|
|
|
Indian Pediatr 2015;52: 528-529 |
 |
Mid-upper Arm Circumference for Detection of
Severe Acute Malnutrition in Infants Aged Between One and Six
Months
|
|
Siddharth Chand and *Dheeraj Shah
Department of Pediatrics, University College of Medical
Sciences and GTB Hospital, Dilshad Garden, Delhi, India.
Email: [email protected]
|
|
This study conducted among 302 infants aimed to determine the most
suitable mid-upper arm circumference cut-off to diagnose severe acute
malnutrition (weight-for-length <–3 SD) in infants aged between 1 and 6
months. The cut-off of
£11.0
cm had the best performance (Youden index 0.63, sensitivity 82.5%,
specificity 80.3%).
Keywords: Anthropometry, Infant, Protein
energy malnutrition.
|
|
Mid-upper arm circumference (MUAC) cut-off of 11.5 cm is used as an
independent diagnostic criterion to identify severe acute malnutrition
(SAM) in children aged between 6 months and 5 years [1]. MUAC is useful
for the purpose of mass screening and community-based diagnosis. The
existing burden of severe wasting (weight-for-length <–3 SD), which is
an indicator of SAM [1], in under-five children in India is 6.4% [2];
the prevalence is even higher (13.1%) in infants below 6 months of age
[2]. The mortality due to SAM has also been shown to be higher in
infants less than six months of age than in older children [3]. However,
role of MUAC in diagnosis of SAM below the age of 6 months of age has
not been studied adequately.
This hospital-based study was conducted in the
Department of Pediatrics, University College of Medical Sciences and GTB
Hospital, Delhi, India from July 2013 to April 2014. Infants aged
between one to six months attending the outpatient department or
admitted in the pediatric ward were screened. Infants showing clinical
evidence of edema, ascites, pleural effusion, a significant tumor or
mass, or length < 45 cm were excluded. Parental consent was obtained,
and ethical clearance was obtained from the Institutional Ethics
Committee. Weight, length and MUAC of all infants were recorded using
standard procedures [4]. Electronic weighing scale (Equinox, BE-EQ 22,
India) with a sensitivity of 10 g was used for recording the weight.
Non-stretchable plastic tape was used to measure MUAC. Weight-for-length
Z-scores (WLZ) was calculated using ‘WHO Anthro for PC’ software [5].
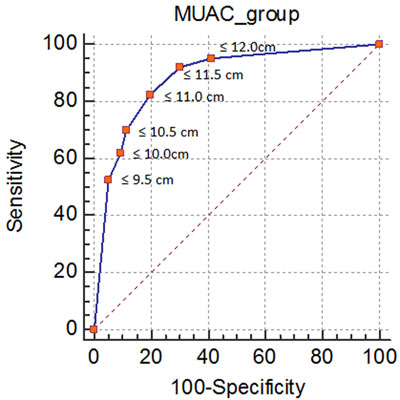
Sensitivity, specificity, Youden index (sensitivity+specificity-1), and
the likelihood ratio of positive and negative tests were calculated for
MUAC cut-offs of 9.5 cm, 10 cm, 10.5 cm, 11 cm, 11.5 cm, and 12 cm
against the presence of SAM (WLZ <–3). Receiver operating characteristic
(ROC) was plotted, including the area under the curve with 95%
confidence interval (CI) using Medcalc software (Version 13.3.3.0) to
assess the optimal MUAC cut-off point [6].
TABLE I Evaluation of Different Cut-offs of Mid-upper Arm Circumference (MUAC) for Diagnosis of SAM (N=302)
|
S.No. |
MAC Cut off (cm) |
Sensitivity (%) |
Specificity (%) |
Youden Index |
LR + |
LR - |
|
1. |
≤12.0 |
95.2% (60/63) |
59.0% (141/239) |
0.54 |
2.32 |
0.08 |
|
2. |
≤11.5 |
92.1% (58/63) |
69.9% (167/239) |
0.62 |
3.06 |
0.11 |
|
3. |
≤11.0 |
82.5% (52/63) |
80.3% (192/239) |
0.63 |
4.20 |
0.22 |
|
4. |
≤10.5 |
69.8% (44/63) |
88.7% (212/239) |
0.59 |
6.18 |
0.34 |
|
5. |
≤10.0 |
61.9% (39/63) |
90.8% (217/239) |
0.53 |
6.72 |
0.42 |
|
6. |
≤9.5 |
53.7% (34/63) |
95.0% (227/239) |
0.49 |
10.43 |
0.50 |
|
SAM: Severe acute malnutrition; LR +: Likelihood ratio for
positive test; LR -: Likelihood ratio for negative test. |
We approached 310 infants for the study; 302
(180 males) were finally included. One-third of the participants (n=101)
were enrolled from the pediatric ward. The mean (SD) age of the subjects
was 99.5 (49.1) days. The number of infants aged between 1-2 months, 3-4
months , and 5-6 months were 147 (48.7%), 97 (32.1%), and 58 (19.2%),
respectively. The mean (SD) weight, length, and MUAC were 4.73 (1.37)
kg, 58.4 (5.0) cm and 11.6 (2.0) cm, respectively. The number of infants
with WLZ >–2, between –2 and –3, and <–3, were 176 (58.2%), 63 (20.9%)
and 63 (20.9%) respectively. The sensitivity, specificity, Youden index,
and the likelihood ratio of positive and negative tests of different
MUAC cut offs for diagnosing SAM have been presented in the Table
I. The MUAC cut-off £11.0
cm yielded the highest Youden index of 0.63 and had high sensitivity
(82.5%) and specificity (80.3%). Fig. 1 shows the ROC
curve comparing the MUAC cut-offs; the best performance was that of 11.0
cm. The total area under ROC curve was 0.884 [95% CI: 0.842, 0.918; P<0.001].
*Values of sensitivity and specificity in percent .
|
|
Fig. 1 Receiver operating
characteristic curve.
|
The limitations of the study include the
hospital-based setting involving a convenience sampling. The MUAC
cut-offs also need to be studied with the functional outcomes such as
risk of infections, morbidity, and related mortality.
With the use of WHO growth standards published in
2006 [7], MUAC cut-off of £11.5
cm is used to diagnose SAM in the age group 6 months-5years [1]. MUAC
cut-off of £12.0cm
has been suggested to be more suitable to diagnose SAM in the Indian
setting [8]. MUAC was shown to be more reliably measured by the
community health workers than WLZ in infants less than 6 months of age
[9]. Another study has suggested using MUAC cut-off of
£11.0 cm to identify
infants in the age group 6-14 weeks with a markedly increased risk of
death [10]. The results of the present study support that the MUAC
cut-off of £11.0
cm can be used for diagnosing SAM in infants below the age of 6 months.
References
1. WHO Child Growth Standards and the Identification
of Severe Acute Malnutrition in Infants and Children. A Joint Statement
by the World Health Organization and the United Nations Children’s Fund.
Geneva: World Health Organization, 2009. Available from:
http://www.who.int/nutrition/publications/severemalnutrition/9789241598
163/en/. Accesses February 3, 2015.
2. National Family Health Survey (NFHS-3), India,
2005-2006. Available from: http://dhsprogram.com/pubs/pdf/SR128/SR128.pdf.
Accessed October 5, 2014.
3. Management of Acute Malnutrition in Infants (MAMI)
project. Emergency Nutrition Network, UCL Centre for International
Health & Development, Action Contre la Faim, 2010. Available from:
http://reliefweb.int/sites/reliefweb.int/files/resources/8A7E77D26B35660F49
2576F70010D7DF-mami-report-complete.pdf. Accessed December 1, 2014.
4. Shah D, Sachdev HPS. Measuring Undernutrition and
Overnutrition in Children. In: Vir S, Editor. Advance
Public Health and Nutrition. New Delhi: 2010.
5. WHO Anthro for Personal Computers, Version
3.2.2,2011: Software for assessing growth and development of the world’s
children. Geneva: WHO; 2010. Available from:
http:/www.who.int/childgrwoth/software/en/. Accessed October 5,2014.
6. Medcalc statistical software, Version 13.3.3.0.
Available from http://www.medcalc.org/download.php. Accessed
October 5, 2014.
7. World Health Organization, Multicentre Growth
Reference Study Group. WHO Child Growth Standards:
Length/height-for-age, weight-for-age, weight-for-length, weight
for-height and body mass index-for-age: Methods and development. Geneva:
World Health Organization; 2006. Available from:
http://www.who.int/childgrowth/standards /technical_report/en/.
Accessed February 3, 2015.
8. Shekhar S, Shah D. Validation of mid upper arm
circumference cut offs to diagnose severe wasting in Indian children.
Indian Pediatr. 2012;49:496-7.
9. Mwangome MK, Fegan G, Mbunya R, Prentice AM,
Berkley JA.Reliability and accuracy of anthropometry performed by
community health workers among infants under 6 months in rural Kenya.
Trop Med Int Health. 2012;17:622-9.
10. Mwangome MK, Fegan G, Fulford T, Prentice AM,
Berkley JA. Mid-upper arm circumference at age of routine infant
vaccination to identify infants at elevated risk of death: A
retrospective cohort study in the Gambia. Bull World Health Organ.
2012;90:887-94.
|
|
|
 |
|

