trial. Hong Kong J Pediatr.
2011;16:247-52.
|
|
|
 |
|

