|
|
|
Indian Pediatr 2014;51:
457-462 |
 |
INCLEN Diagnostic Tool for Attention Deficit
Hyperactivity Disorder (INDT-ADHD):
Development and Validation
|
|
Sharmila Mukherjee, Satinder Aneja, Paul SS Russell, Sheffali Gulati,
Vaishali Deshmukh, Rajesh Sagar, Donald Silberberg, Vinod K Bhutani,
Jennifer M Pinto, Maureen Durkin, Ravindra M Pandey, MKC Nair, Narendra
K Arora and *INCLEN Study
Group
From The INCLEN Trust International, New Delhi, India.
Correspondence to: Dr Narendra K Arora, Executive Director, The
INCLEN Trust International, F1/5, Okhla Industrial Area, Phase-1, New
Delhi, India.
Email: [email protected]
Received: April 03, 2013;
Initial review: May 08, 2013;
Accepted:
February 15, 2014.
*INCLEN Study Group: Core Group: Alok Thakkar, Arun
Singh, Devendra Mishra, Gautam Bir Singh, Manju Mehta, Manoja K Das,
Monica Juneja, Nandita Babu, Poma Tudu, Praveen Suman, Ramesh Konanki,
Rohit Saxena, Savita Sapra, Sunanda K Reddy, Tanuj Dada. Extended
Group: AK Niswade, Archisman Mohapatra, Arti Maria, Atul Prasad,
BC Das, Bhadresh Vyas, GVS Murthy, Gourie M Devi, Harikumaran Nair, JC
Gupta, KK Handa, Leena Sumaraj, Madhuri Kulkarni, Muneer Masoodi, Poonam
Natrajan, Rashmi Kumar, Rashna Dass, Rema Devi, Sandeep Bavdekar,
Santosh Mohanty, Saradha Suresh, Shobha Sharma, Sujatha S Thyagu, Sunil
Karande, TD Sharma, Vinod Aggarwal, Zia Chaudhuri.
|
Objective: To develop and validate INCLEN Diagnostic Tool for
Attention Deficit Hyperactivity Disorder (INDT-ADHD).
Design: Diagnostic test evaluation by cross
sectional design.
Setting: Tertiary care pediatric centers.
Participants: 156 children aged 65-117 months.
Methods: After randomization, INDT-ADHD and
Connor’s 3 Parent Rating Scale (C3PS) were administered, followed by an
expert evaluation by DSM-IV-TR diagnostic criteria.
Main outcome measures: Psychometric evaluation of
diagnostic accuracy, validity (construct, criterion and convergent) and
internal consistency.
Results: INDT-ADHD had 18 items that quantified
symptoms and impairment. Attention deficit hyperactivity disorder was
identified in 57, 87 and 116 children by expert evaluation, INDT-ADHD
and C3PS, respectively. Psychometric parameters of INDT-ADHD for
differentiating attention deficit hyperactivity disorder and normal
children were: sensitivity 87.7%, specificity 97.2%, positive predictive
value 98.0% and negative predictive value 83.3%, whereas for
differentiating from other neuro-developmental disorders were 87.7%,
42.9%, 58.1% and 79.4%, respectively. Internal consistency was 0.91.
INDT-ADHD has a 4-factor structure explaining 60.4% of the variance.
Convergent validity with Conner’s Parents Rating Scale was moderate (r
=0.73, P= 0.001).
Conclusions: INDT-ADHD is suitable for diagnosing
attention deficit hyperactivity disorder in Indian children between the
ages of 6 to 9 years.
Keywords: Childhood neuro-developmental disorders, Resource
limited settings, Psychometric evaluation.
|
|
Attention Deficit Hyperactivity Disorder (ADHD) has 3-5% prevalence in
school- aged children worldwide [1,2]. The diagnosis of ADHD is purely
clinical and challenging as the developmental level and co-morbid
disorders affect manifestations. Subjectivity arises in recognition of
symptoms and degree of functional impairment. In the West, studies have
shown that ADHD can be reliably diagnosed across clinicians [3]. This
may not be true in India and other similar settings due to low levels of
awareness and expertise about ADHD in community clinicians. Clinically,
International Classification of Disease-10 (ICD-10) and the Diagnostic
and Statistical Manual of Mental Disorders-Text Revision (DSM-IV-TR)
criteria are used to diagnose ADHD [4,5]. Both constructs are based on
core symptom clusters of inattention and hyperactivity/impulsiveness.
The American Academy of Pediatrics (AAP) guidelines for ADHD assessment
advise DSM-IV-TR criteria, evaluating for co-morbid conditions, and a
neurological examination [6].
Appropriateness of construct of the DSM-IV-TR
diagnostic criteria has not been studied in the Indian cultural context.
Moreover, the uses of narrow band rating scales are limited by bias,
cost, extensive training requirement, decreased availability and poor
applicability. Some tools require the teacher’s perspective of the
child’s behavior which may not be as reliable given the high
student-teacher ratios. Appropriateness criteria are evidence-based
guidelines developed to assist physicians and clinical psychologists in
diagnosing conditions with wide variability in clinical decision in such
settings. They are created by blending broad ranges of clinical
experience with evidence-based information. The current study was
planned to develop appropriateness criteria for ADHD in Indian children
(6-9 years of age) and validate a diagnostic tool based on this
criteria.
Methods
Development of Appropriateness Criteria and Instrument
A panel consisting of 49 national experts from
different parts of India and 6 international experts (pediatricians,
child psychiatrists, pediatric neurologists, epidemiologists, pediatric
otorhinolaryngologists, clinical psychologists, special educators,
specialist nurses, speech therapist, occupational therapists and social
scientist) developed the appropriateness criteria and diagnostic tool
over three rounds of two-day workshops conducted during 2006-2008.
Diagnostic modalities of ADHD in children were reviewed, and clinical
expertise regarding personal practice was shared [7]. The former
included ICD-10, DSM-IV-TR, ADHD Comprehensive Teacher Rating Scale-2nd
edition, The Vanderbilt ADHD Teacher Rating Scale, Conner’s Parent and
Teacher Rating Scales-Revised (CPRS-R, CTRS-R), Swanson, Nolan, and
Pelham-IV Questionnaire, and Attention Deficit Disorder Evaluation
Scale-Second Edition [8-13]. A pool of items was selected by the panel
using the modified Delphi technique. Appropriateness criteria comprising
of 18 symptoms, based on parental interview and direct observation, were
finalized based on clarity, importance and frequency of endorsement. The
items were formulated in a construct similar to DSM-IV-TR criterion. The
criteria were converted into symptom clusters for clinicians and
psychologists to rate during diagnostic workup. The tool was named
"INCLEN Diagnostic Tool for Attention Deficit Hyperactivity Disorder
INDT–ADHD. The tool was translated forwards and backwards from Hindi
to English and Malayalam by bilingual translators maintaining
conceptual, content, semantic, operational and functional equivalence of
the items, and validated. The tool was similarly prepared in Odia,
Konkani, Urdu, Khasi, Gujarati and Telugu.
Section-A of INDT-ADHD consists of 18 items related
to ‘inattention’ and ‘hyperactivity/impulsiveness’ symptoms (9 items
each) while Section B consists of 8 items pertaining to onset, duration,
functional impairment and a diagnostic algorithm to arrive at the
diagnosis. Scoring is by parental endorsement with ‘1’ for ‘Yes’ and ‘0’
for ‘No’. A score of six or more of the 9 items related to ‘only
inattention’, ‘only ‘hyperactivity/impulsiveness’ and ‘both’ indicate
‘predominantly inattentive’, ‘predominantly hyperactive/impulsive’, and
‘combined subtypes’, respectively. These are considered significant if
the duration of symptom is ≥6
months, onset is before 7 years of age, and manifestation are in at
least two settings. The instrument is given as
Web Appendix I.
Psychometric Evaluation
The evaluation was conducted at four tertiary
pediatric centers [All India Institute of Medical Sciences (AIIMS),
Maulana Azad Medical College (MAMC), and Lady Hardinge Medical College
(LHMC) in New Delhi, and Child Development Centre in Thiruvananthapuram]
from June 2008 to April 2010.
Children 6-9 years of age with various
Neurodevelopmental Disorders (NDDs) were recruited from the Child
Development/Neurology outpatient clinics; those with typical development
were recruited from the pediatric outpatient departments. Informed
consent from the accompanying primary caregiver was obtained. The study
was approved by the IndiaCLEN Review Board and individual Institutional
Ethics Committees.
Enrolment and assessment
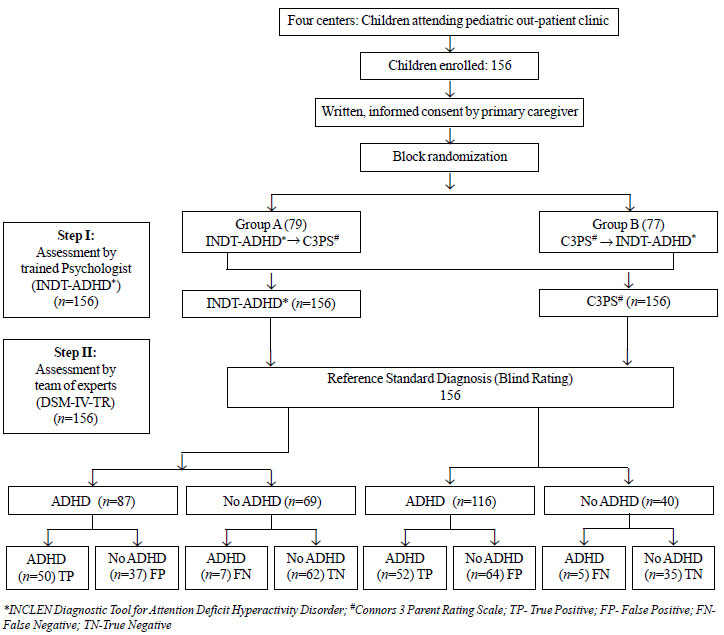
Fig.1 depicts the method for
participant selection, assessment and interview. At every study site,
the study coordinator, who was not part of any assessment, evaluated the
children attending the clinic for eligibility and enrolled them in the
study. The 156 participants were randomly allocated into group A (N=79)
or B (N=77) by block randomization. In group A, INDT-ADHD was
administered followed by Conner’s 3 Parent Rating Scale-Short Form
(C3PS) [14] whereas in group B, the sequence was reversed. This was done
by independent psychologists to minimize rating bias. Thereafter, each
child was assessed by a two member expert team (pediatric neurologist
and child psychiatrist) who based their diagnosis on DSM-IV-TR criteria.
This process took 3.5 hours over two consecutive days for each
participant, comprising of interviews and direct observations. Each
evaluator was blinded to original diagnosis and to the assessment by
each other. After the expert evaluation, parents were counselled
regarding the diagnosis and referrals were facilitated accordingly.
 |
|
Fig. 1 The flowchart for
randomization, assessment and interviews.
|
A sample size of 50 was calculated for each of the
three groups (ADHD, children with other NDDs, and with normal
development) assuming 85% sensitivity and specificity of INDT-ADHD to
diagnose ADHD and 90% precision at 95% confidence. It was decided to
enrol 60 children to account for drop-outs. This sample size was
adequate to have an exploratory factor analysis during validation.
Training: The psychologists were trained in
administration of INDT-ADHD and C3PS using a standardized operational
manual in a 3-day structured workshop. Separate groups of psychologists
were formed for INDT-ADHD and C3PS. Two pediatric neurologists and two
child psychiatrists with over 10 years of professional experience were
the trainers. Out of eight trainees, six were Masters in Psychology and
two were Clinical Psychology graduates.
Data management and analysis
Participants’ assessment details were entered in a
pre-designed instrument with unique identification numbers. Blinding was
maintained by separate opaque, sealed envelopes and protected by
reversible anonymity and restricted availability. Statistical analysis
was done using SPSS (version 19) and MedCalc (version 12.2.1.0) after
data was entered into Intelligent Character Recognition sheets (ICR).
These were processed using ABBYY Form Reader 4.0 software. Psychometric
parameters of diagnostic accuracy, construct validity, criterion
validity and internal consistency of INDT-ADHD were estimated. The
performance of INDT-ADHD was compared with C3PS for convergent validity.
Results
Mean (SD) age of enrolled children (N=156; 107
boys) was 89.1 (11.9) months. The diagnoses made by each method is
depicted in Table I. According to expert team (gold
standard), 57 children had ADHD (47 isolated and 10 with other co-morbid
NDD); 26 were predominantly inattentive, 11 predominantly
hyperactive/impulsive and 20 were combined ADHD. INDT-ADHD diagnosed
ADHD in 87 children; 33 predominantly inattentive, 16 predominantly
hyperactive/impulsive and 38 combined. C3PS made a diagnosis of ADHD in
116 cases without any differentiation into sub-types.
TABLE I Final Diagnoses of Study Group According to Experts (N=156)
|
Evaluation by |
Final Diagnosis |
|
ADHD |
Not ADHD |
|
Total |
Isolated ADHD |
With co- morbid NDD |
Total |
NDD/co morbidities |
Normal
|
|
(Break-up)* |
(Break-up)* |
(Break-up)* |
|
other than ADHD |
development |
|
Expert Team$ |
57 |
47 |
10 |
99 |
55# |
44
|
|
(26,11,20) |
(15,14,18) |
(4,3,3) |
|
|
|
|
INDT-ADHD |
87 |
Not done |
Not done
|
69 |
26 |
43
|
|
(33, 16, 38) |
by tool |
by tool |
|
|
|
|
C3PS |
116 (No sub- |
Not done |
Not done |
40 |
12 |
28
|
|
type possible) |
by tool
|
by tool |
|
|
|
|
*Inattention, hyperactivity/impulsiveness, combined.
#ASD-Autism
Spectrum Disorder; ID-Intellectual Disability; SLD-Speech and
Language Disorder; HI-Hearing Impairment; VI-Vision Impairment;
NMI-Neuro-motor Impairment; CP-Cerebral palsy; LD-Specific
Learning Disorders. INCLEN Diagnostic Tool for Attention Deficit
Hyperactivity Disorder (INDT- ADHD); Connors Parent Rating Scale
(C3PS) and Diagnostic and Statistical Manual of Mental
Disorders- IV-Text Revision (DSM-IV TR). #(ASD
-19, ASD + ID-5, ID-15, SLD- 2, HI-3/ VI-1,
NMI/CP- 3, Epilepsy -2, LD- 5); $Expert team:
diagnosis with DSM-IV-TR Diagnostic criteria of ADHD. |
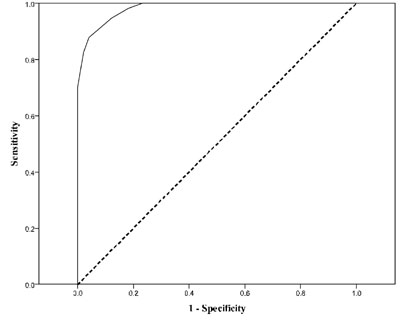
Psychometric parameters of INDT-ADHD are summarized
in Table II. The receiver operating characteristic (ROC)
curve for INDT-ADHD with a cut-off score of ≥8 against expert
diagnosis gave an Area Under the Curve (AUC) of 0.98 [95% CI0.94, 0.99)
[depicted as Fig. 2]. The diagnostic accuracy of
INDT-ADHD against expert diagnosis calculated by AUC according to
age (below and ≥7 years), gender and severity (no ADHD and ADHD)
is presented in Table III. Inter-rater reliability and
test-retest reliability were not assessed. The Cronbach’s
α coefficient
for the whole construct showed high internal consistency (0.91) and good
internal consistency separately for inattention (0.84) and
hyperactivity/impulsiveness (0.87). Construct validity was
demonstrated by exploratory factor analysis (principal component
extraction and varimax rotation). Taking the critical Eigen value as 1,
a 4-factor structure was derived [Web Table I]. Factors 1,
2, 3 and 4 represented inattention, hyperactivity, communication related
restlessness and distractibility, respectively. With loading factor cut
off level of 0.4, 14 items loaded distinctively on to single factors,
eight with inattention, three with hyperactivity, two with communication
related restlessness and one with distractibility, whereas four symptoms
cross-loaded on to more than one factor. This factor analysis explained
60.4% of the variance. When the performance of INDT-ADHD was compared
with that of C3PS it was observed that the convergent validity was
moderate (r = 0.73, P= 0.001).
 |
|
Fig. 2 The Receiver Operating Curve
characteristics of INCLEN
Diagnostic Tool for Attention Deficit Hyperactivity Disorder
(INDT-ADHD) total score against Diagnostic and Statistical
Manual of Mental Disorders- IV-Text Revision (DSM-IV-TR)
diagnosis (Expert Diagnosis).
|
TABLE II Diagnostic Accuracy of INDT-ADHD Against the Expert Diagnosis
|
Sensitivity%
(95% CI) |
Specificity%
(95% CI) |
PPV
(95% CI) |
NPV
(95% CI) |
Positive LR
(95% CI) |
Negative LR
(95% CI) |
|
ADHD vs. |
87.7 |
42.9 |
58.1 |
79.4 |
1.5 |
0.28
|
|
other NDD |
(78.6-94.2) |
(34.6-48.7) |
(52.1-62.4) |
(64.1-90.2) |
(1.2-1.8) |
(0.12-0.61) |
|
ADHD vs. |
87.7 |
97.2
|
98.0 |
83.3 |
31.5 |
0.12 |
|
normal |
(81.1-89.4) |
(86.7-99.9) |
(90.6-99.9) |
(74.3-85.6) |
(6.0-610.8) |
(0.10-0.21) |
|
INDT-ADHD |
87.7
|
95.9 |
38.2 |
11.1 |
21.7 |
0.13 |
|
total score ≥8 |
(76.3-94.9) |
(90.0- 98.9) |
(34.9-43.7) |
(0.04 - 0.2) |
(19.5-24.1) |
(0.04-0.4) |
|
INDT- ADHD: INCLEN Diagnostic Tool for Attention Deficit
Hyperactivity Disorder; Other NDD: Other Neuro-developmental
disorder; LR: Likelihood ratio; PPV: Postive predictive value;
NPV: Negative predictive value. |
TABLE III Performance of INDT-ADHD Against DSM-IV TR Different Age Groups, Gender and Severity* of ADHD
|
Groups |
AUC (95% CI)
|
|
Age group |
|
|
Children < 7 years |
0.98 (0.96-1) |
|
Children ≥7 years |
0.98 (0.96-1) |
|
Gender |
|
|
Boys |
0.97 (0.95-0.99) |
|
Girls |
0.99 (0.97-0.99) |
|
Severity of ADHD*
|
|
|
No ADHD/Borderline |
0.53 (0.42-64) |
|
Severe |
0.81 (0.69-0.93) |
|
*Severity of ADHD dichotomized into no ADHD/borderline (C3RS
score of 0-56/57-63) and elevated scores (C3RS score of
≥64); DSM-IV TR: Diagnostic and
Statistical Manual of Mental Disorder-IV- Text Revision. |
Discussion
In the present study, the diagnostic accuracy for
INDT-ADHD for ADHD was high irrespective of age and gender. Sensitivity,
specificity, positive predictive and negative predictive values were
acceptable INDT-ADHD performed well in differentiating ADHD from normal
children but could not effectively differentiate it from other NDD’s,
especially ASD.
Content validity refers to the extent to which a
measure represents all facets of a given construct. In this tool it was
inattention, hyperactivity, restlessness and distractibility. This was
ensured during tool development as only those items in which >50%
consensus was reached by the experts were considered. During validation
this was substantiated as not a single item was assigned a score of ‘0’
in > 50% of children with ADHD by expert diagnosis. Construct validity
is the degree to which a test measures what it claims to be measuring
that is assessed by factor analysis of the symptom clusters of ADHD.
Variability in factor analysis results has been observed in studies with
2-factor, 3-factor and 4-factor structures being used to explain the
construct, probably attributable to differences in study population and
statistical approach [15-17]. The 4-factor structure of INDT-ADHD is
similar to the model offered by Baumgaertel, et al. [17].
Moderate convergence of INDT-ADHD with C3PS implied that the construct
of both were theoretically related to each other. The Cronbach’s alpha
coefficient of internal consistency is in agreement with a previous
study [18].
The strength of this study was its multi-centric
development and validation. Using appropriateness criteria as diagnostic
tool has been successful previously [19]. However, validation was on a
referral center based population where the prevalence of ADHD is
expected to be high, and not representative of the general population.
The total variance explained by the 4-factor model of 60% indicates that
it could be due to missing information in the tool or a small sample
size. The former may reflect absence of inclusion of symptoms of
co-morbid disorders whereas in the latter a larger size may generate a
more stable factor structure model and improve construct validity.
The implication of this study is the creation of
qualitatively-derived and theory-guided appropriate-ness criteria-based
tool for diagnosing ADHD with high accuracy, and adequate validity and
internal consistency. It can be used for initial evaluation and
assessment of post-intervention status in ADHD. Currently available
tools for diagnosing ADHD are patented and need payment every time these
are used. The INDT-ADHD will be available in public domain and is likely
to expand diagnostic access to populations in developing countries.
Contributors: All authors have contributed,
designed and approved the study. NKA will act as a guarantor for this
work.
Funding: Ministry of Social Justice and
Empowerment (National Trust), National Institute of Health (NIH-USA);
Fogarty International Center (FIH), Autism Speaks (USA); Competing
interests: None stated.
|
What is Already Known?
• Diagnosis of ADHD
necessitates evaluation by an experienced psychologist,
psychiatrist, or developmental pediatrician.
What This Study Adds?
• The INDT-ADHD diagnostic tool for ADHD is
a freely available tool, developed for the resource limited
settings through expert consensus based on established DSM-IV-TR
criteria.
|
References
1. Polanczyk G, de Lima MS, Horta BL, Biederman J,
Rohde LA. The worldwide prevalence of ADHD: a systematic review and
metaregression analysis. Am J Psychiatry. 2007; 164:942-8.
2. Srinath S, Girimaji SC, Gururaj G, Seshadri S,
Subbakrishna DK, Bhola P, et al. Epidemiological study of child
and adolescent psychiatric disorders in urban and rural areas of
Bangalore. Indian J Med Res. 2005; 122:67-79.
3. National Institutes of Health Consensus
Development Conference Statement: Diagnosis and treatment of
attention-deficit/hyperactivity disorder (ADHD). J Am Acad Child Adolesc
Psychiatry. 2000; 39:182-93.
4. World Health Organization (WHO). The ICD-10
Classification of Mental and Behavioral Disorders: Diagnostic Criteria
for Research. Geneva: WHO; 1993.
5. American Psychiatric Association (APA). Diagnostic
and Statistical Manual of Mental Disorders. 4th ed., text rev.
DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000.
6. Dulcan M. Practice parameter for the use of
stimulant medication in the treatment of children, adolescents, and
adults. J Am Acad Child Adolesc Psychiatry. 1997; 36:85-121.
7. Howitt D, Cramer D. First Steps in Research and
Statistics: A Practical Workbook for Psychology Students. London:
Routledge; 2000.
8. Ullman RK, Sleator EK, Sprague RL. ACTeRS: Teacher
and Parent Forms Manual. Champaign, IL: Meri Tech, Inc; 1997,
9. Wolraich ML, Feurer I, Hannah JN, Pinnock TY,
Baumgaertel A. Obtaining systematic teacher report of disruptive
behavior disorders utilizing DSM-IV. J Abnorm Child Psychol. 1998;
26:141-52.
10. Conners CK, Sitarenios G, James D, Parker A,
Epstein JN. Revision and restandardization of the Conners Teacher Rating
Scale (CTRS-R): Factor structure, reliability, and criterion validity. J
Abnormal Child Psychol. 1998; 26:279-91.
11. Conners CK. Conners’ Parent Rating
Scales-Revised. New York, NY: Multi-Health Systems; 1997.
12. Swanson J, Nolan W, Pelham, WE. SNAP rating
scale. Educational Resources Information Center (ERIC); 1982.
13. Adesman AR. The Attention Deficit Disorders
Evaluation Scale. J Dev Behav Pediatr. 1991; 12:65-6.
14. Conners CK. Conners’ Rating Scales, 3rd Edition.
North Tonawanda: NY Multi-Health Systems; 2008.
15. Kanbayashi Y, Nakata Y, Fujii K, Kita M, Wada K.
ADHD-related behavior among non- referred children: parents’ ratings of
DSM-IIIR symptoms. Child Psychiatry Hum Dev. 1994; 25:13-29.
16. Baeyens D, Van DL, Danckaerts M. Validity of the
DSM-IV factor structure of ADHD in young adults. International
Eunethydis Meeting, Vrije Universiteit Amsterdam. The Netherlands 26-28
May 2010
17. Baumgaertel A, Wolraich ML, Dietrich M.
Comparison of diagnostic criteria for attention deficit disorders in a
German elementary school sample. J Am Acad Child Adolesc Psychiatry.
1995; 34:629-38.
18. Mitsis EM, McKay KE, Schulz KP, Newcorn JH,
Halperin JM. Parent–teacher concordance for DSM–IV
attention-deficit/hyperactivity disorder in a clinic-referred sample. J
Am Acad Child Adolesc Psychiatry. 2000; 39:308-13.
19. de Bosset V, Froehlich F, Rey JP, Thorens J,
Schneider C, Wietlisbach V, et al. Do explicit appropriateness
criteria enhance the diagnostic yield of colonoscopy? Endoscopy. 2002;
34:360-8.
|
|
|
 |
|

