A
llergic rhinitis is the most
common respiratory disorder in most countries of the world. It is
estimated that 600 million people suffer from this condition. ISAAC
study [1] reports prevalence up to 40%. 80% of children with
bronchial asthma have associated allergic rhinitis and 30% of
children with allergic rhinitis develop asthma later [2]. Reports
from India shows that 1 out of every 6 person has allergic rhinitis
[3]. Although a cause of significant widespread morbidity, allergic
rhinitis is often viewed rather erroneously as trivial disease. It
may significantly affect the Quality of Life (QOL) of the child by
causing fatigue, headache, cognitive impairment and other associated
symptoms. Allergic rhinitis may be associated with many comorbid
conditions like conjunctivitis, pharyngitis, sinusitis, asthma,
eczema, otitis media, lymphoid hyperplasia, obstructive sleep apnea,
speech impairment, failure to thrive, reduced quality of life,
family disruption and impaired sexual quality of life in adults.
This module is prepared with an objective to provide practicing
doctors the evidence based approach, by reviewing the data in
medical literature as per ARIA [allergic rhinitis impact on asthma]
Guidelines and to suit our needs .
Clinical Features
Allergic rhinitis is defined as a symptomatic
disorder of nose induced by IgE mediated inflammation, after
allergen exposure of the nasal mucous membrane. It is a condition
manifested by nasal blockage, rhinorrhea, sneezing, and itching; any
2 of the above 4 symptoms must be present for >1 hr every day for >2
weeks to diagnose allergic rhinitis. Also there has to be some
associated symptoms such as facial pain, loss of sense of smell, and
postnasal drip. Some individuals may develop sinus infection and
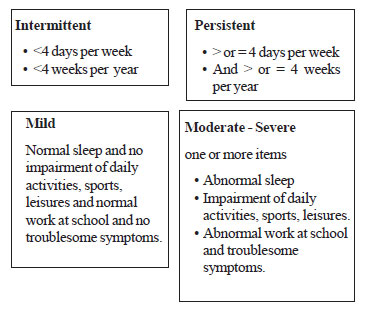
disturbed sleep as well. Severity is classified as shown in
Fig.1.
 |
|
Fig. 1 ARIA classification of
allergic rhinitis. |
Nasal Examination
A careful external and internal examination of
nose is essential in diagnosing allergic rhinitis.
1. A deviated nasal septum can sometimes be
apparent externally.
2. Gross nasal polyps can produce expansion of
nasal bones.
3. A horizontal crease above the tip of the
nose called ‘Darrier’s Line’ is characteristic feature of marked
allergic rhinitis. The Darrier’s line is caused by the patient
persistently rubbing the nose from below upwards with the palm of
the hand.
4. ‘Allergic salute’ is done to relieve itching
and free edematous turbinates from the septum.
5. The patient may exhibit facial grimaces like
nose wrinkling and mouth wrinkling which relieves the nasal
itching of the rhinitis (allergic mannerism).
6. With the worsening of symptoms, many
children may develop bluish-black discolorations under the lower
eye lids which are termed ‘allergic shiners’. These discolorations
are caused by venous stasis in the areolar tissue of the lower
palpebral grooves from pressure on veins by edematous allergic
mucous membranes of the nasal and paranasal cavities.
7. An internal examination using a simple nasal
speculum can show an anterior deviation of the septum, narrowing
of the nasal valve and inferior turbinate hypertrophy.
8. Nasal polyps can easily be confused with
swollen inferior turbinates. Nasal polyps are non-tender and
greyish, whereas swollen turbinates are tender and pale purple or
pink.
Management
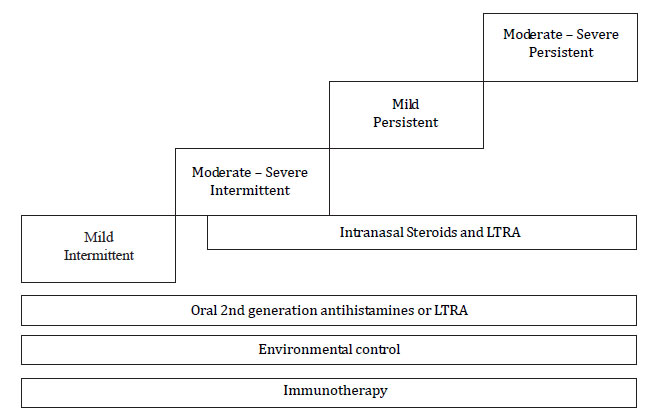
Allergic rhinitis is mainly a clinical diagnosis
and management is mainly four fold: environmental control,
pharmacotherapy, treatment of co-morbid conditions; and
immunotherapy (Fig.2). Recognizing allergy triggers
and avoiding them is the first step towards controlling allergic
symptoms. Avoid allergic triggers like dust mite, pollen grain,
animal dander, cockroach, moulds, cold air, cigarette smoke,
firewood smoke, mosquito coils, etc.
 |
|
Fig. 2 Treatment of allergic rhinitis
(ARIA guidelines). LTRA: leukotriene release inhibitor. |
1. Second generation antihistamines:
It should be prescribed due to their favorable efficacy and
safety rate. SGA have greater selectivity for peripheral H1
receptors. It has anti-allergic effect independent of action at
histamine receptors and long term treatment with SGA is safe.
Drugs used are cetrizine, levocetrizine, fexofenadine and
loratidine.
2. Intranasal steroids: INS are
the first line drug for treatment of moderate to severe allergic
rhinitis. It is the most efficacious medication available and it
can improve all symptoms of allergic rhinitis as well as allergic
conjunctivitis. Quality of life is better compared to
antihistamines. Main INS are budesonide, beclomethasone,
fluticosone propionate and mometasone.
3. Anti-leukotrienes (monteleukast):
It is indicated in seasonal allergic rhinitis, pre school
children and allergic rhinitis associated with other comorbid
conditions like asthma and conjunctivitis. Although combinations
of antihistamines with monteleukast are beneficial in several
studies, it is not recommended.
We conducted a national TOT at Jaipur, Zonal TOTs
at Chennai, Mumbai and Hyderabad following which we are planning to
have 35 workshops throughout the country. I thank the National
Coordinator, Dr H Paramesh and National Convener, Dr Major K
Nagaraju for the help and guidance to implement this program.
References
1. The International Study of Asthma and
Allergies in Childhood. ISSAC Steering Committee Worldwide
variations in prevalence of asthma, allergic rhinoconjunctivitis and
atopic eczema. Lancet. 1998;351:1225-32.
2. Allergic rhinitis and its impact on asthma.
ARIA Guidelines. 1999. Available at http://www.whiar.com. Accessed
May 28, 2011.
3. Shaikh WA. Allergic rhinitis; allergy and asthma: a tropical
view. New Delhi: IJCP Publication; 2001.

