|
|
|
Indian Pediatr 2015;52: 212 -216 |
 |
Diagnostic Accuracy of Indian Scale for
Assessment of Autism (ISAA) in
Children Aged 2-9 Years
|
|
Sharmila Banerjee Mukherjee, Manoj Kumar Malhotra,
Satinder Aneja,
*Satabdi Chakraborty and #Smita
Deshpande
From Department of Pediatrics, LHMC and Associated
Hospitals, New Delhi; *Department of Psychiatry, Pt. BD Sharma PGIMS,
Rohtak, Haryana; and #Department of Psychiatry, PGIMER – Dr. Ram Manohar
Lohia Hospital, New Delhi, India.
Correspondence to: Dr Sharmila B Mukherjee,
Department of Pediatrics, Kalawati Saran Children’s Hospital, Bangla
Sahib Road, New Delhi 110 001, India.
Email: [email protected]
Received: July 07, 2014;
Initial review: September 01, 2014;
Accepted: January 09, 2015.
|
Objective: To determine the diagnostic
accuracy of Indian Scale for Assessment of Autism (ISAA) in children
aged 2-9 year at high risk of autism, and to ascertain the level of
agreement with Childhood Autism Rating Scale (CARS).
Design: Diagnostic Accuracy study
Setting: Tertiary-level hospital.
Participants: Children aged
between 2 and 9 year and considered to be at a high risk for autism
(delayed development, and age-inappropriate cognition, speech, social
interaction, behavior or play) were recruited. Those with diagnosed
Hearing impairment, Cerebral palsy, Attention deficit hyperactivity
disorder or Pervasive developmental disorders (PDD) were excluded.
Methods: Eligible children
underwent a comprehensive assessment by an expert. The study group
comprising of PDD, Global developmental delay (GDD) or Intellectual
disability was administered ISAA by an investigator after one week. Both
evaluators were blinded. ISAA results were compared to the Expert’s
diagnosis and CARS scores.
Results: Out of 102 eligible
children, 90 formed the study group (63 males, mean age 4.5y). ISAA had
a sensitivity 93.3, specificity of 97.4, positive and negative
likelihood ratios 85.7 and 98.7 and positive and negative predictive
values of 35.5 and 0.08, respectively. Reliability was good and validity
sub-optimal (r low, in 4/6 domains). The optimal threshold point
demarcating Autism from ‘No autism’ according to Receiver Operating
Characteristic curve was ISAA score of 70. Level of agreement with CARS
measured by Kappa coefficient was low (0.14).
Conclusions: The role of ISAA in
3-9 year old children at high risk for Autism is limited to identifying
and certifying Autism at ISAA score of 70. It requires re-examination in
2-3 year olds.
Keywords: Autism spectrum disorder,
Certification, Diagnosis, Pervasive Developmental disorders.
|
|
Autism spectrum disorder (ASD) is the most recent
nomenclature for developmental disorders characterized by persistently
impaired social interaction and communication, with stereotypic behavior
[1]. These have previously been also referred to as Pervasive
developmental disorders (PDD) or Autism [2]. Western literature reports
the prevalence of PDD in children as 0.67-1.2% [3,4]. According to a
multicentric Indian community study, it is 0.8 - 1.3% in 2- to
9-year-old children [5]. Early identification of Autism is invaluable as
timely intervention is known to improve outcomes [6]. Current standard
protocols of evaluation recommend satisfying diagnostic criteria of
International Classification of Diseases (ICD) or Diagnostic and
Statistical Manual of Mental Disorders (DSM), followed by qualitative
assessment with internationally validated instruments [1,2,7,8]. These
include Autism Diagnostic Observation Schedule-Generalized (ADOS-G),
Autism Diagnostic Interview-Revised (ADI-R), and Childhood Autism Rating
Scale (CARS) [9-11]. Following this protocol is challenging in India as
differences between Eastern and Western expectations of behavior
influence parental appreciation of symptoms, leading to cultural bias
and affecting instrument psychometric properties [12]. CARS, which also
rates severity, is the only tool validated in the Indian population
[13]. ADOS-G and ADI-R use is additionally limited by cost, and
mandatory international accreditation.
An ideal Indian diagnostic tool for Autism requires
accounting for variable literacy levels and heterogeneous culture and
languages. It needs to be inexpensive, accurate, valid, reliable and
easy to administer. It should also be able to fulfill multiple purposes;
clinical (diagnosis, grading severity, planning intervention and
monitoring), research and certification. The Indian Scale for Assessment
of Autism (ISAA) was jointly developed by the National Trust, Ministry
of Health and Family Welfare, and Ministry of Social Justice and
Empowerment of the Government of India [14]. Its envisioned purpose was
to establish diagnosis, and to rate severity (that was converted to
extent of disability), so that it enabled certification and availing of
benefits from ‘Welfare of Persons with Autism, Cerebral Palsy, Mental
Retardation and Multiple Disabilities Act’ [15].
ISAA was validated in a multi-centric study involving
1124 participants aged 3-22 year with already diagnosed PDD,
Intellectual Disability (ID), other disabilities, and normal intellect,
who belonged predominantly to higher socio-economic strata with higher
literacy levels [16]. Since manifestations are affected by effect of
intervention, developmental age and chronological age, its ability to
diagnose children, especially younger ones was questioned due to their
underrepresentation. The present study was done to determine the
diagnostic accuracy of ISAA in children aged 2-9 year, and measure the
level of agreement with CARS.
Methods
This hospital-based study was conducted in the
Pediatric Developmental Centre of a Medical College in Northern India
from December 2011 to March 2013, after obtaining institutional Ethical
Committee approval. Children between 2-9 years considered to be at high
risk for Autism were consecutively recruited. These included children
with parental concern regarding any one or more of the following:
developmental delay, age-inappropriate cognition, speech delay and
inappropriate social interaction, behavior or play. The sample size
calculated was 85, assuming sensitivity, specificity and power of 80%
each, alpha error 0.05, precision ±10% at 95% confidence interval and
attrition 10% (software-N Master 2.0, CMC Vellore). Those without
accompanying primary care giver, isolated hearing impairment, Cerebral
palsy, or already diagnosed PDD or Attention Deficit Hyperactivity
Disorder (ADHD) were excluded. Informed consent was obtained from all
eligible children.
After evaluation by Brainstem Evoked Response
Audiometry, the evaluation for autism was scheduled on two days, one
week apart. Comprehensive assessment (reference standard) was done on
the first day by a Pediatric consultant (with
³8 years experience
in developmental pediatrics). This comprised of a parental interview
with observation and examination of the child. Developmental Profile
(DP-II) was administered to estimate Developmental quotient (DQ) and
derived Intelligence quotient (IQ), and Vineland Adaptive Behavior Scale
(VABS II) for adaptive function and maladaptive behavior indices
[17,18]. DSM IV diagnostic criteria for PDD were applied, and CARS (DSM
III-based) for assessing severity (total scores of <30, 30-37 and >37
indicate No autism, Mild to moderate autism and Severe autism,
respectively) [2,11]. The study population was consecutively selected
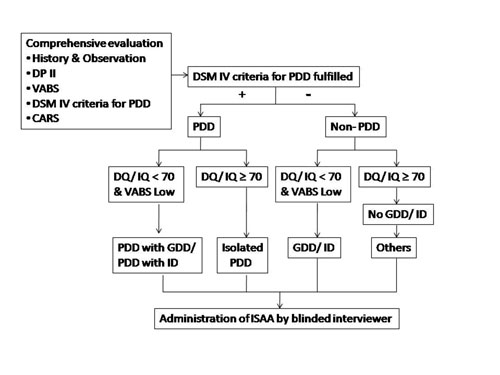
based on a standard diagnostic algorithm (Fig. 1).
Children were categorized as (i) Global Developmental Delay
(GDD)- younger than 5 years with DQ <70, not fulfilling DSM IV criteria
for PDD (ii) Intellectual Disability (ID) with IQ <70 and Low
adaptive levels (³2
SD of norms), not fulfilling DSM IV criteria for PDD (iii) PDD –
fulfilling DSM IV criteria for PDD with or without GDD/ ID and (iv)
Others- other diagnoses.
 |
|
Fig. 1 Algorithm depicting evaluation
and characterization of study subjects.
|
On the next visit, ISAA (test instrument) was
administered by a trained pediatric resident. Test-retest (within 3
months) and inter-rater reliability (by an ISAA expert) was determined
in 10% and 33.3% patients, respectively. ISAA comprises of 40 items
covering 6 domains; Social relationship and reciprocity, Emotional
responsiveness, Speech-language and communication, Behavior patterns,
Sensory aspects and Cognitive. Individual items are scored on a Likert
scale based on history and interviewer observation. Autism is diagnosed
when the total score is ³170.
Severity is categorized as mild, moderate and severe Autism based on
scores of 70-108, 109-153 and >153, respectively. Both evaluators were
blinded to the results of the other’s evaluation. Counseling and further
management was done based on the expert’s diagnosis.
Statistical analysis: SPSS software (version
19.0) was used. Sensitivity, specificity, positive and negative
predictive values, positive and negative likelihood ratio, validity, and
reliability were measured. Kappa coefficient and Receiver Operator
Characteristic (ROC) were determined for level of agreement.
Results
The primary presenting symptoms of the 102 recruited
children were age-inappropriate behavior (64.4%), developmental or
cognitive delay (60% and 48.9%), speech delay (40%), age-inappropriate
play (32.2%) and age-inappropriate social interaction (25.5%). Five
refused participation and 7 were excluded (4 cerebral palsy, 2 neuro-degenerative
disorders and 1 hearing impairment). The study group comprised of 90
children (63 males) with mean age 4.5 years. Age-wise distribution was
2-3 years (26.7%), 3-5 years (28.9 %) and 5-9 years (44.4%). Most were
from the Middle/Lower Middle Socio-economic strata with parental
literacy till higher secondary level [19]. Expert diagnoses were PDD
(77, 85.5%), isolated GDD (3, 3.3%), isolated ID (5, 5.5%), and others
that included 1 Dravet syndrome, 2 ADHD and 2 Behavior problems (5,
5.8%). CARS scores indicated No autism in 12 (13.3%), Mild to moderate
autism in 16 (17.7%) and Severe autism in 62 (68.8%). Co-morbid GDD/ID
were observed in 87% of the children with PDD; moderate cognitive
impairment (DQ/IQ 35-50) more in children with Mild to moderate autism,
and severe cognitive impairment (DQ/IQ 20-35) more in severe autism.
ISAA administration: The average administration
time was 17.4 minutes. During administration, it became apparent that
the content of a few items were unsuitable for the younger children. On
assessment of construct validity it was noted that Pearson correlation
coefficient (r) was acceptable (0.8-0.89) in only Social and
Emotional domains with sub-optimal values ( £0.5)
in the other four. Test-retest and inter-rater reliability was 0.93-0.99
and 0.99, respectively. ISAA scores
³70 (diagnostic of autism) was seen in 76 (84.4%)
children, with rating of severity 53.9% mild, 46 % moderate, and none
with severe Autism. Psychometric parameters are presented in Table
I. Level of agreement of ISAA with CARS was low (Kappa coefficient
0.14, minimal acceptable value ³0.4);
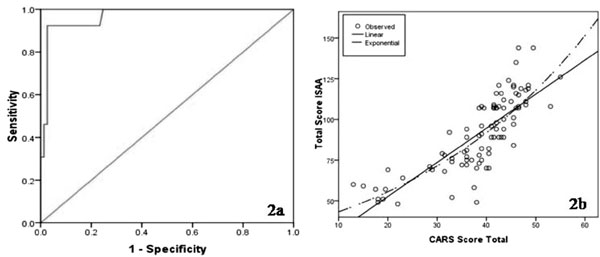
however, the ROC curve (Fig. 2a) showed the
best cut-off point at a score of 70 with 0.92 sensitivity and 0.97
specificity. The scatter diagram plotted between ISAA and CARS total
scores showed maximal clustering around ISAA scores of 70-80 (Fig.
2b).
Table 1 Psychometric Properties of Indian Scale for Assessment of Autism (ISSA)
|
Age group |
Number |
Sensitivity |
Specificity |
PPV |
NPV |
PLR |
NLR |
|
2-9 years |
90 |
92.3 |
97.4 |
85.7 |
98.7 |
35.5 |
0.08 |
|
2-3 years |
24 |
100 |
92.3 |
100 |
100 |
12.9 |
0 |
|
3-9 years |
66 |
90 |
96.4 |
81.8 |
98.2 |
25.0 |
0.11 |
|
Key: NLR- Negative Likelihood Ratio, NPV-Negative Predictive
Value, PLR-Positive Likelihood ratio, PPV- Positive Predictive
Value. |
 |
|
Fig. 2 (a) ROC-curve of Indian Scale
for Assessment of Autism (ISAA) in children aged 2-9 years; (b)
Correlation between total scores obtained on ISAA and Childhood
Autism Rating Scale (CARS).
|
Discussion
This hospital-based study was conducted to determine
the diagnostic accuracy of ISAA in 2-9 year old children presenting with
features considered to be at ‘high risk’ for autism, and to ascertain
its level of agreement in rating severity with CARS. The present study
differed from the original validation study by multiple aspects: younger
participant age (study objective), smaller sample size (albeit
statistically adequate), lower socio-economic and literacy levels
(hospital patient profile), undisclosed diagnosis (eliminating
respondent bias), administration by a pediatrician, and use of
comprehensive assessment as the reference standard instead of only CARS.
This approach is considered superior to the use of a single tool, as it
qualitatively and holistically assesses the multiple facets of ASD [7].
A major limitation realized post-hoc was failure to incorporate
age-stratification and purposive sampling during patient selection. This
resulted in skewed participant profile; lesser 2-3 year olds and
children with isolated GDD/ ID.
Most children (87%) with Autism were low functioning
(co-existent GDD/ID), which is higher than international data (40-80%)
but close to a previous Indian study (90%) [20]. Reasons for this may be
explained by the aforementioned drawbacks of using International
psychometric tools in Indian children, i.e. cultural bias and
non-validation. The use of tools designed for children with GDD/ID to
assess DQ/IQ results in variable data when applied in ASD, scoring is
based on the ability to perform, without considering unwillingness
(frequently seen in autism). Adaptive function is a better reflector of
ability as it considers frequency and quality of performance [21].
Evaluation of diagnostic accuracy of a tool entails critical examination
of validity (the extent to which a test measures what it is supposed to
measure), accuracy (psychometric properties) and reliability (the degree
to which a test consistently measures whatever it measures) [22,23].
Some items demonstrated over-lapping content, ambiguous phrasing (i.e.
‘unable to grasp pragmatics of communication’), and scoring of features
considered developmentally normal in young children as deviant (i.e.
‘unable to maintain peer relationships’, ‘inconsistent attention and
concentration’). Manifestations of ASD are age-dependent; positive
symptoms (overt behaviors) are easily identified irrespective of age,
and negative symptoms (absence of pro-social symptoms) more often missed
in younger children due to non-recognition. Both require inclusion when
a single tool is used for a wide age range. The sub-optimal construct
validity of ISAA may be due to these shortcomings.
The original sensitivity and specificity of ISAA was
reported as 94.3 and 92, respectively [16]. In this study accuracy of
ISAA was found acceptable, albeit specificity was marginally lower.
Although figuratively acceptable, these parameters need to be
interpreted with caution in 2-3 year olds due to aforementioned item
unsuitability and smaller sample size. ROC curves are used to assess
inherent validity. An area-under-the-curve (AUC) value approaching 1
indicates superior performance. Despite the aforementioned fallacies,
the optimal threshold (point of maximum correct classification) was
still 70 (the point that demarcated ‘No autism’ from ‘autism’ in the
validation study). This implies that this ability remains consistent
even in 2-9 year olds. Further categorization of severity was found
unsatisfactory, evident by poor agreement with CARS and absence of
clustering around ISAA scores of >153, which had been expected since
most children had severe autism. The accuracy of ISAA is comparable to
the INCLEN Diagnostic Tool for ASD (INDT-ASD), another validated Indian
instrument designed to identify ASD without grading severity or
disability [24]. Whether INDT-ASD also displays similar drawbacks when
used in pre-school children is uncertain as an age-wise data comparison
is unavailable [24,25].
To conclude, despite its many advantages (indigenous,
free, availability in regional languages and requiring minimal training)
and acceptable psychometric properties, the role of ISAA in 3-9 year old
children is limited to only identifying autism and certifying disability
of at least 40%. This requires further examination in 2-3 year olds. It
may not be possible to use ISAA for assessing severity.
Contributors: SBM, SA: conceived the concept of
the study, and were the neuro-developmental experts of the study; they
will stand as guarantors; SBM: designed the study, and acquired clinical
data related to comprehensive assessment of study subjects; MKM:
collected ISAA related data of study subjects; SD, SC: trained MKM in
administration of ISAA; SC: also helped in collection of ISAA related
data; SBM, MKM: did the literature search and drafted the manuscript
with important inputs from SA, SD and SC. All authors approved the final
manuscript.
Funding: None; Competing Interest: None
stated.
|
What Is Already Known?
•
ISAA is reported to be an
accurate, valid and reliable Indian tool for diagnosing Autism
and grading severity and disability among persons aged 3-22
year.
What This Study Adds?
•
ISAA is psychometrically acceptable and reliable but has
sub-optimal validity in 3-9 year-old children.
•
ISAA can identify autism at a cut-off score of
³70
and thus certify disability of
³40%
in 3-9 year-old children.
|
References
1. American Psychiatric Association. Autistic
Spectrum Disorders. In: Diagnostic and Statistical Manual of
Mental disorders. 5th ed. Arlington VA: American Psychiatric
Association; 2013.p.50-9.
2. American Psychiatric Association. Autistic
Disorder. In: Diagnostic and Statistical Manual of Mental
Disorders. 4rth ed. Washington DC: American Psychiatric Association;
1994.p.70-5.
3. Centers for Disease Control. Prevalence of autism
spectrum disorders-autism and developmental disabilities monitoring
network, 14 sites, United States, 2008. Morbid Mortal Wkly Rep.
2007;56:1-28.
4. Raviola G, Gosselin GJ, Walter HJ, DeMaso DR.
Pervasive Developmental Disorders and Childhood Psychosis. In:
Kliegman RM, Stanton BF, St. Gene III JW, Schor NF, Behrman RE, editors.
Nelson Textbook of Pediatrics. 19th ed. Philadelphia: Saunders,
Elsevier; 2012.p.100-7.
5. Deshmukh VB, Mohapatra A, Gulati S, Nair M,
Bhutani VK, Silberberg DH, et al. Prevalence of neuro-developmental
disorders in India. Proceedings of International Meeting for Autism
Research; 2013 May 4; Kursaal Centre, Donostia, San Sebastián, Spain.
Available from: https//imfar.confex/imfar/2013/webprogram.
Accessed April 5, 2014.
6. Chawarska K, Volkmar FR. Autism in Infancy and
Early Childhood. In: Volkmar FR, Paul R, Klin A, Cohen D,
editors. Handbook of Autism and Pervasive Developmental Disorders. 3rd
ed. New Jersey: John Wiley and Sons, Inc; 2005.p.223-46.
7. Klin A, Saulnier C, Tsatanis K, Volknar FR.
Clinical Evaluation in Autism Spectrum Disorders: Psychological
Assessment with a Transdisciplinary Framework. In: Volkmar FR,
Paul R, Klin A, Cohen D, editors. Handbook of Autism and Pervasive
Developmental Disorders. 3rd ed. New Jersey: John Wiley and Sons, Inc;
2005.p.772-98.
8. World Health Organization. The International
Classification of Diseases 10. Classification of Mental and Behavioral
Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva:
World Health Organization;1992.
9. Lord C, Risi S, Cook EH, Dilavore PC. The Autism
Diagnostic Observation Schedule-Generic: a standard measure of social
and communication deficits associated with the spectrum of autism. J
Autism Dev Dis. 2000;24:659-85.
10. Lord C, Rutter M, LeCouteur A. The Autism
Diagnostic Interview-Revised: a revised version of a diagnostic
interview for caregivers of individuals with possible pervasive
developmental disorders. J Autism Dev Dis. 1994;24:659-85.
11. Schopler E, Reichler RJ, Renner BR. The Childhood
Autism Rating Scale (CARS). Los Angeles: Western Psychological Services,
Inc;1988.
12. Freeth M, Sheppard E, Ramachandran R, Milne E. A
cross-cultural comparison of autistic traits in the UK, India and
Malaysia. J Autism Dev Disord. 2013;43:2569-83.
13. Russell PSS, Daniel A, Russell S, Mammen P, Abel
JS, Raj LE, et al. Diagnostic accuracy, reliability and validity
of Childhood Autism Rating Scale in India. World J Pediatr 2010;6:141-7.
14. Ministry of Social Justice and Empowerment.
Scientific Report on Research Project for Development of Indian Scale
for Assessment of Autism. New Delhi: Government of India; 2009.
15. Ministry of Social Justice and Empowerment. The
National Trust for Welfare of Persons with Autism, Cerebral Palsy,
Mental Retardation and Multiple Disability, The National Trust
Regulations, 2001. Available from: www.social
justice.nic.in/ntregu2001.php. Accessed June 23, 2014.
16. National Trust Web based Intervention Resource
Centre. Indian Scale for Assessment of Autism. Available from:
www.nationaltrust.co.in. Accessed May 6, 2012.
17. Alpern GD, Boll TJ, Shearer M. Developmental
Profile II. Los Angeles: Western Psychological Services; 1989.
18. Sparrow SS, Balla DA, Cicchetti DV. Vineland
Adaptive Behavior Scales. Circles Pines: AGS Publishing; 2005.
19. Kumar R, Dudala SR, Rao AR. Kuppuswamy’s
socio-economic status scale- a revision of economic parameter for 2012.
IJRDH 2013;1:2-4.
20. Juneja M, Mukherjee SB, Sharma S. A descriptive
hospital based study of children with autism. Indian Pediatr.
2005;42:453-8.
21. Sugar M, Konstantareas M, Rampton G. The adaptive
profiles of individuals with Autism spectrum disorders. J Dev Dis.
2010;16:72-6.
22. Greenhalgh T. How to read a paper: papers that
report diagnostic or screening tests. BMJ. 1997;315:540-3.
23. STARD Steering Committee. Standards for the
Reporting of Diagnostic Accuracy Studies Statement. Available from:
www.stard-statement.org. Accessed August 3, 2012.
24. Juneja M, Mishra D, Russell P, Gulati S, Deshmukh
V, Tudu P, et al. INCLEN diagnostic tool for Autism Spectrum
Disorder (INDT-ASD): Development and validation. Indian Pediatr.
2014;51:359-65.
25. Wong CM, Singhal S. INDT-ASD: An autism diagnosis tool for Indian
children. Indian Pediatr. 2014;51:355-6.
|
|
|
 |
|

