Pediatricians are the professionals most concerned
about the well-being of the child, in addition to being a respected group
in the society. They are often the first contact of a child who has
suffered abuse. In the outpatient or casualty, whenever one comes across a
case of child abuse, chances are that the severity may often determine
whether we do suspect it or fail to recognize the subtle varieties. The
pediatrician can only recognize all such cases, when he/she considers
every child seen by him/her potentially at risk of either abuse or
neglect. Multiple studies worldwide have demonstrated that health workers
have insufficient knowledge and/or training in addressing child abuse. The
NSCA(2) also recommends that ‘good practices in protection need to be
documented/ shared for qualitative improvement at all levels’.
The Child Rights and Protection Program (CRPP), taken
up under VISION 2007 program of Indian Academy of Pediatrics, stems from
the United Nations Convention on the Rights of the Child (UNCRC)(3), and
is a major step in the history of Child Rights in India. It aims to
provide an impetus to the involvement of pediatricians in child protection
activities. As part of the CRPP, a ‘Training of Trainers (TOT) Workshop on
Child Rights and Protection’ was held on 10th and 11th January, 2007 in
Mumbai (under the aegis of Pedicon 2007, Department of Pediatrics,
LTMG Hospital, Sion, Mumbai; The Royal College of Pediatrics and Child
Health; and, Northumbria Healthcare Trust, UK). The recommendations at the
end of the workshop included: developing country-specific teaching and
training manual, to organize methodology workshop for TOT, and, formation
of Task force of IAP CRPP Programme. This task force developed a
module for ‘Training of Trainers Workshops for Pediatricians’. RCPCH
shared their protocol on ‘Response to child abuse’(4,5) and gave
permission to modify it in the Indian context. A National Consultative
Meet was held on 10th and 11th October, 2007 at New Delhi to discuss and
approve the abovementioned teaching program. Participants included
pediatricians from all parts of the country, as well as, all members of
the ‘task force’ [Annexure 1]. The program was discussed and
ratified at the meet.
Recommendations
Who is a child?
Most of the Government programs on children are still
targeted for the age group below 14 years. The UNCRC, 1989(3) defined the
child as "every human being below the age of eighteen years unless,
under the law applicable to the child, majority is attained earlier. After
the introduction of the Juvenile Justice (Care and Protection) Act, 2000
(amended 2006), for all practical purposes, a child is considered as a
person below 18 years.
Recognizing child abuse
Interviewing the child with abuse
A large proportion of children encounter abuse in their
homes itself(3). Most cases of child abuse are committed by people known
to the child and most children do not report the matter to anybody. When
abuse is suspected, the concerned doctor must try to gather a detailed
medical history from the child, if possible, and the caretakers. During
the interview process, the following points need to be considered:
• If possible, interview the child alone (separately
from the attendants).
• The interviewer must be sensitive to the child’s
possible fears and apprehension when discussing the home situation and
should tailor the interview to the child’s developmental level.
• Repetitive interviews can be problematic to the
child. The doctor concerned must gather the basic information necessary
to help make the decisions that are in best interest of the child.
• In cases of severe abuse, parents may flee with the
child, and thus it is advisable to report the case to the authorities,
prior to informing the parents of the suspected diagnosis.
• Documentation of the interview results is
essential.
• Above all, everything is to be done in the best
interest of the child.
Maintaining a professional approach with the family,
although not always easy, can facilitate the interviewing process.
Explaining the reporting process and what the parents can expect to happen
is often helpful. Non-accusatory statements should be used. The various
techniques and stages on interviewing a child with abuse are available
elsewhere(4-8).
Response of the pediatrician to child abuse
A pediatrician’s response to a case of child abuse,
either in the outpatient or inpatient settings should follow three
cardinal principles. It should be:
1. Child centered and child friendly: It
should keep the best interest of child in mind. Safety of the child is
to be considered paramount.
2. Family supportive: Response should provide
adequate support to the family as generally family forms the backbone of
the child protection system. Keeping the child permanently in an
institution is the last option in child protection.
3. According to the law of the land and safe for
the pediatrician: The management and documentation of the case
should be impeccable to avoid professional litigation later.
When a pediatrician is confronted with a suspected case
of child abuse, it is important not to jump to the diagnosis of abuse. The
basic rules to be followed include:
• To consult widely with people who know the child
well, like relatives, teachers etc., apart from parents.
• To gather information from other professionals like
the child’s regular pediatrician, the parents’ physician, especially if
the parent is suffering from mental disease, drug abuse, or other
chronic diseases.
• To check past medical records for any hospital
admissions (for child safety concerns) and developmental history.
• To document child safety concerns after a
comprehensive medical assessment.
• To make a final conclusion after discussing the
case with seniors, peers, psychologists and probably even NGOs and
social worker.
The responses of a pediatrician to a child abuse case
can be broadly classified into:
1. Urgent response is needed if the child is
brought dead or with a life threatening injury or with acute sexual
assault (reports within 24-72 hours of the abuse). The child will need
emergency care and the police would require immediate forensic samples
to book a strong case against the abuser. Such cases are best managed in
a government hospital setting.
2. Admission to the hospital is needed in all
cases of serious injuries. A child may be admitted incase it is felt
that there is an immediate threat to his safety at home.
3. Social Services like Child Welfare
Committee (CWC) and Child Helpline (Phone No.1098) or local NGOs may be
contacted if the parents refuse to follow the treatment plan or if there
is an immediate threat to safety of other sibs. CWC and Child Helpline
can also be contacted in any case where child rights are violated like
neglect, child labor, corporal punishment at school, child marriage etc.
4. Planned response is the best. Here a
planned interview and examination are performed in a child-friendly
atmosphere with the appropriate equipment and health personnel (social
worker, psychologist, gynecologist if needed). A child friendly
atmosphere is one that is sensitive to the needs of the child, where he
feels comfortable, relaxed and at ease to confide his problems.
Reporting Child Abuse
The following background information is important
before the pediatrician decides to handle a case of child abuse or
neglect:
Childline. This service, launched by the Government
of India, is a 24-hours free phone service, which can be accessed by a
child in distress or an adult on his behalf by dialing the number 1098 on
telephone. Childline provides emergency assistance to a child and
subsequently based upon the child’s need, the child is referred to an
appropriate organization for long-term follow up and care. It responds to
calls for medical assistance, shelter, repatriation, missing children,
protection from abuse, emotional support and guidance, information and
referral to services, death related calls etc.
Child Welfare Committee. Under the JJ Act, it is
possible for the Child Welfare Committee to declare any parent or
guardian; who grossly abuses a child, or fails to protect a child from
being abused, as unfit persons and order for the removal of the child from
the custody of such persons. The offences under this Act are cognizable
and the special police officer or any of his subordinate may arrest a
person without warrant and search the premises without warrant.
Mandatory reporting. Mandatory reporting mandates
certain professionals to report to appropriate authorities suspected cases
of child physical and sexual abuse. Designated professionals (including
pediatricians) are required by law to report all suspected cases of child
abuse and neglect. They are protected by law in case of an erroneous
reporting, as long as it was in good faith. They are legally penalized in
case they fail to report. Under this law, proof is not required to report,
and the only requirement is to report suspected abuse. In India, such
provisions have not yet been introduced.
Whom to Report. In the absence of ‘mandatory
reporting’ provisions and child protection services in India, this
constitutes an important decision. Usually the reporting can be done to
the Police, the local Child Welfare Committee, and even to the
Childline. However, even after reporting, networking among various
professionals is usually required to follow-up the case to its just
conclusion.
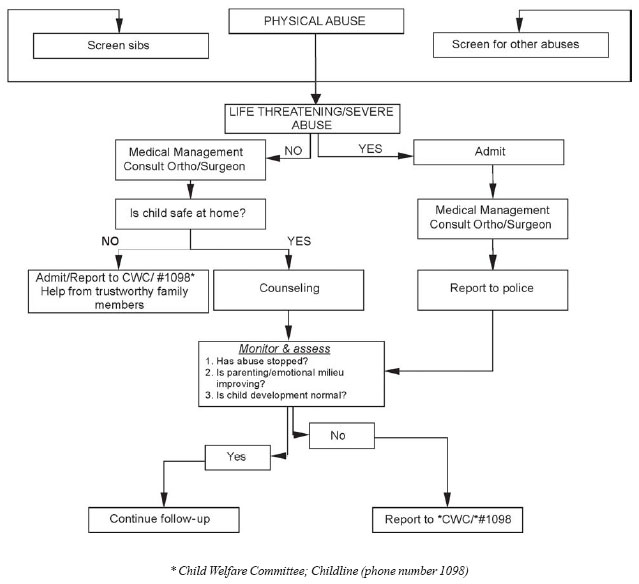
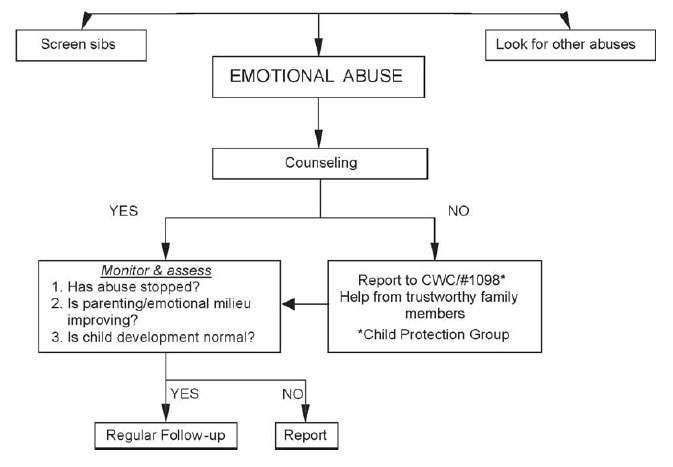
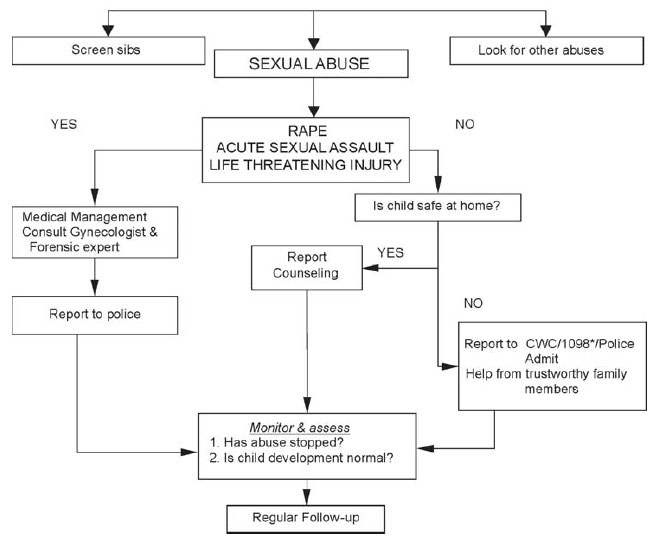
The team developed the following flow charts, based on
our discussions and on previously published material(4,5,15), which
provide suggested protocols for pediatricians to respond to physical (Fig.
1), sexual (Fig. 2), and emotional abuse (Fig.
3). Following are the important goals of a pediatrician’s response:
1. Immediate goal is to ensure safety and provide
emergency care if needed.
2. Comprehensive medical assessment including
history, examination and investigations, and documentation.
3. Short term goals include providing immediate
emotional (counseling) and social support to the child and family and
treating physical problems like injuries, providing immunization, STD
prophylaxis and emergency contraception.
4. Long term goals include complete physical and
psychosocial well being of the child. They also ensure his reintegration
into the family and social system.
 |
|
Fig. 1 Response to physical abuse. |
 |
|
Fig. 2 Response to emotional abuse. |
 |
|
Fig. 3 Response to sexual abuse. |
Comprehensive Medical management
History
1. A detailed account of the incident(s) should be
sought from both the caregiver and the child, separately. History should
be recorded verbatim. The rapport building and interviewing skills of
the examiner are of utmost importance. The examiner should observe the
behavior of the child during history-taking.
2. Presenting symptoms of the child are noted.
Physical, mental and personality development should be noted.
3. Family and Social history should be taken with
details about the marital status of parents, whether the family is a
broken or dysfunctional one, total number of members in the family,
interpersonal conflicts and social interaction among various family
members, etc.
4. Social history includes employment details of
parents, their age, education and physical and mental maturity, nature
of parent-child relationship, any concerns about profession, health,
education, etc.
5. Sexual history of victim about exploitation or
abuse should be obtained. Presence of addictions such as alcohol, drugs
and tobacco should be noted. The recorded information should include the
relation of the victim with the accused and exploiter, age difference of
accused and victim and other relevant information.
The presence of a chaperone, preferably a nurse is a
must during the assessment. The assessment should be recorded in a special
proforma. History-taking from the parent or caretaker should be documented
separately from that of the child. Repeated interviews are to be avoided.
• It is important to treat the child and the parents
with respect and dignity without making accusations.
• Listen carefully and have a sensitive, empathic and
nonjudgmental attitude.
• Ask open-ended and non-leading questions.
• Nonverbal cues as ‘watchful frozenness’, sad mood,
avoidance of eye contact, etc. should be recorded. Exact question and
answers need to be recorded verbatim.
• Points to be covered in history include place,
time, witness, present and past history, noticeable behavior change,
developmental and immunization history. Family history, pedigree chart
and social history are extremely important. A psychosocial history known
by the acronym HEEADDSS (details of home, education, eating behavior,
activities and peers, drugs, depression, suicide, sexual history and
sleep pattern) can be taken directly from an adolescent patient.
Examination
Examination of victims of abuse and neglect follows the
same basic principles as examination for any other medical condition, but
requires an expertise which accrues from training and regular updating.
There are many standard works on the examination of the abused
child(4,5,8-10), where a detailed discussion is available. Parental and
(preferably) the child’s consent are essential for a medical examination.
The child may prefer to get examined by a doctor of the same sex. He may
also choose to have a trustworthy adult along with him during the
procedure. The pediatrician may seek the expertise of a forensic physician
and a gynecologist (for a female child) while examining a case of sexual
abuse. The following should be recorded:
• Resistance to examination, especially in a case of
sexual abuse and/or, dissociation (going to sleep during examination)
• General demeanor (like unkempt appearance in
neglect)
• Vitals and head-to-toe general physical
examination, especially noting pallor, bruises, vitamin deficiencies
(and malnutrition), sequelae of unexplained trauma, etc.
• Height, weight and head circumference to be plotted
on growth chart
• Sexual Maturity Rating for adolescents
• All injuries are to be marked on anatomical
diagrams. Special sites to look for injuries include ears, inside the
mouth, soles, genitalia and anus.
• Systemic examination is done, especially to look
for injuries.
• Examination of genitalia in girls should be done in
supine (frog leg), prone (knee chest) and left lateral position. Details
of hymen and injuries are to be noted. Anal dilatation on per rectal
examination may indicate sodomy, and must be documented. Presence of
discharge, genital ulcers, warts and inguinal lymphadenopathy are to be
noted and, samples preserved in appropriate manner for forensic
evaluation.
It is important to know that in 70-85% of documented
sexual abuse, the physical examination is normal.
Investigations
The correct age of the child should be established for
any case that is going to be reported and is a must in case of a
trafficked child. Other investigations which need to be done:
• Child sexual abuse: STD screening, including low
and high vaginal (in post pubertal girls) swabs and urethral swabs in
boys, and serology for HIV, hepatitis B and syphilis are done in cases
of acute sexual assault, penetrative abuse, vaginal/ urethral discharge
and, STD in abuser. Pregnancy test should be done in an adolescent girl.
Forensic samples maintaining the chain of evidence include skin, hair,
nail clippings, clothing, saliva, and, oral and genitourinary secretions
in acute sexual assault(11).
• Physical abuse: Skeletal survey is done in a case
of multiple injuries, and in all cases if a child is below 2 years.
Multiple bruising entails a detailed hematological profile, including
bleeding and coagulation profile. Neuroimaging and ultrasonography of
abdomen are indicated in a case of head and abdominal injury,
respectively.
Management
Management should be child friendly and should aim at
achieving the short term and long term goals. The current and future plans
of action should be discussed with the non-offending family members. The
need for breaking immediate contact with the abuser, if he/she is a known
person, should be emphasized.
The physical injuries should be treated. Hepatitis B
vaccination should be considered if the sexually abused child is not
vaccinated, and if the child presents within six weeks of the last assault
(schedule 0, 1, 2, 12)(12). DPT/ DT vaccination should be given in
unvaccinated children. Tetanus immunization status should be confirmed and
updated, if necessary. Overall, the risk of acquiring a STD is low and
varies according to many factors(13). STD prophylaxis and emergency
contraception is to be given to an adolescent with acute sexual assault.
STD prophylaxis should be offered in cases of oral-genital,
genital-genital, or anal-genital contact by the abuser. HIV prophylaxis
may be indicated in specific cases(12,13); it should be considered for
every case that presents within 72 hours of the most recent abuse, if
unprotected anogenital penetration has occurred, taking into consideration
risk factors(12). All children of the family should be screened for abuse
if the abuser is close to the family. Multiple types of abuses may coexist
in the same patient and should be specifically looked for and managed.
Injuries should be treated as needed. Lacerations extending into the
vagina are not common and should be assessed by a gynecologist, as the
full extent of the laceration must be determined. The vaginal wall is
extremely thin in the prepubescent child and may be perforated more easily
than in the older child(13).
Counseling of the child and family forms the
cornerstone of the management. The immediate counseling of the child that
can be done by the pediatrician should focus on the following:
• Believe the child, reassure and absolve feelings
of guilt/ blame
• Explain about the existence of a medical, family
and social support system.
• Listen carefully to all fears and concerns
associated with disclosure.
• Teach coping and assertive skills.
Referrals to appropriate specialties should be made
according to the need of the child. These will include psychologist,
psychiatrist, orthopedic surgeon, surgeon, social services and police. The
family members may also need counseling and treatment from mental health
professionals.
Follow up
Follow up after 2 weeks, or earlier if necessary, is
essential to reassess the child and evaluate for development of sequelae.
In acute sexual assault of an adolescent girl, a repeat pregnancy test is
warranted. A repeat serology for syphilis at 4-6 weeks and for HIV at 3-6
months is required.
The long term after-effects of abuse on the physical
and mental health are well known, but some children suffer no adverse
consequences. The outcome is influenced by the following factors: nature,
extent and type of abuse, age of child, temperament and resilience of the
child, relationship of abuser to the child, and family’s response to abuse
and medical management. A single episode of non-contact sexual abuse by a
stranger may just need reassurance and letting out feelings in one or two
counseling sessions with a good outcome. But prolonged abuse by a close
family member will require longer and multiple counseling sessions to heal
completely.
Regular follow up of the abused children should include
the following: To verify if abuse has stopped, to monitor physical and
mental health, To monitor development and ensure that it is normal, and to
refer for therapy (counseling, cognitive behavior therapy or medication)
for delayed presentation of symptoms.
The key points to be kept in mind while making
decisions in the existing framework of child protection services include:
1. Seriousness of abuse: Serious abuse requires
urgent intervention and long term follow up
2. Safety of the child: If the child is not safe at
home, help from non-offending family members for a change in residence
is sought for. CWC, Child Helpline and local NGOs may also help in this
situation. If the home continues to be unsafe, safer options like foster
care and adoption of the child need to be considered.
3. Importance of counseling and follow up of the
child are important issues. Counseling of the parents, if they are the
abusers, is also necessary. All abuse, especially sexual abuse, needs to
be reported to the police.
The pediatrician’s response must always be in
accordance with the existing law of the country, as highlighted in these
guidelines.
Medico-legal aspects, Documentation and Reporting
Most victims of obvious child abuse are directly
brought to hospitals (usually Government hospitals) for medical
examination by the police. They may be accompanied by Social worker (NGO),
but at times are brought by parents / guardians. At other times, there may
be incidental recognition of child abuse during consultation for an
unrelated medical problem, which can occur in any type of setting.
Guidelines are available for documentation and may be used or adapted
depending on local settings(11).
All consultations with the patient should be in hand
written notes, with diagrams, body charts, and if possible, photographic
documentation. It should be understood that both, age determination and
complete examination requires multidisciplinary references. Their opinions
either in person or telephonically, should be recorded. Time, date,
signature, designation and additional comments, wherever appropriate, are
a must for enabling the due process of law.
The examining doctor should make sure that important
details are not omitted. All aspects of consultation should be documented
and detailed notes must be made during the consultation, patient’s records
have to be kept strictly confidential and stored securely. The
documentation should be confined to areas of health care expertise only;
interpretation of the same has to be done by a trained person if the
examining Medical Officer is not trained in examination of medicolegal
cases. Consent should always be taken in writing, and preferably from both
the guardian and the victim. All documents should be preserved for, as
yet, an undetermined amount of time.
Steps of medical examination
• Documentation should be accurate, impartial,
objective and scientific.
• After obtaining written consent, the preliminary
data should be noted including the FIR No., date and time and place of
examination, witnesses present during examination and recording, details
of informant and relation with the child.
• Demographic information, brief History and an
account of Assault should be taken.
• Examination of clothes of victim for semen stains,
struggle tears, trace material etc. should be done.
• Genitalia examination and photography (if needed)
should be taken.
• Findings of general physical examination, systemic
examination, exam for injuries, clinical/ forensic (STD, pregnancy, etc)
should be recorded.
• Examination for age determination (if needed) is a
must in a trafficking case. Age determination involves multidisciplinary
approach. The age range provided should be as narrow as possible.
The examining doctor must express opinion about
physical/sexual abuse/age determination. Treatment should be administered,
as per need. The examining doctor should be liberal in taking second
opinion, and taking references from specialists in other faculties, as
required.
Reporting by medical officer
The medical officer should not try to be an
investigator. His duty is to the court and not to either party.
1. The report should be written clearly and precisely
and should state clearly fact and medical opinion. The Court relies on
objectivity, competence and integrity. Hence the medical officer should
be balanced and accurate, report without exaggerations, and limit the
report to facts.
2. The opinion must have components of injury, sexual
activity and age estimation if required, and must consider whether there
is sexual abuse or not, acute and chronic effect on victims body and
mind, and whether proper samples have been collected for identification.
3. Positives and negatives should be included in the
report. The medical officer should not mislead by omission and should
avoid making generalizations.
4. Age determination is a must in trafficking cases.
5. The report should be reviewed and, if necessary, a
peer review should be obtained before handing it over. Premature opinion
should not be given.
Media and Child Abuse
The fundamental guideline for the media with regard to
reporting on child abuse is to protect the identity of the child. The JJ
Act, 2000; the Immoral Traffic Prevention Act, 1956; and, the Criminal
Procedure Code prohibit the disclosing of the identity of victims. Press
Council Act has also laid down the norms to be followed by the media,
keeping in mind the rights of children.
Advise to Caregivers of an Abused Child
If a child discloses that he/she has been sexually
abused or exploited:
· Support the child and explain that he/she is not
responsible for what happened.
• Believe the child and don’t make her/him feel
guilty about the abuse.
• Be empathetic, understanding and supportive.
• Consult a doctor and consider the need for
counseling or therapy for the child.
• Don’t criticize the child or get angry with
her/him.
• Don’t panic or overreact, with your help and
support, the child can make it through this difficult time.
• Don’t ignore the abuse. Voice your fears to
responsible NGOs or individuals.
• Lodge a complaint with the police and ensure that
the abuse stops immediately.
Guardians should be made to understand that their first
responsibility is to the child – to protect him/her and to ensure that
there is no breach of privacy or confidentiality.
Conclusions
These guidelines detail suggested actions to be taken
after suspecting child abuse and neglect. Many of the details of
examination and interviewing are already available in standard texts and
have not been detailed here. We plan to review the guidelines as and when
further changes in the laws dealing with age of child and, child abuse and
neglect occur.
Acknowledgments
The IAP Child Rights and Protection Program was
launched by Dr Naveen Thacker during his tenure as IAP President 2007. We
are thankful to Dr U. Bodhankar, chairperson of the initial ToT at Mumbai.
We acknowledge the support of – Dr Michael Webb, RCPCH Overseas Director
(South Asia), Department of Paediatrics, Gloucestershire Royal Hospital,
Gloucester, UK: for permission to adapt the RCPCH training material by
modifying it in the Indian context; Dr Neela Shabde, Consultant
Pediatrician and lead for RCPCH Safeguarding Children Level 2 Project, UK:
for helping us to adapt the material in the Indian context; Ms Victoria
Rialp, Chief, Child Protection, UNICEF: for the support of UNICEF to fund
this project; Dr Loveleen Kacker, Joint Secretary, Child Welfare, Ministry
of Women and Child Development and, Mrs Shantha Sinha, Chairperson,
National Commission for Protection of Child Rights: for their support. We
also acknowledge the help received from the invited experts: Rajeev
Awasthi, Criminal lawyer, Delhi, and Dr Gaurav Agarwal, Department of
Forensic Medicine, Safdarjung Hospital, Delhi.
1. Report of the Consultation on Child Abuse
Prevention, 29-31 March 1999, WHO, Geneva. Geneva, World Health
Organization, 1999 (document WHO/HSC/PVI/99.1). Available from http://whqlibdoc.who.int/hq/1999/aaa00302.pdf.
Accessed on 22 November, 2009.
2. Study on Child Abuse: India 2007. Ministry of Women
& Child Development, Government of India, Delhi, 2007. Available from
http://wcd.nic.in/childabuse.pdf. Accessed on 21 November, 2009.
3. Convention on the Rights of the Child. United
Nations Children’s Fund. Delhi, 2004.
4. Child Protection Companion. 1st Edition, RCPCH,
London, 2006. Available on http:// www.rcpch.ac.uk/Education/Education-Courses-and-Programmes/Safeguarding-Children.
Accessed on 21 November, 2009.
5. Child Protection Reader. 1st edition, RCPCH, London,
2007. Available on http:// www.rcpch.ac.uk/Education/Education-Courses-and-Programmes/Safeguarding-Children.
Accessed on 21 November, 2009.
6. Agarwal K, Dalwai S, Galagali P, Mishra D, Prasad C,
Thadani A. Manual on recognition and response to child abuse-the Indian
scenario. Indian Academy of Pediatrics - Child Rights and Protection
Programme (CRPP), Delhi, 2007.
7. Safeguarding children: Recognition and response in
child protection. RCPCH Trainer CD ROM, 2006, London, 1st edition.
8. DGH de Silva, CJ Hobbs. Managing Child Abuse. A
Handbook for Medical Officers. WHO SEARO, Delhi, 2004.
9. Kellog N. Evaluation of suspected child abuse and
neglect. AAP Policy statement. Pediatrics 2007; 119: 1232-1241.
10. Kellog N. Evaluation of sexual abuse in children.
AAP Policy statement. Pediatrics 2005; 116: 506-512.
11. Manual for Medical Officers. Dealing with Child
Victims of Trafficking and Commercial Sexual Exploitation. Department of
Women and Child Development, Government of India, New Delhi, 2007.
Available from URL: http://wcd.nic.in/ManualMedicalOfficers.pdf. Accessed
on 21 November, 2009.
12. The Physical Signs of Child Sexual Abuse – An
Evidence-based Review and Guidance for Best Practice. Royal College of
Paediatrics and Child Health, London, 2008.p.146-147. Also available from
URL: http://www.rcpch.ac.uk/Research/CE/RCPCH-guidelines.
13. American Academy of Pediatrics. Sexually
transmitted infections in adolescents and children. In: Pickering
LK, Baker CJ, Long SS, McMillan JA, eds. Red Book: 2006 Report of the
Committee on Infectious Diseases. 27th ed. Elk Grove Village, IL:
American Academy of Pediatrics; 2006.p. 166-177.
14. Resource Book. First National Conference on Child
Abuse for Multidisciplinary Professionals (COCAMP 2004). Indian Council
for Child Welfare, Tamil Nadu and Sri Ramchandra Medical College and
Research Institute, Chennai: February 2004.
15. CJ Hobbs, JM Wynne, HGI Hanks. Child abuse and
social aspects of pediatrics. In: N McIntosh, PJ Helms, RL Smyth,
Eds. Forfar and Arneil’s Textbook of Pediatrics, 6

