|
|
|
Indian Pediatr 2009;46: 219-224 |
 |
Retinopathy of Prematurity in a Tertiary Care
Center – Incidence, Risk Factors and Outcome |
|
Sudha Chaudhari, Vidyadhar Patwardhan, Umesh Vaidya,
Sandeep Kadam and Aarti Kamat
From the Division of Neonatology, Department of
Pediatrics, KEM Hospital, Pune 411 011, India.
Correspondence to: Dr Sudha Chaudhari, Department of
Pediatrics, KEM Hospital, Pune 411 011, India.
E-mail: [email protected]
Manuscript received: April 23, 2007;
Initial review completed: May 12, 2008;
Revision accepted: July 2, 2008. |
|
Abstract
Objective: To study the incidence and risk
factors predisposing to retinopathy of prematurity (ROP) and to assess
the outcome after laser photocoagulation.
Design: Prospective cohort observational study.
Setting: Infants admitted to a neonatal intensive
care unit of a referral hospital between 2000-2006 and followed up till
the age of 3 years.
Methods: Preterm infants with birthweight < 1500g
and gestation £ 32 weeks were
screened for ROP at 4 weeks after birth or 31-33 post conceptional age,
whichever was later. Infants with birthweight
³ 1500g and gestation
> 32 weeks were screened only if
they had additional risk factors. Those found to have threshold disease
ROP had laser photocoagulation. They were recalled at 3 years and had a
complete ophthalmic check up.
Results: The incidence of ROP in the 552 infants
who were screened was 22.3%. No ROP was found in infants weighing
³ 2000g or with a gestational age
more than 36 weeks. Risk factors predisposing to ROP were septicemia
(P<0.001), apnea (P=0.0001) and oxygen therapy (P=0.031). Out of the 123
infants who had ROP, 41 (33.6%) needed laser photocoagulation. Twenty
two (53.6%) were seen at 3 years of age. Ten children had myopia, 1 had
amblyopia and 9 children had completely normal structural and visual
outcome. Only two (9%) children were blind due to retinal detachment.
Conclusion: One third of the infants with ROP
needed laser photocoagulation, the outcome of which was good. Risk
factors predisposing to ROP were septicemia, apnea, oxygen therapy and
use of blood products.
Key words: Laser photocoagulation, Follow-up, Retino-pathy of
prematurity, Visual outcome, Risk factors.
|
|
R
etinopathy of prematurity (ROP) is
a disease process mostly reported in preterm neonates with a wide
spectrum, ranging from mild, transient changes in the retina with
regression to severe progressive vasoproliferation, scarring, detachment
of retina and blindness. If identified early, it can be treated
successfully. In 1942, Terry(1) first described retrolental fibroplasia
with implication of oxygen therapy as the causative agent. Hence,
administration of oxygen in prematures was severely curtailed, resulting
in increased mortality. Today it is well known that oxygen therapy is not
the single causative factor, but many other risk factors play a causative
role in the pathogenesis of ROP(2,3).
The aim of this prospective study was to find out the
incidence of ROP in a tertiary care centre in a developing country. It
also attempts to identify the risk factors which predispose to ROP in a
large population of Neonatal Intensive Care Unit (NICU) graduates and the
long term outcome of those treated with laser photocoagulation.
Methods
All neonates weighing <1500g and/or with a gestation
£32
weeks admitted to our NICU were routinely screened for ROP between the
years 2000-2006. The initial examination was carried out at 4 weeks after
birth or 31 to 33 weeks postconceptional age, whichever was later(4). All
the infants were screened by the same ophthalmologist(VP).
Ethical clearance was obtained from the hospital ethics
committee and informed consent of the parents was also obtained.
Neonates with birthweight
³
1500g or gestational age more than 32 weeks were screened if they had an
unstable neonatal course with risk factors like ventilation, oxygen
requirement, use of surfactant, septicemia, hyperbilirubinemia,
intraventricular hemorrhage, patent ductus arteriosus, exchange
transfusion, apnea and use of blood products. A detailed history including
birthweight, gestational age at birth, weight for gestation (AGA / SGA
status) and, problems during NICU stay and its management were recorded.
The screening was done with a binocular indirect
ophthalmoscope. Eyes were examined with an infant speculum and a Kreissig
scleral depressor, under topical anesthesia using 2% proparacaine drops.
The pupils were dilated by using 0.4% tropicamide +1.25% phenylepherine
eye drops two or three times, till full dilatation occurred. Retinopathy
was graded into stages and zones as per the ICROP classification(5,6).
Infants with normal vascularization upto the periphery
were not examined again. Those with ROP were examined every week till
regression occurred or till they reached threshold for laser treatment.
Any stage 3 ROP with plus disease with 5 contiguous clock hours of disease
or a total 8 noncontiguous clock hours in zone 1 or 2 was considered as
threshold for treatment(4).
Laser treatment: Laser photocoagulation was advised
for infants who developed threshold disease as per ICROP classification(5)
or earlier, if aggressive progression was seen in zone 1 disease. Laser
was done using 810nm red laser (iridex SLx) with laser indirect
ophthalmoscope as early as possible, at least within 7 days of diagnosis
of threshold plus disease. This was done under topical anesthesia, using
an infant wire speculum and scleral indentation in the NICU. The avascular
retina beyond the ridge was ablated using confluent medium intensity burns
over one session. Topical treatment with tobramycin and dexamethasone was
given for 5 days and an oral analgesic was given for one day. If
regression was found to be inadequate or skip areas were seen on
subsequent examination, laser was repeated after one or two weeks.
Follow up: All children who had laser therapy were
asked to come for regular follow up. At the age of 3 years, they were
called for a detailed ophthalmic examination.
Statistical analysis: Analysis was performed using
SPSS version 10.0. Univariate analysis was conducted using Chi square
test. Multiple logistic regression analysis was performed to study the
predictors of ROP using independent variables as those variables which
were significant in the univariate analysis.
Results
Five hundred and fifty two infants were screened for
ROP in the NICU from year 2000 to 2006. Their birthweight ranged from
550-2499g with a mean of 1306 ±267g.
The gestational age ranged from 26-37 weeks with a mean of 31.4±2.2
weeks. There were 340 males and 212 females. ROP was seen in 123 infants
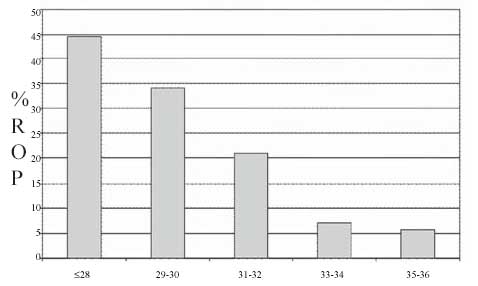
and the overall incidence of ROP was 22.3%. The incidence of ROP according
to gestational age is shown in Fig. 1. As the gestational
age decreased, the incidence of ROP increased (P=0.003). The
incidence of ROP in 58 ELBW infants was 36.2%, in the 381 VLBW infants, it
was 23.6% and was 11.4% in 105 infants weighing 1500-1999g. No ROP was
seen in infants with birth weight
³2000g
and gestational age more than 36 weeks. The frequency distribution of
stages of ROP is shown in Table I.
 |
|
Fig. 1 Incidence of ROP according to
gestational age. |
Table I
Frequency Distribution of Stages of ROP
| |
Left Eye
n (%) |
Right Eye
n (%) |
| I |
46(39.6) |
49(39.8) |
| II |
40(34.5) |
43(34.9) |
| III |
23(20.2) |
23(18.7) |
| IV |
5(4.4) |
6(4.9) |
| V |
2(1.7) |
2(1.6) |
| Total |
116 |
123 |
Table II
The Univariate and Multivariate (Independent) Determinants of ROP
| Risk factor |
ROP (+ve)
(n=123) (%) |
ROP (–ve)
(n=429) (%) |
Univariate
analysis
Odds Ratio
95% CI |
Multivariate analysis
Odds Ratio
95% CI |
P-value |
| Seizures |
2.5 |
0.7 |
3.46 |
0.48-24.97 |
1.04 |
0.11-9.60 |
0.969 |
| Oxygen therapy |
64.5 |
39.7 |
2.75 |
1.81-4.19 |
1.89 |
1.06-3.39 |
0.031 |
| Ventilation |
41.7 |
24.8 |
1.69 |
1.23-2.34 |
1.06 |
0.55-2.01 |
0.867 |
| Exchange transfusion |
20.2 |
13.5 |
1.62 |
0.93-2.81 |
1.60 |
0.75-3.43 |
0.220 |
| Blood products use |
23.6 |
14.2 |
1.86 |
1.13-3.06 |
1.68 |
0.86-3.28 |
0.125 |
| Hyperbilrubinemia |
56.1 |
51.0 |
1.22 |
0.82-1.83 |
0.78 |
0.45-1.37 |
0.390 |
| PDA |
8.6 |
4.4 |
2.06 |
0.78-5.43 |
1.60 |
0.52-4.92 |
0.407 |
| Apnea |
38.4 |
10.7 |
5.19 |
2.91-9.23 |
3.75 |
1.98-7.09 |
0.0001 |
| Septicemia |
22.0 |
11.4 |
2.17 |
1.29-3.66 |
3.13 |
1.56-6.29 |
0.001 |
| CPAP |
68.9 |
67.4 |
1.07 |
0.49-2.31 |
0.74 |
0.26-2.12 |
0.578 |
When we looked at the year-wise distribution of the
incidence of ROP, it was 24.4% in 2000 and 27.3% in 2001. It declined to
16.7, 19.5, 18.4% in 2002, 2003 and 2004, respectively. However, it rose
to 26% in 2005 and 2006, as we started saving smaller babies. There was no
significant difference in the incidence of ROP between males and females.
There was no difference in the incidence of ROP between appropriate for
gestational age (AGA) and small for gestational age (SGA) low birthweight
infants.
A univariate analysis was initially done taking each
risk factor. The risk factors included were oxygen therapy, seizures,
ventilation, exchange transfusion, use of blood products, patent ductus
arteriosus, septicemia, continuous positive airway pressure (CPAP), apnea,
hyperbilirubinemia. Septicemia (P=0.003), apnea (P=0.0001),
oxygen therapy (P=0.0001), ventilation (P=0.001) and use of
blood products (P=0.013) were found to be significant. When these
were put in a multiple logistic regression, only apnea, septicemia and
oxygen therapy were found to be significant, as shown in Table
II.
In 116 infants, both eyes were affected. In 7 infants,
only one eye was affected. Laser photocoagulation was done in 41 (33.3%)
infants out of the 123 infants having ROP. Table III
shows the frequency distribution of infants requiring laser therapy
according to gestational age and birth weight. More than one laser was
needed in 9 infants. All babies withstood the procedure well and there
were no post-laser complications other than reddening of the conjunctiva,
which disappeared in 2-3 days.
Table III
Proportion of Infants Requiring Laser Therapy According to Gestational
Age and Birthweight
|
Gestational |
Total |
Laser |
Birthweight |
Total |
Laser |
|
age (wks) |
|
n (%) |
(g) |
n |
n (%) |
| ≤ 28 |
31 |
12(38.7) |
<1000 |
24 |
11(45.8) |
| 29-30 |
55 |
17(30.9) |
1000-1499 |
128 |
24(18.8) |
| 31-32 |
60 |
6(10) |
1500-1999 |
31 |
6(19.4) |
| 33-34 |
33 |
6(18.2) |
2000-2499 |
3 |
0 |
| 35-36 |
6 |
0 |
– |
– |
– |
| ≥ 37 |
1 |
0 |
– |
– |
– |
An effort was made to recall all children who had
undergone laser therapy at the age of 3 years. Those born in 2005 and 2006
had not completed 3 years at the end of the study. Four children were lost
to follow up. Twenty two children had a complete ophthalmic checkup
(53.6%). Ten children had myopia and needed glasses and one had amblyopia.
Nine children had completely normal structural and visual outcome. Two
children had poor outcome (9%). One girl had retinal detachment and is
blind in one eye, and another boy had retinal detachment in both eyes and
is totally blind.
Discussion
We screened all babies admitted to our NICU with
birthweight <1500g and gestation
£32
weeks. Infants with birthweight
³1500g
and gestation more than 32 weeks were screened only if they had additional
risk factors. In a recent article, Chawla, et al.(7) have
suggested the same screening criteria. As reported by Palmer, et al.(8),
incidence and severity of ROP was closely related to lower birthweight and
lower postconceptional age, as was seen in our study. The incidence of ROP
of 22.6% in our study was much lower than that reported by Gopal, et
al.(9) in 1995. In more recent studies, incidence of ROP reported is
similar to our incidence(10,11).
There are varying screening criteria described by
different authors. Maheshwari, et al.(12) screened all babies
weighing <1500g with a gestational age <35 weeks. Gupta, et al.(11)
screened all babies £1500g
and/or gestational age
£35
weeks. Vinekar, et al.(13) suggested that the scenario in
developing countries is quite different. Larger and gestationally ‘older’
infants are more likely to develop ROP compared to their counterparts in
Western countries. Hence, the application of Western screening guidelines
for developing countries has been questioned by Jalali, et al.(14).
As a higher cutoff limit, they recommended screening babies born at <37
weeks gestation and/or birthweight <2000g in the presence of a high
sickness score, in order to prevent missing any infant with threshold ROP.
Goble, et al.(15) felt that they were screening too many babies for
ROP and recommended that babies with birthweight above 1250g should not be
screened. In our study, we would have missed 12 cases of ROP needing laser
if we had used <30 weeks criteria, as per American Academy of Pediatrics
(AAP) updated recommendations(16).
Many risk factors have been reported to predispose to
the development of ROP. Oxygen therapy, anemia, double volume exchange,
packed cell volume transfusion, septicemia, apnea and clinical sepsis are
important risk factors(10,13, 17,18). In our study, oxygen administration,
septicemia, and apnea were found to be significant risk factors. Vinekar,
et al.(13) also found that septicemia was a significant risk
factor. Aggarwal, et al.(10) found apnea, clinical sepsis and male
sex to be significant risk factors. We started using surfactant
sparingly in 2001, and then more frequently in later years. Seventy one
neonates received surfactant, out of which 37 had ROP and 34 had no ROP.
Seiberth, et al.(4) found surfactant a significant risk factor, but
we did not find it significant.
It has been suggested that 13% of infants would be
missed if AAP criteria are applied(19). So, we feel that all babies with
birthweight less than 1500g and gestation
£32
weeks should be routinely screened. Infants with birthweight between
1500-2000g and gestational age more than 32 weeks should be screened at
the discretion of the neonatologist, depending on other risk factors
during the course of stay in the NICU.
Ng, et al.(19) and Connolly, et al.(20)
have reported that long term structural and functional outcome using laser
was superior to that obtained with cryotherapy. Favorable results were
obtained in 83% eyes treated with laser as compared to only 25% treated
with cryotherapy. Laser obviates the need for general anesthesia and
hardly has any complications. We found that the results of laser are
extremely satisfactory and only 2 children (9%) had poor outcome, out of
the 22 children who were available for 3 year follow up.
Since ROP is essentially asymptomatic in the early
stages, standards of practice now demand carefully timed retinal
examination of at risk infants for ROP by an ophthalmologist experienced
in the examination of the retina, to minimize the risks of visual loss by
these infants.
Acknowledgment
We gratefully acknowledge the help of Dr Vaijayanti
Deodhar for doing the follow up ophthalmic examination and Ms Anjali Mote
for statistical analysis.
Contributors: SC conceived the project, supervised
data collection, wrote the manuscript and will be guarantor for the paper.
VP did the retinal examination and laser photocoagulation and helped to
write the article. UV was in charge of the clinical management in NICU and
reference for ROP screening. SK was in charge of the clinical management
in NICU and reference for ROP screening. AK collected data, helped in
statistical analysis and writing of the article. The final manuscript was
approved by all authors.
Funding: None.
Competing interest: None stated.
|
What is Already Known?
• Prematurity, oxygen administration, septicemia,
apnea and blood transfusion predispose to retinopathy of prematurity
(ROP).
What This Study Adds?
• Bigger and gestationally more "mature" babies
can develop ROP. Laser photocoagulation is a safe therapeutic
procedure with good outcome. |
References
1. Terry TL. Extreme prematurity and fibroblastic
overgrowth of persistent vascular sheath behind each crystalline lens. Am
J Ophthalmol 1942; 25: 203-204.
2. Hammer ME, Mullen PW, Fergusson JG, Poi S, Cosbox C.
Jackson KL. Logistic analysis of risk factors in acute retinopathy of
prematurity. Am J Ophthalmol 1986; 102: 1-6.
3. Seiberth V, Linderkamp O. Risk factors in
retinopathy of prematurity. A multivariate statistical analysis.
Ophthalmologica 2000; 214: 131-135.
4. American Academy of Pediatrics. Screening
examination of premature infants for retinopathy of prematurity.
Pediatrics 2001; 108: 809-811.
5. International Committee for the Classification of
Retinopathy of Prematurity. Multicenter trial of cryotherapy. An
international classification of retinopathy of prematurity. Arch
Ophthalmol 1984; 102: 1130-1134.
6. International Committee for the Classification of
the Late Stages of Retinopathy of Prematurity. An international
classification of retinopathy of prematurity II. The classification of
retinal detachment. Arch Ophthalmol 1987; 105: 906-912.
7. Chawla D, Agarwal R, Deorari AK, Paul VK.
Retinopathy of prematurity. Indian J Pediatr 2008; 75: 73-76.
8. Palmer EA, Flynn JT, Hardy RJ, Phelps DL, Phillips
CL, Schaffer DB, et al. Incidence and early course of retinopathy
of prematurity. Ophthal-mology 1991; 98: 1628-1640.
9. Gopal L, Sharma T, Ramachandran S, Shanmuga-sundaram
R, Asha V. Retinopathy of prematurity: A study. Indian J Ophthalmol
1995;43: 59-61.
10. Aggarwal R, Deorari AK, Azad RV, Kumar H, Talwar D,
Sethi AI. Changing profile of retinopathy of prematurity. Trop Pediatr
2002; 48: 239-242.
11. Gupta VP, Dhaliwal U, Sharma R, Gupta P, Rohtagi J.
Retinopathy of prematurity – risk factors. Indian J Pediatr 2004; 71: 887-
892.
12. Maheshwasri R, Kumar H, Paul VK, Singh M, Deorari
AK, Tiwari AK. Incidence and risk factors of retinopathy of prematurity in
a tertiary newborn unit in New Delhi. Natl Med J India 1996; 92: 211-214.
13. Vinekar A, Dogra M, Sangtam T, Narang A, Gupta A.
Retinopathy of prematurity in Asian Indian babies weighing greater than
1250 grams at birth: ten year data from a tertiary care center in a
developing country. Indian J Ophthalmol 2007; 55: 331-336.
14. Jalali S, Anand R, Kumar H, Dogra MR, Azad RV,
Gopal L. Programme planning and screening strategy in retinopathy of
prematurity. Indian J Ophthalmol 2003; 51: 89-99.
15. Goble RR, Jones HS, Fielder AR. Are we screening
too many babies for retinopathy of prematurity? Eye 1997; 11: 509-514.
16. Screening examination of premature infants for
retinopathy of prematurity. Section on Ophthal-mology, American Academy of
Pediatrics. American Academy of Ophthalmology. Pediatrics 2006; 117:
572-576.
17. Rekha S, Battu RR. Retinopathy of prematurity:
incidence and risk factors. Indian Pediatr 1996; 33: 999-1003.
18. Dutta S, Narang A, Dogra MR, Gupta A. Risk factors
of threshold retinopathy of prematurity. Indian Pediatr 2004; 41: 665-671.
19. Ng EY, Connolly BP, McNamara JA, Regillo CD, Vander
JF, Tasman W. A comparison of laser photocoagulation with cryotherapy for
threshold retinopathy of prematurity at 10 years. Part 1- Visual function
and structural outcome. Ophthalmology 2002; 109; 928-934.
20. Connolly BP, Ng EY, McNamara JA, Regillo CD, Vander JF, Tasman W. A
comparison of laser photocoagulation with cryotherapy for threshold
retinopathy at 10 years. Part 2- Refractive outcome. Ophthalmology 2002;
109: 936-941. |
|
|
 |
|

