|
|
|
Indian Pediatr 2015;52: 241 -242 |
 |
Primary Lung Abscess in Early Infancy
|
|
Prasoon Goyadi, *Srikanth KP , Pankaj C Vaidya and
#Meenu Singh
From Departments of Pediatrics, *Pediatric
Gastroenterology and #Pediatric Pulmonology, PGIMER, Chandigarh, India.
Correspondence to: Dr Meenu Singh, Professor,
Division of Pediatric Pulmonology,
Department of Pediatrics, PGIMER, Chandigarh, India.
Email: [email protected]
Received: September 25, 2014;
Initial review: October 22, 2014;
Accepted: December 24, 2014.
|
|
Background: Lung abscess is rare in early infancy. Case
characteristics: We report two infants with lung abscess, who
presented with short respiratory illness.Intervention: Infants
were managed with broad spectrum antibiotics including Clindamycin.
Needle aspiration was attempted in one case. Message: High index
of suspicion in infants with respiratory distress of prolonged duration
can help in reaching the diagnosis.
Keywords: Infants, Pulmonary abscess,
Staphylococcus.
|
|
Lung abscess is a rare condition and much rarer in
early infancy [1,2]. It is characterised by coagulative necrosis of one
or more areas of lung, with more predilection for right lung.
Post-pneumonic abscess is the common variant; however, in young infants
and neonates, de novo occurrence of abscess is reported more often [1].
Unless the condition is complicated by dissemination, recovery is a rule
with appropriate antibiotics alone [3]. We present two cases of primary
lung abscess in early infancy managed with intravenous antibiotics.
Case Report
Case 1: A-6-week-old infant with uneventful
antenatal history, presented with low grade fever for 1 day, followed by
non-paroxysmal cough that was persisting till the time of admission. On
admission to emergency, child was in respiratory distress with rate of
54/min. Examination revealed deceased air entry on the right
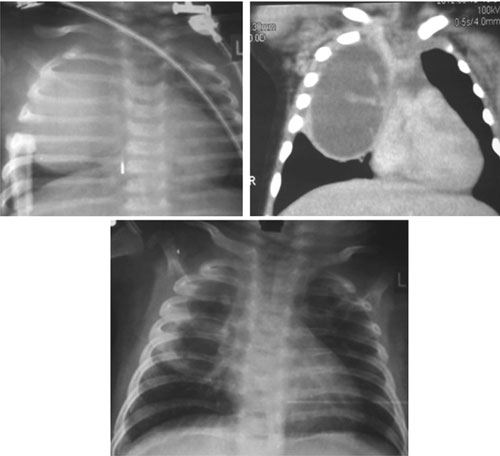
infraclavicular area. Examination of other systems was normal. X-ray
of chest revealed rounded homogenous opacity involving right hemithorax,
silhouetting the right mediastinal margin (Fig. 1a)
with normal costo-phrenic angle. Contrast enhanced computed tomography
(CECT) of the chest (Fig. 1b) revealed a
heterogeneous fluid-filled lesion arising from the right upper lobe,
which was suggestive of a primary lung abscess, infected congenital
cystic adenomatoid malformation, or a germ cell tumour of mediastinum.
Fine needle aspiration cytology was attempted, which did not show any
representative tissue. Total leukocyte count was 16500 with 57%
polymorphs, which substantiated an infectious pathology. Infant improved
after intravenous antibiotics for 3 weeks followed by oral antibiotics.
No organism was isolated from other sterile sites such as blood and CSF,
thus the antibiotics of choice were based on the local epidemiology and
sensitivity pattern. Metabolic parameters were normal, with normal
growth during hospital stay and repeat chest X-ray showed
significant improve after one week (Fig. 1c).
Infant was discharged on oral antibiotics.
 |
|
Fig. 1 Chest radiograph with right
hemithorax opacity sparing costo-phrenic angle (1a), CECT chest
in coronal view showing mass lesion in the right upper
hemithorax suggestive of lung abscess (1b), and chest radiograph
showing clearing of abscess after one week of antibiotics (1c).
|
Case 2: A 10-week-old, previously normal, and
infant was admitted in Pediatric Pulmonology ward with the complaints of
fever, cough and rapid breathing of 10 days duration. Examination
revealed tachypnea, S PO2
of 92%, with subcostal
retractions, nasal flaring and dull note in right mammary and
infraaxillary area with diminished breath sounds in the above mentioned
area. The baby was initially treated as community acquired pneumonia;
however, the chest X-ray revealed a homogenous opacity involving
right upper and middle zone with polymorph nuclear response in hemogram,
thus possibility of lung abscess was considered. In view of early
infancy associated congenital malformation was also considered and CECT
chest was done, which revealed cystic collection in the right hemithorax
suggestive of lung abscess. Blood cultures and CSF analysis were
negative. Patient was started on Cefotaxime, Amikacin, Cloxacillin and
Clindamycin to cover gram positive, gram negative and anaerobic
organisms. Respiratory distress improved remarkably; chest X-ray
repeated after one week revealed clearing of the opacity.
In both the patients, organism could not be isolated.
Work-up for primary and secondary immunodeficiency, and cystic fibrosis
was normal. Total duration of antibiotics was 6 weeks including 3 weeks
each by intravenous and oral route.
Discussion
Primary lung abscesses are rare in early infancy;
however, cases have previously been reported showing that the clinical
course is somewhat different from the older children [1,3,4]. The right
lobe is more commonly affected [4] and associated lung malformations are
reported in nearly half of the patients [5]. The most likely
pathogenesis of primary lung abscess involves an area of initial
pneumonitis leading to necrosis, cavitation and abscess formation [9].
Factors such as prior viral infections like measles, empyema,
under-nutrition and developmental delay [9] were implicated in the
predisposition, though our cases were previously well without any major
risk factors. Presentation varies from typical pneumonic symptoms to
atypical, smouldering course, which can be easily overlooked.
Implicated organisms are Staphycoccus aureus, beta
hemolytic streptococci, Hemophilus influenza and Streptococci pneumoniae,
which can be found alone or in combination [3]. The organism profile is
different in secondary lung abscess where anaerobes are more common. In
a study from China, multitude of organisms was isolated including
Aspergillus and Pseudomonas species [6]. In majority of the
instances the organism profile is comparable to the abscesses at other
site like brain and abdomen [7]. Before the advent of antibiotics,
surgical drainage was the mode of therapy [1]. Microbial therapy is the
cornerstone for the lung abscess and it should be based on the local
epidemiology and culture and sensitivity pattern [5,6]. The reported
duration of therapy varied from 5 days to 3 weeks of parenteral followed
by 4-8 weeks of oral therapy; neonates may require total course through
parenteral mode only [2]. Therapeutic interventions like bronchoscopy,
trans-tracheal drainage, aspiration, and lobectomy are done only when
medical therapy fails, which may also yield the causative agent [3,5].
Before any intervention, these abscesses should be differentiated from
staphylococcal pneumatoceles as management differs [5]. The role of
repeat imaging for documenting the resolution of infection is debatable
and no specific guidelines are set, consensus is to repeat after the
completion of total course of antibiotics [2]. Mortality is less than 5%
in children [8].
To summarize, in two cases of lung abscess discussed
here without any underlying predisposing factors, the most likely
pathogenesis would be post-pneumonia. Lung abscess should be considered
as a differential diagnosis in all infants presenting with clinical
features suggestive of severe community-acquired pneumonia in which
chest radiograph reveals focal or diffuse homogenous opacity.
Contributors: All authors have contributed in
managing the case, reviewing the article and preparation of the
manuscript.
Funding: None; Competing interests: None
stated.
References
1. Moore TC, Battersby JS. Pulmonary abscess in
infancy and childhood: Report of 18 cases. Ann Surg. 1960;151:496-500.
2. Patradoon-Ho P, Fitzgerald DA. Lung abscess in
children. Paediatr Respir Rev. 2007;8:77-84.
3. Bruckheimer E, Dolberg S, Shlesinger Y, Bar Ziv Y,
Branski D, Kerem E. Primary lung abscess in infancy. Pediatr Pulmonol.
1995;19:188-91.
4. Emanuel B, Shulman ST. Lung abscess in infants and
children. Clin Pediatr (Phila). 1995;34:2-6.
5. Jane DS, George HM. Neonatal lung abscess: A
report of six cases. Am J Dis Child. 1979;133:947-9.
6. Chan PC, Huang LM, Wu PS, Chang PY, Yang TT, Lu
CY, et al. Clinical management and outcome of childhood lung
abscess: a 16-year experience. J Microbiol Immunol Infect.
2005;38:183-8.
7. Mehnaz A, Syed AU, Saleem AS, Khalid CN. Clinical
features and outcome of cerebral abscess in congenital heart disease.
JAMC. 2006;18:21-4.
8. Yen CC, Tang RB, Chen SJ, Chin TW. Pediatric lung
abscess: a retrospective review of 23 cases. J Microbiol Immunol Infect.
2004;37:45-9.
9. Brook I, Finegold SM. Bacteriology and therapy of lung abscess in
children. J Pediatr. 1979;94:10-2.
|
|
|
 |
|

