|
|
|
Indian Pediatr 2017;54: 185 -192 |
 |
Intergenerational Change in Anthropometric
Indices and Their Predictors Among Children in New Delhi Birth
Cohort
|
|
*$ Sikha Sinha,
#Abha Rani
Aggarwal, **Clive Osmond, **Caroline HD Fall,
‡Santosh K
Bhargava and *Harshpal Singh Sachdev
From *Sitaram Bhartia Institute of Science
and Research, $University School of Medicine and Para-medical
Health Sciences, Guru Gobind Singh Indraprastha University, #National
Institute of Medical Statistics, Indian Council of Medical Research, and
‡Sunder Lal Jain Hospital, New Delhi, India; and **MRC
Lifecourse Epidemiology Unit, University of Southampton, Southampton,
UK.
Correspondence to: Prof Harshpal Singh Sachdev,
Senior Consultant Pediatrics and Clinical Epidemiology, Sitaram Bhartia
Institute of Science and Research, B-16 Qutab Institutional Area, New
Delhi 110 016, India.
Email: [email protected]
Received: October 07, 2016;
Initial review: November 03, 2016;
Accepted: November 30, 2016.
Published online: December 05, 2016.
PII:S097475591600033
|
Objective: To evaluate
intergenerational change in anthropometric indices of children and their
predictors.
Design: Prospective cohort.
Participants: New Delhi Birth
Cohort participants (F1), born between 1969 and 1972, were followed-up
for anthropometry at birth and 6-monthly intervals until 21 years. Their
children (F2) below 10 years were evaluated anthropometrically.
Outcome measure:
Intergenerational change (F2-F1) in height, weight and body mass index
(BMI) of children in comparison to their parents at corresponding ages.
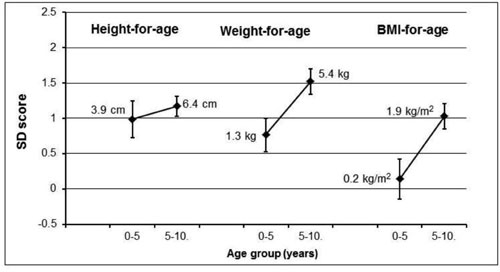
Results: 432 F2-F1 pairs were
analyzed in age-groups of 0-5 (26.9%) and 5-10 (73.1%) years. Children
were considerably taller (0-5 years 0.99 SD; 5-10 years 1.17 SD) and
heavier (0-5 years 0.77 SD; 5-10 years 1.52 SD) while only those aged
5-10 years were broader (had a higher BMI; 1.03 SD), than their parents.
These increases for 0-5 and 5-10 years, respectively corresponded to 3.9
and 6.4 cm for height, 1.3 and 5.4 kg for weight and 0.2 and 1.9 kg/m2
for BMI. Lower parents’ anthropometric indices and poor water supply and
sanitation facilities; higher age of parents at child birth and of
children when measured (for height and weight); and more parental
education (for weight and BMI), were associated with greater
intergenerational gains in children.
Conclusion: Over one generation
in an urban middle-class population, whose general living conditions had
improved, under-five children have become considerably taller and
heavier, and 5-10 year old children have additionally become broader,
than their parents at corresponding ages. Child populations probably
‘grow up’ before ‘growing out’.
Keyword: Anthropometry, Body mass index,
Intergenerational effect, Secular trend.
|
|
T
here is a perception that despite considerable
economic growth, India has not made commensurate progress in addressing
anthropometric (weight-for-age, height-for-age and weight-for-height or
body mass index-for-age) undernutrition [1]. The current national
prevalence of undernutrition in children below five years is still high;
39% are stunted, 29% are underweight and 15% are wasted [2]. However,
this common belief appears somewhat flawed; there has been substantial
improvement in stunting and underweight over the years [3,4]. A
comparison of the two latest national surveys, National Family Health
Survey-3 (2005-06) and Rapid Survey on Children (2013-14), reveals a
decline in stunting (48% to 39%) and underweight (43% to 29%), but only
a marginal reduction in wasting (20% to 15%) [2,5]. Similarly, available
data from 14 states in the recent National Family Health Survey-4
(2015-16) confirms a decline in stunting and underweight. However,
wasting decreased in only six states (by 2% to 15%) and paradoxically
increased in eight states (by 1% to 9%) [6].
National surveys and regional cross-sectional studies
do not provide a robust indication of secular change and its quantum,
especially in those reaping the benefits of development, for example,
the middle socio-economic strata in urban settings. Information of this
nature would provide a reasonable yardstick for improvement goals in
childhood anthropometry, especially if novel nutrition interventions are
being considered. Further, such data would identify the potential burden
of over-nutrition in children born to relatively undernourished parents;
a nutrition transition pattern that could explain the emerging epidemic
of non-communicable diseases (NCDs) in the country [7].
A robust estimate could be obtained through an
intergenerational cohort design. This would offer the advantages of
partially controlling for genetic variations while comparing
anthropometry of children with their parents at similar ages. To the
best of our knowledge, no such data are available in the Indian context
to inform policy. This communication reports the intergenerational
change in anthropometric indices of children below ten years of age and
their predictors in the New Delhi Birth Cohort (NDBC).
Methods
The NDBC was drawn from a population of 119,799
living in 12 km 2 area of
South Delhi during 1969-72 [8,9]; 20,755 married women of reproductive
age were recruited and followed regularly every other month to record
menstrual dates. Information on the socio-demographic profile of the
family were collected during recruitment by a social worker. These
included maternal (F0 generation) schooling, paternal (F0 generation)
occupation, and household socio-economic characteristics (type of
family and house, and water supply and sanitation facilities). Women who
became pregnant were visited every two months initially and on alternate
days from the 37th week of gestation. There were 9169 pregnancies
resulting in 8181 live births of cohort children (F1 generation).
Trained personnel recorded the length and weight of the infants within
72 hours of birth, at the ages of 3, 6, 9 and 12 months (± 7 days) and
every 6 months (± 15 days) until 14-21 years using standardized
techniques [9]. These F1 participants were again followed-up at 26-33,
33-39, 36-42 and 42-46 years for anthropometry and cardio-metabolic risk
factors. Socio-demographic profile recorded during these visits included
education and occupation of the F1participant, occupation of F1 spouse,
type of housing, material possessions, family size, toilet, drinking
water source and supply, and general water source and supply.
Simultaneously, their children (F2 generation) below ten years of age
were invited to attend the clinics for anthropometry. The study was
approved by the respective institutional ethics committees. After
obtaining informed consent from parents (F1) and assent from children
(F2, >6 years of age), the length/height and weight of the F2 generation
were recorded using standardized techniques [10]. Recumbent length in
children below 2 years of age was measured using an infantometer, and
height in children ³2
years of age using a portable stadiometer to the nearest 0.1 cm. Weight
was measured using calibrated digital weighing scales with a sensitivity
of 0.1 kg. Body Mass Index (BMI) was calculated as weight in kilograms
divided by height in meters squared.
Statistical analysis: Data analysis was performed
using SPSS 20.0. The intergenerational change in anthropometry was
computed using two types of standardized scores (Z-scores); the World
Health Organization (WHO) reference and internally within the cohort.
For the former, F2 and F1 generation anthropometry was converted to WHO
length/height-for-age, weight-for-age and BMI-for-age Z-scores at the
date of measurement, using an SPSS macro for age-groups 0-5 years [11]
and 5-19 years [12]. For the internal cohort Z-scores, the longitudinal
height, weight and BMI measurements for the F1 generation were modelled
into growth charts using Cole’s LMS method [13,14]. These charts were
used to compute age- and sex-specific Z-scores for F2 children at the
date of measurement. To compare intergenerational anthropometry at
similar ages, the F1 Z-score was interpolated at the exact age of the F2
measurement, using neighbouring F1 measurements. The interpolation was
acceptable if the F1 observation was within 6 months for ages up to 1
year; within 1 year for ages 1 to 2 years; within 1.5 years for ages 2
to 3 years; and within 2 years thereafter. To estimate the comparison in
absolute units, the interpolated F1 Z-score at the exact date of F2
measurement was back-transformed using the L, M and S values for the
cohort Z-scores [15].
The intergenerational change in size was computed as
F2-F1. This intergenerational model had a 3-level data structure
comprising the F0 generation having one or more F1 children (F1-F1
siblings) and the F1 generation having one or more F2 children (F2-F2
siblings). Thus, a mixed model [16] approach was used to allow for this
structure. There were 13 sibships among the F1 generation. We fitted
models to allow for this third level of variation, but there were too
few sibships to disturb the intergenerational effect size estimates and
their standard errors; so subsequently we ignored this variance
component.
The change was quantified in two age groups: 0-5
years and 5-10 years, adjusting for all combinations of the sex of the
child and parent. This intergenerational change was further adjusted for
socio-demographic characteristics. These included maternal (F0)
schooling, wealth and water supply, sanitation and hygiene (WASH) score
at F1 birth; and education of the F1 parent (cohort subject), wealth and
WASH score at F2 measurement. We used the 1st principal component score
[17] to derive the wealth and WASH scores at F1 birth and F2 measurement
from the individual variables (listed in the footnotes of the relevant
tables). These covariates were used in multivariate models as
standardized units (mean 0), so that uncentered variables do not cause
shifts in computed intergenerational changes.
Results
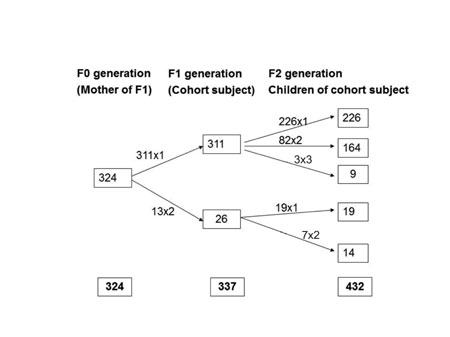
Among the 337 F1 participants there were 13 pairs of
F1-F1 siblings and among the 432 F2 children, 245 were single children,
89 were paired siblings and 3 were three siblings (Fig. 1).
We thus analyzed 432 F2-F1 pairs, which included 178 (41.2%) father-son,
138 (31.9%) father-daughter, 71 (16.4%) mother-son and 45 (10.4%)
mother-daughter comparisons. Among them, 116 (72 boys) were aged 0-5
years and 316 (177 boys) were 5-10 years old, with mean (SD) ages of 3.5
(1.2) and 7.9 (1.3) years, respectively. The mean (SD) height-for-age,
weight-for-age and BMI-for-age (WHO Z-scores) were -0.97 (1.39), -0.68
(1.19) and -0.08 (1.37), respectively for younger children and -0.42
(1.22), -0.31 (1.55) and -0.12 (1.49), respectively for older children.
 |
|
Fig. 1 The three level structure of
the intergenerational data set.
|
The socio-demographic characteristics at the time of
the parent’s (F1 generation) birth and at the time of the child’s (F2
generation) measurement are summarized in Web Table 1.
Comparatively, parents (F1) had a poorer socio-demographic profile;
one-third were residing in a flat or bungalow, the mean (SD) members
sharing a room were 3.6 (1.7), four-fifths had shared toilet facilities,
60% had a common water supply and only one-fourth of their F0 mothers
had completed 10 or more years of education. In contrast, at the time of
the child’s measurement, almost all of them were living in either flat
or independent house, mean (SD) members sharing a room were 1.9 (0.9),
most had separate toilet facilities (96%) and water supply (81%), and
62% of their F1 mothers had 15 or more years of education (graduate).
TABLE I Intergenerational Changes in Anthropometry
|
Anthropometric |
|
|
0-5 years |
|
|
5-10 years |
|
change (F2-F1) |
N |
Mean (95% CI) |
P value |
No. |
Mean (95% CI) |
P value |
|
WHO Z-score |
|
|
|
|
|
|
|
Height for age |
114 |
0.99 (0.73; 1.25) |
<0.001 |
315 |
1.17 (1.03; 1.31) |
<0.001 |
|
Weight for age |
112 |
0.77 (0.53; 1.00) |
<0.001 |
305* |
1.52 (1.34; 1.70) |
<0.001 |
|
BMI for age |
110 |
0.14 (-0.14; 0.42) |
0.310 |
310 |
1.03 (0.85; 1.21) |
<0.001 |
|
Absolute units |
|
|
|
|
|
|
|
Height (cm) |
114 |
3.9 (2.9; 4.9) |
<0.001 |
315 |
6.4 (5.6; 7.2) |
<0.001 |
|
Weight (kg) |
112 |
1.3 (0.8; 1.7) |
<0.001 |
311 |
5.4 (4.7; 6.1) |
<0.001 |
|
BMI (kg/m2) |
110 |
0.2 (-0.2; 0.6) |
0.255 |
310 |
1.9 (1.5; 2.2) |
<0.001 |
Mixed model adjusted for the sex of the children and parents.
* WHO weight-for-age could not be interpolated for 6 parents
because the reference stops at 10 years of age. |
Table I summarizes the intergenerational
change (F2-F1) in anthropometry. Children were significantly (P<0.001)
taller and heavier than their parents at corresponding ages; the
increase was similar (~1 SD) for height in both age groups but was
higher for weight in older children (1.52 vs 0.77 WHO Z-score;
non- overlapping confidence intervals). However, the BMI-for-age
increase (1 SD) was significant (P<0.001) only in the age-group
of 5-10 years. Considering the entire age range (0-10 years), the mean
(95% CI) intergenerational increases (SD) in anthropometric indices
were: Length/Height-for-age: 1.13 (1.01, 1.26), Weight-for-age: 1.32
(1.17, 1.47), and BMI-for-age: 0.79 (0.63, 0.95) (P<0.001 for
all). These average Z-score increases for the 0-5 and 5-10 year
age-groups, respectively corresponded to 3.9 and 6.4 cm for height, 1.3
and 5.4 kg for weight, and 0.2 and 1.9 kg/m 2
for BMI (Fig. 2). The intergenerational change among boys
and girls was comparable. Sensitivity analyses, using internal cohort Z-
scores and narrower window ranges for F1 Z-score interpolation at the
exact age of F2 measurement revealed similar findings (data not shown).
 |
|
Mixed model adjusted for the sex of the
children and parents. Error bars represent 95% confidence
intervals.
Fig. 2 Intergenerational changes in
anthropometric indices (WHO Z-scores).
|
Using the WHO definition [18], in comparison to their
parents, under-five children had a substantially lower prevalence of
stunting (44.7% vs 18.4%; n=114) and underweight (25.9%
vs 12.5%; n=112). However, wasting remained unchanged (4.6%
vs 5.5%; n=109).
TABLE II Predictors of Intergenerational Change in Anthropometric Indices (Multivariate Model)
Predictors(Standardized units)
|
Height for age (n=331)
Effect size (95% CI); |
Weight for age (n=323)
Effect size (95% CI); |
BMI for age (n=325)
Effect size (95% CI); |
|
P value |
P value |
P value |
|
Parent anthropometry‡ |
-0.47 (-0.62,-0.31); <0.001 |
-0.49 (-0.67, -0.32); <0.001 |
-0.65 (-0.82, -0.49); <0.001 |
|
Age of parent at child birth |
0.34 (0.18, 0.51); <0.001 |
0.37 (0.19, 0.56); <0.001 |
0.17 (-0.02. 0.36); 0.080 |
|
Age of child |
0.25 (0.09, 0.40); 0.002 |
0.32 (0.14, 0.50); <0.001 |
0.12 (-0.08, 0.31); 0.246 |
|
At parent birth |
|
Maternal (F0) Schooling |
0.01 (-0.17, 0.18); 0.954 |
-0.02 (-0.22, 0.19); 0.874 |
-0.02 (-0.23, 0.18); 0.816 |
|
Wealth, Housing, paternal (F0) |
0.08 (-0.10, 0.25); 0.393 |
0.15 (-0.07, 0.36); 0.176 |
0.16 (-0.05, 0.37); 0.125 |
|
occupation* |
|
WASH (Sanitation & water supply)# |
-0.17 (-0.32, -0.03); 0.021 |
-0.25 (-0.43, -0.08); 0.004 |
-0.22 (-0.39, -0.04); 0.014 |
|
At child measurement |
|
Education of parent (F1) |
0.11 (-0.07, 0.29); 0.221 |
0.26 (0.05, 0.47); 0.015 |
0.29 (0.08, 0.50); 0.007 |
|
Wealth, Housing, maternal & |
0.08 (-0.11, 0.26); 0.421 |
0.10 (-0.12, 0.32); 0.374 |
0.05 (-0.17, 0.26); 0.672 |
|
paternal (F1) occupation$ |
|
WASH (Sanitation & water supply)^ |
0.00 (-0.14, 0.14); 0.969 |
-0.07 (-0.23, 0.09); 0.375 |
-0.10 (-0.26, 0.06); 0.236 |
|
Mixed model analysis adjusted for the sex of the children and
parents. All other predictors were also inserted simultaneously
in the multivariate model as standardized units. The intraclass
correlation coefficients (ICC) were 0.14 for height-for-age,
0.27 for weight-for-age and 0.20 for BMI-for-age; ‡Parental
measurement and intergenerational change were for the same
anthropometric index (WHO reference); *Wealth score at F1 birth
was generated from type of family, combination of type of
housing and ownership, paternal (F0) occupation, per capita
household annual income and crowding; #WASH score at
F1 birth was generated from type of toilet, water supply and
facilities for sanitation and water supply; $Wealth
score at F2 measurement was generated using maternal and
paternal (F1) occupation, material possession score and
crowding; ^WASH score at F2 measurement was generated
from toilet and water supply (general and drinking water)
facilities. |
Table II depicts the multivariate
associations of intergenerational change. Parents’ (F1) anthropometry
had the most consistent and strongest associations (P <0.001),
with effect sizes ranging from 0.47 to 0.65 SD decrease per SD. Thus
children of shorter, lighter and thinner parents had gained more in
height, weight and BMI, respectively. The age of the parent (F1) at
child birth and the age of the child (F2) at measurement were
significant (P<0.001) positive predictors for F2 height-for-age
and weight-for-age but not for BMI-for-age. Amongst the
socio-demographics characteristics, poorer WASH status at the F1
parents’ birth predicted greater increase in all three F2 indices. In
contrast, higher parental (F1) education predicted greater F2 gain in
weight and BMI, and had no association with F2 height gain. Table
III quantifies the adjusted intergenerational changes across
sub-groups of various predictors.
TABLE III Adjusted Intergenerational Changes Across Different Subgroups of Predictors (Multivariate Model)
|
Predictors |
Length/Height-for-age |
Weight-for-age |
BMI-for-age |
|
n |
Mean change (95% CI) |
P |
n |
Mean change (95% CI) |
P |
n |
Mean change (95% CI) |
P |
|
F2 sex |
|
Male |
191 |
1.19 (1.02, 1.37) |
0.478 |
184 |
1.33 (1.11, 1.54) |
0.916 |
186 |
0.76 (0.55, 0.97) |
0.501 |
|
Female |
140 |
1.05 (0.85, 1.25) |
|
139 |
1.21 (1.00, 1.42) |
|
139 |
0.75 (0.52, 0.98) |
|
|
F1 sex |
|
Male |
248 |
1.13 (0.96, 1.29) |
0.756 |
239 |
1.29 (1.11, 1.48) |
0.637 |
242 |
0.77 (0.60, 0.95) |
0.822 |
|
Female |
83 |
1.18 (0.98, 1.39) |
|
84 |
1.32 (1.02, 1.63) |
|
83 |
0.72 (0.36, 1.09) |
|
|
Parent anthropometry with WHO reference |
|
1st tertile |
110 |
1.57 (1.31, 1.83) |
<0.001 |
110 |
1.62 (1.36, 1.89) |
<0.001 |
113 |
1.45 (1.20, 1.69) |
<0.001 |
|
2nd tertile |
114 |
1.07 (0.84, 1.29) |
|
107 |
1.55 (1.33, 1.78) |
|
99 |
0.58 (0.28, 0.88) |
|
|
3rd tertile |
107 |
0.77 (0.53, 1.01) |
|
106 |
0.77 (0.45, 1.09) |
|
113 |
0.21 (-0.09, 0.52) |
|
|
Age of parent at child birth |
|
1st tertile |
117 |
0.79 (0.54, 1.03) |
<0.001 |
112 |
1.06 (0.75, 1.37) |
<0.001 |
117 |
0.80 (0.54, 1.07) |
0.080 |
|
2nd tertile |
116 |
1.28 (1.09, 1.48) |
|
117 |
1.21 (0.98, 1.45) |
|
116 |
0.53 (0.30, 0.76) |
|
|
3rd tertile |
98 |
1.32 (1.08, 1.56) |
|
94 |
1.58 (1.33, 1.83) |
|
92 |
0.97 (0.64, 1.31) |
|
|
Age of child |
|
|
|
|
|
|
|
|
|
|
0-5 years |
95 |
1.02 (0.74, 1.31) |
0.002 |
94 |
0.78 (0.56, 1.01) |
<0.001 |
92 |
0.20 (-0.10, 0.49) |
0.246 |
|
5-10 years |
236 |
1.16 (1.01, 1.31) |
|
229 |
1.45 (1.25, 1.64) |
|
233 |
0.96 (0.77, 1.14) |
|
|
At parent birth Maternal schooling (F0) |
|
Illiterate |
126 |
1.19 (0.99, 1.39) |
0.954 |
123 |
1.19 (0.95, 1.42) |
0.874 |
124 |
0.51 (0.28, 0.74) |
0.816 |
|
Primary to middle |
123 |
1.09 (0.86, 1.31) |
|
118 |
1.41 (1.14, 1.67) |
|
120 |
0.99 (0.72, 1.26) |
|
|
Matric or above |
82 |
1.06 (0.76, 1.37) |
|
82 |
1.09 (0.76, 1.42) |
|
81 |
0.58 (0.28, 0.88) |
|
|
Wealth, housing, parental (F0) occupation |
|
1st tertile |
110 |
1.11 (0.86, 1.35) |
0.393 |
105 |
1.22 (0.94, 1.50) |
0.176 |
106 |
0.64 (0.34, 0.93) |
0.125 |
|
2nd tertile |
112 |
1.21 (1.00, 1.43) |
|
110 |
1.31 (1.04, 1.57) |
|
111 |
0.74 (0.48, 0.99) |
|
|
3rd tertile |
109 |
1.01 (0.78, 1.25) |
|
108 |
1.20 (0.94, 1.46) |
|
108 |
0.78 (0.55, 1.01) |
|
|
WASH (Sanitation & water supply) |
|
Below median |
174 |
1.28 (1.10, 1.46) |
0.021 |
169 |
1.43 (1.22, 1.64) |
0.004 |
171 |
0.80 (0.58, 1.01) |
0.014 |
|
Above median |
157 |
0.92 (0.73, 1.12) |
|
154 |
1.04 (0.81, 1.26) |
|
154 |
0.59 (0.38, 0.80) |
|
|
At child measurement Education of parent (F1) |
|
Up to High school+ |
153 |
1.07 (0.85, 1.29) |
0.221 |
148 |
1.09 (0.85, 1.32) |
0.015 |
151 |
0.50 (0.26, 0.73) |
0.007 |
|
Graduate or above |
178 |
1.19 (1.03, 1.36) |
|
175 |
1.46 (1.25, 1.67) |
|
174 |
0.95 (0.74, 1.17) |
|
|
Wealth, Housing, maternal & paternal (F1) occupation |
|
1st tertile |
119 |
1.23 (1.01, 1.46) |
0.421 |
115 |
1.13 (0.87, 1.38) |
0.374 |
117 |
0.39 (0.13, 0.65) |
0.672 |
|
2nd tertile |
104 |
0.99 (0.72, 1.27) |
|
101 |
1.39 (1.10, 1.69) |
|
102 |
1.04 (0.73, 1.34) |
|
|
3rd tertile |
108 |
1.13 (0.92, 1.35) |
|
107 |
1.35 (1.09, 1.60) |
|
106 |
0.83 (0.59, 1.07) |
|
|
WASH (Sanitation & water supply) |
|
Below median |
86 |
1.19 (0.93, 1.45) |
0.969 |
84 |
1.43 (1.09, 1.76) |
0.375 |
85 |
0.88 (0.54, 1.22) |
0.236 |
|
Above median |
245 |
1.09 (0.93, 1.24) |
|
239 |
1.20 (1.03, 1.38) |
|
240 |
0.69 (0.51, 0.86) |
|
|
Multivariate mixed model adjusted for sex of the child and
parent, parent anthropometry, age of parent at child birth, age
of child, F0 maternal schooling, F1 parent education, wealth and
WASH score at F1 birth and F2 measurement; All variables were
used in standardized units (centred). P value is estimated from
a continuous scale of covariates as in Table II. |
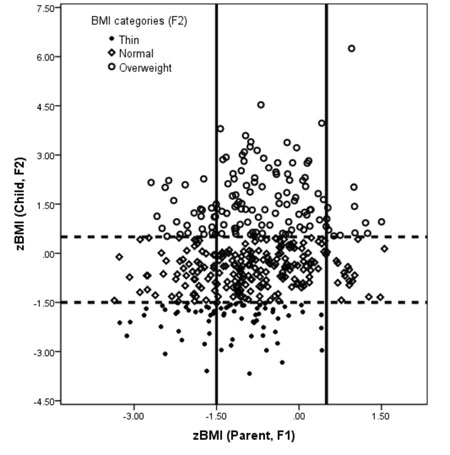
The scatterplot in Fig. 3 illustrates
the transition in BMI categories among parents and children at the same
age. The cut-offs were slightly modified from WHO recommendations [19]
to ensure sufficient numbers in each category: Thin <-1.5 Z, Normal -1.5
to 0.5 Z, and Overweig`ht >0.5 Z. In comparison to 127 children, only 29
parents were overweight at the same age. While a higher proportion of
children of overweight parents were overweight, the greatest increase in
BMI categories occurred in thin parents. A quarter of their children
were overweight while half were normal. In contrast, among all children
born to overweight parents, only 41% were overweight and 59% were
normal.
 |
|
These categories were defined using WHO BMI
Z-score as follows: Thin <–1.5, Normal –1.5 to 0.5, and
Overweight >0.5.
Fig. 3 Scatterplot of transition in Body
Mass Index (WHO Z scores) in parents and their children at
corresponding ages.
|
Discussion
In this intergenerational study, we documented that
children below ten years of age were considerably taller (~1 SD) and
heavier (0.8 to1.5 SD), while only 5-10 years old were broader (~1 SD),
than their parents at corresponding ages. Independent predictors of
greater gains in children included parents with lower anthropometric
indices and poorer WASH facilities; higher age of parents at child birth
and of children at measurement (height and weight); and more parental
education (weight and BMI).
Important limitations of this study include a
somewhat small sample size based on a proportion of the currently
available cohort. Among the parents, there was a considerably higher
representation of fathers because outmigration after marriage was common
in female participants (F1). The main strengths of our study include the
comparison of children and their parents at corresponding ages from
carefully collected prospective data for the latter, an urban LMIC
setting of relatively rapid socio-economic development, and appropriate
multi-level modelling with available confounder adjustment.
These data from an urban middle-class population
provide evidence of substantial increases in the body size of Indian
children over one recent generation. The findings are in broad agreement
with the observed decline in anthropometric under-nutrition from
national surveys [2-6]. Interestingly, the 26% reduction in stunting
over 30 years in this small sample roughly corresponds to the 1% annual
decline documented nationally [2-6]. A scarcity of similar data preclude
emphatic international comparisons. A recent analysis of a century of
trends in adult human height (1896 to 1996 births) concluded that South
Asians (including Indians) were among the shortest and had experienced
little increase (<5 cm) during this era [20]. We could locate only one
directly comparable estimate from Britain, pertaining to a 15 years
earlier period, with similar or better development index status than our
cohort [21,22]. At 7 years, these offspring were only slightly taller
(0.19 SD or 1 cm) and broader (boys: 0.16 SD or 0.23 kg/m 2
and girls: 0.25 SD or 0.46 kg/m2)
than their parents. The substantially larger intergenerational increases
seen in our cohort children will probably translate into commensurate or
greater absolute (cm, kg, kg/m2)
gains in adulthood. These findings should inspire optimism that with
rapid improvements in living conditions, anthropometric gaps from
high-income countries will reduce, particularly because a plateauing
trend for height is evident in some developed nations [20].
In the absence of targeted food or nutrient
supplementation, it is reasonable to ascribe these intergenerational
gains to improvements in general living conditions. However, from a
policy perspective, filtering out important predictors is desirable.
Poorer water supply and sanitation facilities of the parents (F1) at
birth predicted greater F2 gains. A Cochrane systematic review of
cluster randomized trials, intervening for only 9-12 months also
suggests that WASH interventions confer a small benefit on linear growth
(~0.1 SD) in under-five children [23]. The current national impetus on "Swach
Bharat Abhiyaan" is therefore timely and appropriate. In conformity with
earlier experiences [24,25], higher parental literacy was a positive
predictor, thereby re-emphasizing the importance of improving education.
Higher ages of parents at child birth and of children at measurement
were important positive predictors of intergenerational gains in height
and weight. A quadratic relation of childhood anthropometry with age of
child birth has been documented in pooled analyses of cohorts from low-
and middle- income countries (LMICs) [26]; our sample was probably
constituted by the linear component of this association. However, both
these variables are also proxies for exposure duration, thereby
suggesting that sustained improvement in living conditions resulted in
greater benefit.
Poorer parental anthropometry had the strongest and
most consistent predictive ability for greater intergenerational gains.
Potential explanations for this include statistical regression to the
mean, narrowing of socio-economic inequalities and greater biological
response among deprived strata. This observation augurs well for
attempting equity for secular increases in the height of populations.
However, excessive BMI gain in children of thin parents, if primarily
due to increased adiposity, could be providing the backdrop for the
current escalation of cardio-metabolic risk factors in Indian children
and adolescents [7,27,28]. This hypothesis is in concordance with our
earlier observation of increased risk of diabetes mellitus in adults who
were relatively thin as children but continued to become obese relative
to themselves [9].
Under-five children were considerably taller and
heavier but only older subjects were additionally broader than their
parents. This provides more direct evidence of the earlier postulate,
based on cross-sectional comparisons [29], that children "grow up" (get
taller) before "growing out" (get broader). This observation is also
consistent with the increased prevalence of obesity in older children
from India [28] and other countries [29-31]. The underlying mechanisms
for this phenomenon are unclear to us and merit further exploration.
Our data suggest that sustained improvement in
general living conditions leads to considerable increases in height,
weight and BMI within one generation. The current governance focus on
inclusive development is therefore apt, especially if the benefits
percolate preferentially to the underprivileged. Isolated vertical
interventions (for example, nutrient supplementation) should only be
entertained if there is convincing evidence of substantial benefit above
that expected from developmental transition. Findings from the NFHS-4
survey of notable reductions in stunting and underweight with nearly
stagnant or even increased wasting prevalence in some states should not
fuel exaggerated concerns and action to screen for and treat for severe
acute malnutrition; as this phenomenon may occur in a population
undergoing development-related anthropometric transition. Vigilance may
be required to address the potential of greater cardio-metabolic risk in
families showing large intergenerational increases in BMI.
In conclusion, over one generation in an urban
middle-class population, whose general living conditions had improved,
under-five children have become considerably taller and heavier and 5-10
year old children have additionally become broader, than their parents
at corresponding ages. Child populations probably "grow up" before
"growing out".
Contributors: SS, ARA, HPS, CHDF and SKB:
conceptualized the study. SS, ARA, CO and HPS: analyzed the data. SS:
drafted the initial manuscript. All authors contributed to the critical
revision of the article.
Funding: Indian Council of Medical
Research for supporting Ms. Sikha Sinha through the Senior Research
Fellowship Scheme. The original cohort studies were supported by the
National Center for Health Statistics, USA and the Indian Council of
Medical Research, India. Later phases have been supported by Department
of Biotechnology, India; British Heart Foundation, UK; Wellcome Trust,
UK; Medical Research Council; UK; Department for International
Development, UK; and Bill and Melinda Gates Foundation, USA.
Competing interests: None stated.
|
What is Already Known?
•
National surveys suggest a decline in anthropometric
undernutrition but there is no robust quantification of secular
increases in body size of children over a recent generation.
What This Study Adds?
• Children below ten years were
considerably taller and heavier, while only 5-10 year old
children were broader (higher BMI), than their parents at
corresponding ages.
|
References
1. Paul VK, Sachdev HS, Mavalankar D, Ramachandran P,
Sankar MJ, Bhandari N, et al. Reproductive health, and child
health and nutrition in India: meeting the challenge. Lancet.
2011;377:332-49.
2. Ministry of Women and Child Development,
Government of India. Rapid Survey on Children 2013-2014. Available from:
http://wcd.nic.in/issnip/National_Fact%20sheet_
RSOC%20_02-07-2015.pdf. Accessed September 6, 2016.
3. Sachdev HP. Overcoming challenges to accelerating
linear growth in Indian children. Indian Pediatr. 2012;49:271-5.
4. Sachdev HPS, Shah D. Epidemiology of maternal and
fetal malnutrition in South Asia. In: Bhutta ZA, editor. Perinatal and
Newborn Care in South Asia. Oxford: Oxford University Press; 2007.
p.75–105.
5. International Institute for Population Sciences
(IIPS) and Macro International. National Family Health Survey (NFHS-3),
2005-06: India:Vol.I. Mumbai, IIPS. Available from:
http://www.rchiips.org/nfhs/NFHS-3%20Data/VOL-1/Summary%20of%20Findings%20(6868K).pdf.
Accessed September 6, 2016.
6. International Institute for Population Sciences
(IIPS). NFHS 4 Factsheet. Available from:
http://rchiips.org/NFHS/factsheet_NFHS-4.shtm. Accessed September 6,
2016.
7. Sachdev HPS. Exploring agricultural levers for
mitigating the overnutrition burden in India. International Food Policy
Research Institute Discussion Paper 01183, May 2012, pp 1-29. Available
from:
http://www.ifpri.org/publication/exploring-agricultural-levers-mitigating-overnutrition-burden-india.
Accessed September 6, 2016.
8. Richter LM, Victora CG, Hallal PC, Adair LS,
Bhargava SK, Fall CH, et al. Cohort profile: the consortium of
health-orientated research in transitioning societies. Int J Epidemiol.
2012;41:621-6.
9. Bhargava SK, Sachdev HS, Fall CH, Osmond C,
Lakshmy R, Barker DJ, et al. Relation of serial changes in
childhood body-mass index to impaired glucose tolerance in young
adulthood. N Engl J Med. 2004;350:865-75.
10. World Health Organization. Physical
Status: The Use and Interpretation of Anthropometry; Report of a WHO
Expert Committee Technical Report. Geneva: World Health
Organization; 1995.
11. World Health Organization. The WHO Child Growth
Standards. Available from: http://www.who.int/child
growth/standards/en/. Accessed September 6, 2016
12. World Health Organization. WHO Growth Reference
data for 5-19 years. Available from: http://www.who.int/growthref/en/.
Accessed September 6, 2016.
13. Cole TJ. The LMS method for constructing
normalized growth standards. Eur J Clin Nutr. 1990;44:45-60.
14. Pan H, Cole T. LMS chart maker Light version
2.54. A program for calculating age-related reference centiles using the
LMS method. London, UK: 2011.
15. Construction of LMS Parameters for the Centers
for Disease Control and Prevention 2000 Growth Charts. National Health
Statistics Reports. Number 63;2013.
16. Cheng J, Edwards LJ, Maldonado-Molina MM, Komro
KA, Muller KE. Real longitudinal data analysis for real people: building
a good enough mixed model. Stat Med. 2010;29:504-20.
17. Vyas S, Kumaranayake L. Constructing
socio-economic status indices: how to use principal components analysis.
Health Policy Plan. 2006;21:459-68.
18. World Health Organization. Global Database on
Child Growth and Malnutrition. Available from:
http://www.who.int/nutgrowthdb/about/introduction/en/index5. html.
Accessed September 6, 2016.
19. World Health Organization. WHO BMI-for-age
criteria. Available from: http://www.who.int/growthref/who2007_
bmi_for_age/en/. Accessed September 6, 2016.
20. NCD Risk Factor Collaboration (NCD-RisC). A
century of trends in adult human height. Elife. 2016;5:e13410.
21. Li L, Power C. Influences on childhood height:
comparing two generations in the 1958 British birth cohort. Int J
Epidemiol. 2004;33:1320-8.
22. Pinot de Moira A, Power C, Li L. Changing
influences on childhood obesity: a study of 2 generations of the 1958
British birth cohort. Am J Epidemiol. 2010;171:1289-98.
23. Dangour AD, Watson L, Cumming O, Boisson S, Che
Y, Velleman Y, et al. Interventions to improve water quality and
supply, sanitation and hygiene practices, and their effects on the
nutritional status of children. Cochrane Database Syst Rev.
2013;8:CD009382.
24. Galobardes B, McCormack VA, McCarron P, Howe LD,
Lynch J, Lawlor DA, et al. Social inequalities in height:
persisting differences today depend upon height of the parents. PLoS
One. 2012;7:e29118.
25. United Nation Children Fund. UNICEF Conceptual
Framework. Available from:
http://www.unicef.org/nutrition/training/2.5/4.html. Accessed
September 6, 2016.
26. Fall CH, Sachdev HS, Osmond C, Restrepo-Mendez
MC, Victora C, Martorell R, et al. Association between maternal
age at childbirth and child and adult outcomes in the offspring: a
prospective study in five low-income and middle-income countries
(COHORTS collaboration). Lancet Glob Health. 2015;3:e366-77.
27. Garg P, Kaur S, Gupta D, Osmond C, Lakshmy R,
Sinha S, et al. Variability of thinness and its relation to
cardio-metabolic risk factors using four body mass index references in
school-children from Delhi, India. Indian Pediatr. 2013;50:1025-32.
28. Hoque ME, Doi SA, Mannan M, Long K, Niessen LW,
Mamun AA. Prevalence of overweight and obesity among children and
adolescents of the Indian subcontinent: a meta-analysis. Nutr Rev.
2014;72:541-50.
29. Smith SM, Craig LC, Raja AE, McNeill G, Turner
SW. Growing up before growing out: secular trends in height, weight and
obesity in 5-6-year-old children born between 1970 and 2006. Arch Dis
Child. 2013;98:269-73.
30. Moon JS. Secular trends of body sizes in Korean
children and adolescents: from 1965 to 2010. Korean J Pediatr.
2011;54:436-42.
31. Zong XN, Li H. Physical growth of children and
adolescents in China over the past 35 years. Bull World Health Organ.
2014;92:555-64.
|
|
|
 |
|

