|
|
|
Indian Pediatr 2017;54:
455-459 |
 |
Family-Centered Care to Complement Care of
Sick Newborns: A Randomized Controlled Trial
|
|
Ankit Verma, Arti Maria, *Ravindra
Mohan Pandey, $Charoo
Hans, Arushi Verma and #Fahima
Sherwani
From Departments of Pediatrics and $Microbiology,
PGIMER and Dr. RML Hospital; *Biostatistics, AIIMS; and
#Management Studies, IIT; New Delhi, India.
Correspondence to: Dr Arti Maria, Neonatal Division,
Department of Pediatrics, PGIMER and Dr. RML Hospital, Baba Kharak Singh
Marg, New Delhi, India 110 001.
Email: [email protected]
Received: June 28, 2016;
Initial review: October 14, 2016;
Accepted: April 10, 2017.
Trial Registration: Clinical Trial Registry of
India (CTRI/2013/09/003969)
|
Objective: To assess the impact
of family-centered care in delivery of care to sick newborns, on
nosocomial infection rate.
Design: Randomized controlled
trial
Setting: Tertiary referral
nursery (October 2010 to March 2012).
Participants: 295 neonates
randomized at the time of hospitalization in neonatal intensive care
unit.
Intervention: Parent-attendant of
intervention group were trained using an indigenously developed and
pretested, culturally sensitive, simple audio-video tool that covered
domains of personal hygiene, hand washing, danger signs recognition and
feeding of sick neonate. Control group received routine care by nurses
and doctors.
Outcome measure: Primary:
culture positive nosocomial infection rate. Secondary: culture
negative nosocomial infection rate, duration of hospitalization,
mortality and breastfeeding rate.
Results: Two-thirds of family
caregivers were fathers/ mothers and about 20% were grandparents. About
60% of family care givers were either illiterate (25%) or primary/middle
pass (34%). Incidence of nosocomial episodes of sepsis was not different
between groups (incidence rate difference 0.74, 95 % CI -4.21, 5.6, P
= 0.76). Pre-discharge exclusive breastfeeding rates were significantly
higher in intervention group [80.4% vs 66.7% (P=0.007)].
Conclusions: There was no
significant difference in nosocomial infection rate between the two
groups. Translating and adapting principles of family-centered care was
feasible, and improved the pre-discharge exclusive breastfeeding rates.
Keywords: Breastfeeding, Capacity building,
Caregivers, Cross infection, Patient care team.
|
|
F
amily-centered care (FCC) in neonatal intensive
care unit (NICU) setting is an approach to develop and nurture the
family's role in partnership with that of the healthcare team in care of
a sick neonate. Implementation of this strategy has shown to decrease
length of stay, improve wellbeing of preterms, allow better allocation
of resources and enhance parent infant bonding [1-6]. However, impact of
FCC on nosocomial infections has not been evaluated.
We hypothesized that capacity-building and involving
parents through a structured training program for a supervised delivery
of limited care to their own baby in nursery to complement the
conventional care by nurse-doctor will reduce the nosocomial infection
rate. This was based on the premise that the parents have more interest
than anyone else in their baby’s wellbeing. Hence whatever capacity is
built for delivery of care to their sick baby during the opportunity of
contact during hospitalization is likely to be complied fully not only
through the hospital stay but also even likely to be carried at home
discharge. While the doctor/nurse continues to be the primary caregiver,
involvement of parents leads to sharing of work.
Methods
This study designed as a randomized controlled trial
was conducted between October 2010 to March 2012 in a setting of
16-bedded referral neonatal unit of Northern India with 2 or 3 nurses
and one resident doctor available as care providers round-the-clock.
Nursery has an intensive side with provision for tertiary care and a
step-down side. Free visitation by mothers/parent attendants is allowed
only in the step-down side. The trial was approved by the Institutional
Ethical Committee.
The primary objective was to document impact of
structured parental participation of parent attendants in delivery of
care to their sick neonates on culture-positive nosocomial infection
rate. The secondary objectives were to document effects of this
intervention on mortality, median duration of hospital stay,
breastfeeding rate and culture-negative nosocomial infection rate.
Nosocomial infection was defined as any episode of sepsis developing
after 72 hours or more of hospitalization, and the rate was calculated
as number of sepsis episodes per 1000 patient- days of admission [7]. A
new episode of nosocomial infection was defined in a baby who was doing
clinically well and off-antibiotics for at least last 7 days, developing
clinical features compatible with sepsis.
Hypothesizing about 50% reduction in nosocomial
infection rate from existing rate of about 20 infections/1000
patient-days (with ±10% precision) at 80% power and 5%
a error, sample size
of 2157 patient-days in each group was estimated. Assuming 15
patient-days, we required to enroll about 150 patients in each group.
Participants: All neonates admitted to NICU who
were accompanied by at least two attendants
(mother/father/grandparents/relatives) were eligible. After initial
assessment, stabilization and appraisal about baby's condition, the
accompanying parent/attendants were asked for a written informed consent
after they had viewed the research information video.
Neonates whose accompanying attendant refused to
consent, or who were critically sick or hemodynamically unstable or had
any major malformation incompatible with life or were product of
multiple gestation were excluded from the study. The enrolled babies
were randomized: control group received care from the nurses and doctors
as per routine unit practice and the intervention group in addition to
nurses and doctors received a supervised delivery of a package of care
by the parent-attendants of the baby who were trained using an
indigenously developed audio-visual training module (study tool).
Randomization: Computer generated random number
sequence was generated by a person not otherwise involved with the
study, using STATA 9.0 version. Allocation concealment was ensured using
sequentially numbered, opaque, sealed and stapled envelopes that were
opened by the primary investigator at the time of randomization. Given
the nature of intervention being clinical care, blinding was not
possible.
Intervention: A simplified comprehensive
audio-visual training tool was prepared with multidisciplinary technical
input from a neonatologist, community medicine specialist, psychologist,
nurse, and hindi-language expert. The objective of this module was to
make aware, educate, train, and build the capacity of the accompanying
parent-attendant in various elementary skills pertaining to sick newborn
care. The module content was structured into four sequential parts: Part
1 pertaining to preparing the attendant for entry into nursery
(information about dos and don'ts before entry, learning steps of hand
washing, wearing gown, change of soiled diapers); Part 2 related to
familiarization with nursery environment (information about care under
warmer and phototherapy, stability of fixation of warmer/ pulse oximeter
probes/orogastric tube/oxygen nasal prongs and intravenous (IV) cannula.
Drawing nurses' attention towards monitor-alarms and redness/swelling at
IV sites; Part 3 focused on building skills of recognizing and reporting
danger signs (noticeable change in colour/activity/breathing
pattern/bleeding rash/gastric aspirates/vomiting, abdominal distension,
altered stool colour), to note frequency of stool/urine passed; and Part
4 on teaching orogastric/paladay/katori-spoon feeding.
Pre-implementation testing of the tool was done by administering to ten
parents from varied religious/language/socioeconomic/literacy
backgrounds and incorporating constructive feedbacks for tool
improvement. Tool was re-administered and rechecked for comprehension
and clarity, until approved by experts for final implementation.
Kangaroo mother care, breastfeeding, milk expression and discharge
counselling were taught and practiced in both groups as standard
practices of our nursery.
Once enrolled following consent for participation,
2-3 attendants per baby were initiated into daily training between 10 AM
to 12 noon. Audio-video module was screened sequentially from part 1 to
part 3, respectively from day 1 to day 3 after initiation of the
training process for the attendants. Part 4 was screened and training
for feeding begun once the infant was considered ready for enteral
feeding. This screening was done either individually or in groups. The
audio-video training was supplemented with demonstrations as and when
required by the principal investigator. Other resident doctors and
nurses in the unit were similarly trained to impart training to
participating parent-attendants (in case principle investigator was not
available). Repeated sequential screening of audio-visual module parts
1-4 were done until the attendants demonstrated satisfactory skill
learning as assessed by the investigators. Reinforcement and interactive
revision of the module was done each time they viewed next part.
Lateral/horizontal learning was encouraged among attendants. The
attendant imparted care to their respective babies with these acquired
skills (Table I).
TABLE I Acquired Skills and Their Assessment: An Overview
|
Part of |
Skill taught |
Assessment |
|
module |
|
|
|
Part 1 |
Gowning |
Observing the attendant |
|
Handwashing |
Demonstrating at least 4 |
|
Cleaning the |
out of 6 steps of hand |
|
soiled baby |
washing correctly |
|
Part 2 |
Covering eyes/ genitals |
Documentation in |
|
in phototherapy |
nurse's chart |
|
Checking warmer/ pulse-ox |
|
|
probe stability/fixation |
|
|
Swelling and redness at |
|
|
I/V cannula site |
|
|
Part 3 |
Recognition and reporting |
Monitoring by nurses/ |
|
of danger signs |
residents |
|
Part 4 |
Orogastric/paladay/katori- |
Supervisory |
|
spoon feeding |
|
Outcomes: The episodes of nosocomial infection
(culture positive and negative), duration of stay, final outcome
(discharge/LAMA/death) and number of babies breastfeeding at the time of
discharge were documented as per the pre-set definitions in both groups.
Data were recorded in a predesigned performa and managed on an Excel
spreadsheet. Actual time spent bedside in previous 24 hours was noted
weekly by direct enquiry from attendants.
Statistical analysis: Characteristics of
participants in both the groups were compared using Students 't' test
(quantitative variables), or Chi-square test (categorical variables).
Effect size and its 95% CI were computed for the primary and secondary
outcomes. Stratified analysis was done only as exploratory analysis.
Analysis was done by ‘intention to treat’, using STATA 9.0.
Result
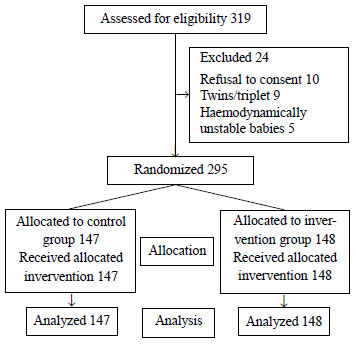
We randomized 295 out of 319 eligible newborns to
either the control group (n= 147) or intervention group (n=148)
after 24 exclusions (Fig. 1).
 |
|
Fig. 1 Study flow chart.
|
Mean (SD) weight and gestational age in control and
intervention groups were 2303 (67) g and 2376 (65) g; 36.4 (3.2) weeks
and 36.8 (3.1) weeks, respectively. The baseline characteristics are
shown in Table II.
TABLE II Baseline Characteristics of Enrolled Babies
|
Characteristics |
Control gp |
Intervention gp |
|
n=147, n (%) |
n=148, n (%) |
|
Gestational age (wks) |
|
|
|
<28 |
9 (3.0) |
7 (2.3) |
|
29-34 |
25 (8.5) |
21 (7.1) |
|
35-42 |
113 (76.8) |
120 (81.0) |
|
Gestation* (wk) |
36.4 (3.2) |
36.8 (3.1) |
|
Weight* (g) |
2303 (67) |
2376 (65) |
|
Age at admission* (d) |
6.9 (7.6) |
7.7 (8.9) |
|
SGA |
33 (11.2) |
27 (9.1) |
|
Male gender |
102 (69.4) |
101 (68.2) |
|
Home delivery |
95 (64.6) |
96 (64.8) |
|
Vaginal delivery |
118 (80.2) |
119 (80.4) |
|
Birth asphyxia |
31 (10.5) |
27 (9.1) |
|
Previous hospitalization |
|
|
|
Single |
22 (14.96) |
21 (14.2) |
|
Multiple |
10 (6.80) |
8 (5.4) |
|
Stability at admission |
|
|
|
Severe hypothermia |
1 (0.68) |
6 (4.0) |
|
Fever |
5 (3.40) |
10 (6.7) |
|
#Saturation <85% |
20 (13.6) |
16 (10.8) |
|
Hypoglycaemia |
10 (6.8) |
4(2.7) |
|
Invasive procedures |
|
|
|
PICC line n (d) |
23 (124) |
27 (167) |
|
Umbilical cath. n (d) |
33 (175) |
34 (170) |
|
Surgical intervention n (%) |
1 (0.68) |
2 (1.35) |
|
Ventilated n (d) |
37 (149) |
31 (296) |
|
Values in No. (%) or *mean (SD); #Oxygen saturation;
PICC: Peripherally-inserted central catheter. |
Majority (37%) of parent-attendants were fathers, 20%
were grandparents, mothers were 22% initially and 30% later. One-fourth
(25%) were illiterate, 34% were primary/middle school level and only 2%
were graduates. 40% were aged 25-35 years, 19% being 36-50 years, and
41% were >50 year-old. Mean (SD) time spent bedside by attendant was
14.7 (1.1) hours/day.
 |
|
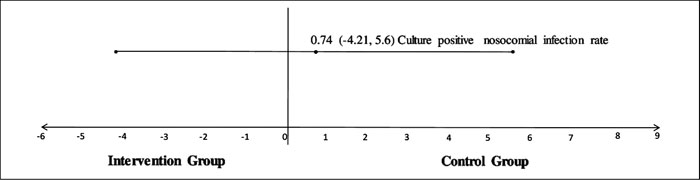
Fig. 2 Differences in incidence rate
of culture positive nosocomial infection.
|
Total nosocomial infection episodes were 75; 38
(culture positive 22, culture negative 16) in control group and 37
(culture positive 23, culture negative 14) in intervention group. No
episode of nosocomial infection was reported in step-down side of the
nursery. Total nosocomial infection rates (culture positive and culture
negative) were 24.72 and 24.02 episodes per 1000 baby days in control
and intervention groups, respectively (P=0.7). Culture positive
and culture negative nosocomial infection rates between the control and
intervention groups were not significantly different (Table
III and Fig. 2). Median (IQR) duration of
hospitalization in control and intervention group was 11 (7,18) days and
11.5 (7,17.5) days, respectively (P>0.05). The mortality was 8.8%
in control as compared to 6.8% in intervention group. The breastfeeding
rate in control group was 66.7 % as compared to 80.4% in intervention
group (P=0.007).
TABLE III Summary of Outcomes in the Two Group of Sick Newborns
|
Outcome variables |
Control group |
Intervention group |
Mean difference (95% CI) |
P value |
|
(n=147) |
(n=148) |
|
|
|
Culture positive nosocomial infection rate |
7.17 |
6.43 |
0.74 (-4.21, 5.6) |
0.76 |
|
Culture negative nosocomial infection rate |
9.86 |
10.56 |
-0.70 (-6.6,5.2) |
0.82 |
|
Duration of stay, median (IQR) |
11 (7,18) |
11.5 (7,17.5) |
|
>0.05 |
|
Mortality, No. (%) |
13 (8.8) |
10 (6.8) |
(0.042,0.134) |
0.5 |
|
Breastfeeding rate, No. (%) |
98 (66.7 ) |
119 (80.4) |
(0.59,0.74) |
0.007 |
Discussion/p>
In this randomized controlled trial evaluating
family-centered care of sick newborns admitted in a NICU, we did not
find a significant impact on reducing nosocomial infections. The
intervention significantly improved breast feeding rates before
discharge. This may reflect an easier transition from intensive to the
step-down side and better preparedness in this group since mothers were
involved through the period of hospitalization of the baby.
Few studies have evaluated impact of various
interventions within the ambit of FCC and have shown improved health
outcomes for neonates and families. Bhutta, et al. [8] had
allowed free visitation of mothers in step-down area for care of stable
very low birth weight (VLBW) infants and found that this was associated
with reduced duration of stay and decreased nosocomial infection.
Parents in COPE trial had received written and audiotaped information
and performed behavioral activities to parent preterms. This reduced
their duration of hospitalization [3,9]. In Stockholm Neonatal Family
Centered Care Study [10], parents were allowed to stay for 24 hours and
this reduced total hospital stay duration in preterm neonates admitted
to a level 2 NICU. O'Brien, et al. [11] developed a Family
Integrated Care model for parental participation in care of preterm
babies by getting trained with daily education sessions that improved
breast feeding rates and weight gain. Importance of providing peer
support to NICU parents, delivered through hospital or community based
programs to complement services of NICU staff has been realised. It has
been recommended that offering peer support to NICU parents should be an
integral part of NICU services [12].
We could not demonstrate a positive impact of FCC in
reducing nosocomial infections, our study could be underpowered to
detect small differences as we calculated our sample size based on an
ambitious 50% reduction. We have not assessed long term outcomes as also
perspectives of various stake-holders. It is possible that this
intervention that involves competency building of family attendant with
respect to essential newborn care has far reaching consequences on
post-discharge outcomes.
Broad-based inclusion with limited exclusions and the
fact that the trial was conducted on parent attendants with varied
characteristics offer a good generalizability. Strict adherence to study
protocol with inbuilt quality assurance measures gives a good internal
validity to the study.
Possible implication of this trial is that parent
attendants could be trained for imparting care to their sick neonates in
human resource constrained setting like special care newborn units
(SCNUs) and help in strengthening the health care system with better
neonatal outcomes. Translating and adapting principles of family centred
care seems to be feasible. Additionally it is believed that empowering
and capacity building mothers/parent-attendants with care giving
competencies for their babies would be a cornerstone for providing a
continuum of care for these high risk NICU graduates at home after
discharge.
While this one as a preliminary study evaluated only
few outcomes, and implementation was shown to be feasible, more impact
evaluation research may be required including qualitative studies to
evaluate the perceptions of the stakeholders as this concept seems to
have promising potential to impact newborn care not only during their
hospitalization but also likely to impact their outcomes after
discharge.
Contributors: ANV: acquisition of data, initial
analysis, and interpretation of data, drafted the initial manuscript;
AM: conceptualized, designed and supervised the study, reviewed and
ensured quality assurance through the study, and revised the manuscript.
RMP: designed the study, analysis and interpretation of data, and
critically reviewed the manuscript; CH: acquisition of data,
interpretation of data, and critically reviewed the manuscript; ARV, FS:
analysis and interpretation of data, and drafting the article. All
authors approved the final version of manuscript.
Funding: None; Competing interest: None
stated.
|
What Is Already Known?
• Family-centered care in NICUs favourably
impacts outcomes.
What This Study Adds?
• Translating and adapting principles of
family-centered care to an operational, culturally-sensitive
module improved breastfeeding rates before discharge, but did
not affect nosocomial infection rates.
|
References
1. Forsythe P. New practices in the transitional care
center improve outcomes for babies and their families. J Perinatol.
1998;18:119-28.
2. Jotzo M, Poets CF. Helping parents cope with the
trauma of premature birth: An evaluation of a trauma-preventive
psychological intervention. Pediatrics. 2005;115: 915-19.
3. Melnyk BM, Fischbeck-Feinstein N, Alpert-Gillis L,
Fairbanks E, Grean HF, Sinkin RA. Reducing premature infants' length of
stay and improving parents' mental health outcomes with the COPE NICU
program: A randomized clinical trial. Pediatrics. 2006;118:1414-37.
4. Shields-Poe D, Pinelli J. Variables associated
with parental stress in neonatal intensive care units. Neonatal Netw.
1997;16:29-37.
5. Van Riper M. Family-provider relationships and
well-being in families with preterm infants in the NICU. Heart Lung.
2001;30:74-84.
6. Eichner JM, Johnson BH. Family-centered care and
the pediatrician's role policy statement. Pediatrics. 2003;112:691-96.
7. Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo
WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth
weight neonates: The experience of the NICHD Neonatal Research Network.
Pediatrics. 2002;110:285-91.
8. Bhutta Z, Khan I, Salat S, Raza F, Ara H. Reducing
length of stay in hospital for very low birthweight infants by involving
mothers in a stepdown unit: An experience from Karachi (Pakistan). BMJ.
2004;329:1151-5.
9. Mianaei S, Karahroudy F, Rassouli M, Tafreshi M.
The effect of Creating Opportunities for Parent Empowerment program on
maternal stress, anxiety, and participation in NICU wards in Iran. Iran
J Nurs Midwifery Res. 2014;19:94-100.
10. Ortenstrand A, Westrup B, Broström EB, Sarman I,
Åkerström S, Brune T, et al. The Stockholm Neonatal Family
Centered Care Study: Effects on length of stay and infant morbidity.
Pediatrics. 2010;125:278-85.
11. O'Brien K, Bracht M, Macdonell K, McBride T,
Robson K, O'Leary L, et al. A pilot cohort analytic study of
Family Integrated Care in a Canadian neonatal intensive care unit. BMC
Pregnancy Childbirth. 2013;13:S12.
12. Hall SL, Ryan DJ, Beatty J, Grubbs L.
Recommendations for peer-to-peer support for NICU parents. J Perinatol.
2015;35:9-13.
|
|
|
 |
|

