|
|
|
Indian Pediatr 2016;53: 627-629 |
 |
Rotavirus
Diarrhea in Children Presenting to an Urban Hospital in Western
Uttar Pradesh, India
|
|
Neeraj Teotia, Amit Upadhyay, Sunny Agarwal,
#Amit Garg and *Dheeraj
Shah
From Department of Pediatrics and #Microbiology,
LLRM Medical College, Meerut, UP; and *Department of Pediatrics,
University College of Medical Sciences and GTB Hospital, New Delhi;
India.
Correspondence to: Dr Neeraj Kumar Teotia, Department
of Pediatrics, LLRM Medical College, Meerut, UP, India.
Email: [email protected]
Received: January 02, 2014;
Initial review: January 27, 2014;
Accepted: April 27, 2015
|
Objective: To determine the proportion and clinical profile of
rotavirus-associated diarrhea in children aged 6 months to 5 years.
Methods: Clinical details and stool samples were
collected from 254 children aged between 6 months to 5 years
presenting with acute diarrhea, irrespective of hydration status, to the
outpatient department or emergency room of a hospital in Meerut, Uttar
Pradesh, India.
Results: Rotavirus accounted for 26.3% (51 of
194) of diarrhea cases overall, and 41.2% (14 of 34) in hospitalized
children. Rotavirus infection was associated with significantly longer
duration [3.3 (1.4) d vs. 2.5 (1.1) d; P=0.004) of
diarrhea, and more chances of dehydration (OR 1.85; 95% CI 1.19, 3.57)
as compared to non-rotavirus diarrhea.
Conclusion: Rotavirus is a common cause of acute
diarrhea in under-five children, and is associated with a longer
duration and more chances of dehydration than non-rotavirus diarrhea.
Keywords: Acute diarrhea, Epidemiology, Etiology.
|
|
Rotavirus is a common cause of diarrhea in
children below 5 years of age, and is estimated to cause 4.4% and 3.2%
of deaths worldwide in children in age group below one year and 1-4
years, respectively [1]. India has estimated annual burden of 2.0-3.4
billion cases attributable to rotavirus [2]. A rising trend in
proportion of rotavirus cases in hospitalized children has been
reported; 26.1% before 2000 to 38.3% after 2005 [3]. A recent
multi-centric surveillance study in India reported 39% prevalence of
rotavirus in children below five years of age hospitalized for acute
diarrhea [4]. World Health Organization (WHO) estimated that State of
Uttar Pradesh (UP) in India accounts for 32% of diarrheal deaths due to
rotavirus infection among Indian children younger than five years [5].
As UP was not included in rotavirus multi-centric surveillance study, it
is pertinent to collect information related to rotavirus diarrhea from
this region. The present study was designed to estimate the proportion
of rotavirus diarrhea in children presenting with acute diarrhea, and to
study its clinical profile.
Methods
This descriptive study was conducted in the
Department of Pediatrics, LLRM Medical College, Meerut, UP, India from
July 2011 to June 2012. Children aged between 6 months to 5 years
presenting with acute diarrhea (<7 days duration), irrespective of
hydration status, to the outpatient department (OPD) or emergency room
of hospital were eligible for inclusion. Diarrhea was defined as passage
of three or more loose stools in the last 24 hours [6]. Children with
severe malnutrition (weight-for-height <-3 SD of WHO charts), dysentery
and clinical evidence of coexisting acute or chronic systemic illnesses
were excluded from the study. Written informed consent was obtained from
parents of children enrolled in the study.
All children were managed according to their
dehydration status, as per WHO guidelines [6]. Children were monitored
for number of loose stools, consistency of stool and time since last
loose stool every six hours in a day. Children admitted in emergency
ward were monitored directly by doctor on duty. Those who were enrolled
on outpatient basis were contacted telephonically till diarrhea
resolved, or for a period of 7 days after enrolment, whichever was
earlier.
Stool samples of enrolled children were collected in
sterile screw-top container, and were stored at -20° C till testing.
Rotavirus detection was done only in children who completed the 7-day
follow-up. Samples were transported to Microbiology department of our
hospital in vaccine carrier; rotavirus detection was done by ELISA using
Rota IDEIA Kit (DAKO, Germany).
Data were entered in the Microsoft Excel worksheet
and were analyzed using SPSS Version 17.0.
Results
Over a 12-month period, 516 children (444 OPD and 72
Emergency services) with acute diarrhea presented to the hospital, out
of which 254 eligible children were enrolled in the study. Among
included patients, 170 patients were also part of another study to
determine the effect of probiotics on acute childhood diarrhea [7].
Stool sample analysis for rotavirus could be done only for 194 patients;
165 (85.1%) were enrolled from OPD and 29 (14.9%) from the emergency
(overnight hospital stay). The mean (SD) age was 19.1 (13.5) months, and
children aged 6-23 months accounted for 79.5% of all included children.
Some dehydration was seen in 40.7%, severe hydration in 5.1% and
vomiting in 37.8% of participants. Thirty-six (14.6%) children required
intravenous fluids for dehydration correction, and one child died 6
hours after admission in emergency services. None of the included
children was vaccinated with rotavirus vaccine.
 |
|
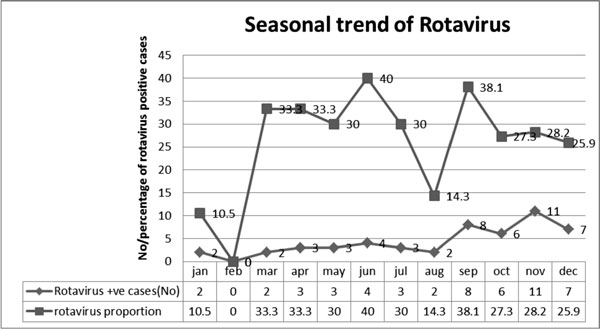
Fig. 1 Month-wise rotavirus positivity
in study children.
|
Rotavirus was detected in 51 out of 194 (26.3%)
children with acute diarrhea. Fig. 1 depicts the
month-wise detection of rotavirus antigen in study children. Among
hospitalized children, rotavirus was detected in 14 out of 34 (41.2%).
Most (82.3%) rotavirus-positive cases occurred in the age group of 6–23
months. Rotavirus positivity rate did not differ significantly by sex
(34.7% among boys vs. 24.3% among girls). Table I
compares clinical profile of diarrhea in children with rotavirus
positive and rotavirus negative status. Children with rotavirus diarrhea
had a longer duration of diarrhea and were more likely to be dehydrated
than those with rotavirus-negative disease [dehydrated (56.8%) vs.
non- dehydrated (43.2%); OR 1.85; 95% CI 1.19, 3.57; P=0.021].
Fever was observed in 72.5% (37 of 51) children with rotavirus diarrhea
and 48.9% (70 of 143) without rotavirus diarrhea.
TABLE I Clinical Profile of Children with Rotavirus Diarrhea
|
Variable |
Rotavirus positive |
Rotavirus negative |
P value |
OR (95% CI) |
|
Age < 2 y |
42 (82.3) |
94 (65.7) |
0.02 |
2.41 (1.10, 5.26) |
|
Winter season (Nov-Feb) |
26 (50.9) |
69 (48.3) |
0.89 |
1.11 (0.48, 2.20) |
|
Fever |
37 (72.5) |
70 (48.9) |
0.004 |
2.75 (1.37, 5.53) |
|
Dehydrated |
29 (56.9) |
56 (42.0) |
0.02 |
1.85 (1.19, 3.57) |
|
#Loose stools per day |
9.8 (2.1) |
9.6 (2.2) |
0.83 |
0.33 (-0.44, 0.93)* |
|
#Duration of hospital stay (h) |
76.1(27.7) |
76.5 (17.7) |
0.97 |
-0.36 (-16.19, 15.48)* |
|
#Duration of diarrhea at time of enrolment (d) |
3.3 (1.4) |
2.5 (1.1) |
0.004 |
1.25 (0.90-1.64) |
|
#Total duration of diarrhea (d) |
6.3 (1.6) |
5.3 (1.4) |
0.02 |
1.55 (1.09, 2.00)* |
|
Data in No. (%) or #Mean (SD); *Mean difference (95% CI). |
Discussion
Rotavirus infection is the most common cause of
severe gastroenteritis in children below five years of age in most
regions of India [8-10]. The present study demonstrated that rotavirus
accounts for approximately one-fourth of acute diarrhea among children
presenting to hospital below 5 years of age. The proportion was higher
(41.2%) in hospitalized children, and those with rotavirus diarrhea had
a longer duration of diarrhea and were more likely to be dehydrated.
Kang, et al. [2] detected rotavirus in 39%
cases in Indian multi-centric surveillance whereas Bahl, et al.
[8] reported 23.5% positivity rate in children below 5 years,
hospitalized for acute diarrhea. A review of 46 epidemiological studies
reported rotavirus in 20% of children hospitalized for acute diarrhea
[10]. The difference observed between our study and previous studies may
be attributed to variation in enrolment criteria among the studies, and
inclusion of outpatient children in our study. Like previous studies
[2,11], we also found more dehydration and longer duration of diarrhea
in rotavirus-positive children.
Main limitations of our study were hospital-based
enrolment and absence of asymptomatic control group. Rotavirus detection
was done only in children completing the follow-up, which might have
affected the calculation of the correct positivity rate. Also, we did
not look for other etiological agents causing diarrhea. A recent study
from Kolkata reported that 57.8% cases positive for rotavirus were
co-infected with other pathogens.
We conclude that rotavirus is responsible for about
one-fourth of childhood diarrhea under age of five years, and is
associated with significant risk of dehydration and prolonged diarrhea.
Contributors: AU and DS: conceived and designed
the study and revised the manuscript for important intellectual content;
NT, SA collected the data and drafted the paper; DS: analyzed the data
and provided critical review for revision of manuscript; AG performed
the laboratory work, and provided critical inputs. The final manuscript
was approved by all authors.
Funding: None; Competing interest: None
stated.
References
1. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K,
Aboyans V, et al. Global and regional mortality from 235 causes
of death for 20 age groups in 1990 and 2010: A systematic analysis for
the Global Burden of Disease Study 2010. Lancet. 2012;380:2095-128.
2. Tate JE, Chitambar S, Esposito DH, Sarkar R,
Gladstone B, Ramani S, et al. Disease and economic burden of
rotavirus diarrhoea in India. Vaccine. 2009;27:18-24.
3. Kahn G, Fitzwater S, Tate J, Kang G, Ganguly N,
Nair G, et al. Epidemiology and prospects for prevention of
rotavirus disease in India. Indian Pediatr. 2012;49: 467-74.
4. Kang G, Arora R, Chitambar SD, Deshpande J, Gupte
MD, Kulkarni M, et al. Multicenter, hospital-based surveillance
of rotavirus disease and strains among Indian children aged <5 years. J
Infect Dis. 2009;200:147-53.
5. Morris SK, Awasthi S, Khera A, Bassani DG, Kang
G, Parashar UD, et al. Rotavirus mortality in India: Estimates
based on a nationally representative survey of diarrhoeal deaths. Bull
World Health Organ. 2012;90: 720-7.
6. Arora NK, Das MK, Mathur P. Diseases of
Gastrointestinal Tract and Liver. In: Ghai OP, Paul VK, Bagga A,
editors. Ghai Essential Pediatrics. 7th ed. Delhi: CBS
Publishers; 2009. p. 251-95.
7. Aggarwal S, Upadhyay A, Shah D, Teotia N, Agarwal
A, Jaiswal V. Lactobacillus GG for treatment of acute childhood
diarrhoea: An open labelled, randomized controlled trial. Indian J Med
Res. 2014;139:379-85.
8. Bahl R, Ray P, Subodh S, Shambharkar P, Saxena M,
Parashar U, et al. Incidence of severe rotavirus diarrhea in New
Delhi, India, and G and P types of infecting strains. J Infect Dis.
2005;192:114-9.
9. Banerjee I, Ramani S, Primrose B, Moses P,
Iturriza-Gomara M, Gray JJ, et al. Comparative study of the
epidemiology of rotavirus in children from a community-based birth
cohort and a hospital in South India. J Clin Microbiol. 2006;44:2468-74.
10. Ramani S, Kang G. Burden of disease and molecular
epidemiology of group A rotavirus infections in India. Indian J Med Res.
2007;125:619-32.
11. Gladstone BP, Ramani S, Mukhopadhya I, Muliyil J,
Sarkar R, Rehman AM, et al. Protective effect of natural
rotavirus infection in an Indian birth cohort. N Engl J Med.
2011;365:337-46.
|
|
|
 |
|

