|
|
|
Indian Pediatr
2018;55:31-34 |
 |
Celiac Disease in
Children with Moderate-to-Severe Iron-deficiency Anemia
|
|
Manish Narang
1,
Ravikumar Natarajan1,
Dheeraj Shah1,
Amarender Singh Puri2,
Vikas Manchanda3
and Mrinalini Kotru4
From 1Division of Pediatric Gastroenterology,
Department of Pediatrics and 4Department of Pathology,University College
of Medical Sciences and GTB Hospital; 2Department of Gastroenterology,
GB Pant Institute of Post Graduate Medical Education and Research;and
3Department of Clinical Microbiology and Infectious Diseases, Chacha
Nehru Bal Chikitsalaya; Delhi, India
Correspondence to: Dr Manish Narang, Professor,
Department of Pediatrics, UCMS and GTB Hospital, Dilshad Garden,
Delhi 110095, India.
Email: [email protected]
Received: December 28, 2016;
Initial review: February 09, 2017;
Accepted: September 22, 2017.
|
Objective: To evaluate the proportion of children
with moderate to severe iron-deficiency anemia who have associated
celiac disease. Methods: This cross-sectional analytical study
was conducted among children aged 1 to 12 years of age with
moderate-to-severe iron deficiency anemia and control children without
anemia.Serum IgA-tissue trans-glutaminase levels were assessed in both
cases and controls. All children with positive celiac serology underwent
upper gastrointestinal endoscopy and duodenal biopsy; biopsy finding of
Marsh grade 3 was considered positive for celiac disease. Results:
There were 152 anemic children and 152 controls with mean (SD)
hemoglobinof 7.7 (1.8) and 12.2 (0.74) g/dL, respectively. 16 (10.5%)
cases and 3 (2%) control patients had positive serology for celiac
disease [OR (95% CI) 5.33 (1.52-18.67), P=0.007]. Six (3.9%)
children with iron-deficiency anemia and none of the controls had biopsy
features diagnostic of celiac disease. Conclusion:In the Northern
Indian tertiary-care hospital outpatient setting, Celiac disease was
associated with 4% of children presenting with moderate-to-severe
anemia.
Keywords: Biopsy, Diagnosis, Endoscopy, Transglutaminases.
|
|
U
nexplained iron-deficiency anemia without
gastro-intestinal symptoms is a well-recognized presentation of celiac
disease (CD) [1]. However, the data regarding the proportional
contribution of CD to unexplained anemia in children are scarce,
especially from a country like India where nutritional anemias are very
common [2]. Children diagnosed with CD require major dietary
modifications in addition to the treatment of the nutritional anemia
[3]. This study was conducted to assess proportionate contribution of
celiac disease as the underlying causative factor of the iron deficiency
anemia.
Methods
This cross-sectional study was conducted in the
pediatric outpatient department of a tertiary-care center in Delhi over
a period of 18 months in 2013-15. Children between the ages of 1 and 12
years with visible pallor as detected on physical examination were
included in the study if they had moderate-to-severe iron-deficiency
anemia (IDA). Moderate anemia was defined as hemoglobin concentration:
7-9.9 g/dL in children <5 years of age and 8-10.9 g/dL in children of 5
to 12 years of age. Severe anemia was defined as hemoglobin
concentration: <7 g/dL in children <5 years of age; <8 g/dL in children
of 5 to 12 years of age [4]. Iron-deficiency was considered as a cause
of anemia if serum ferritin level was <12 ng/mL and/or transferrin
saturation <16% [5,6]. Healthy siblings of patients visiting the
outpatient department were chosen as controls.The controls consisted of
children with normal hemoglobin level as per the age (hemoglobin>11 g/dL
in 12-59 month, >11.5 g/dL in 5-11 years of age, >12 g/dL in 12 years of
age) and normocytic normochromic cells. Exclusion criteria were: severe
acute infection (pneumonia), chronic diseases (cardiac, renal, hepatic,
autoimmune disease, immunodefi-ciencies), hematological disorders,
chronic gastrointes-tinal diseases, already diagnosed celiac disease,
bleeding, intake of any cytotoxic agents or radiotherapy in the last 6
weeks.
A detailed history with emphasis on current or past
gastrointestinal symptoms was taken from the children or their parents.
Nutritional status was assessed at the time of entry into the study. All
eligible anemic children underwent hematological work-up that included
hemogram, peripheral blood smear, red blood cell indices, serum iron
levels, total iron binding capacity, transferrin saturation and serum
ferritin levels. Stool examination was done on two consecutive days for
identification of parasitic infestations. Children who were recruited as
controls had a complete blood count done prior to enrolment.
We measured IgA-anti tissue transglutaminase (IgA-tTG)
by ELISA (Aeskulisa) in all included patients. IgA-tTG levels >18 U/mL
were as considered positive as per information provided by the
manufacturer, levels between 12 and 18 U/mL were considered as
equivocal, and levels <12 U/mL were considered as negative. All children
who screened positive for celiac disease underwent upper
gastrointestinal (UGI) endoscopy. Four biopsy specimens were taken from
the second/first portion of the duodenum, out of which at least one
sample was taken from the duodenal bulb. Histopathological examination
of duodenal biopsies was performed by a histopathologist blinded to
clinical history, and the result was graded using the modified Marsh
grading [7]. Final diagnosis of CD was based on serology and endoscopic
duodenal biopsy (Grade-3). Children diagnosed as CD were adviced strict
gluten-free diet and oral iron supple-mentation for nutritional anemia.
Children with IDA were advised oral iron preprations and dietary
supplementation.
A sample size of 138 children with anemia (and 138
non-anemic controls) was calculated to determine the proportion of
celiac disease with an estimated proportion of 10% [5] with absolute
precision of 0.05 and confidence interval of 95%. Assuming 10% loss to
follow up, 152 cases and control were recruited. The statistical
software SPSS 17 for Windows (Illinois, Chicago) was used for
statistical analysis. Fischers exact test was applied to compare the
proportion IgA-tTG positive patients among cases and controls. Ethical
clearance was obtained from Institutional ethical committee of
University College of Medical Sciences. A written informed consent was
obtained from parents of children eligible for inclusion, and assent was
taken from children ³7
years of age.
Results
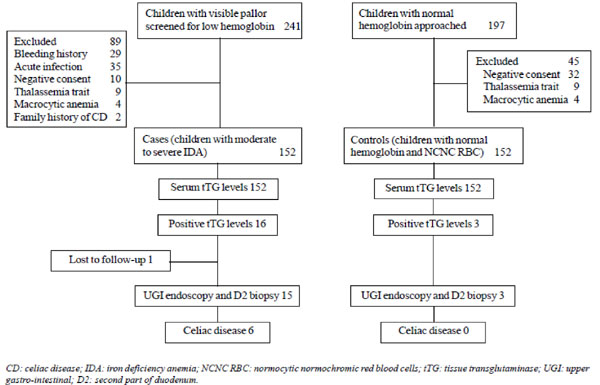
The flow of participants in the study is shown in
Fig.1. We included 152 cases and 152 controls. The non-anemic
controls were of higher age group as compared to anemic cases [mean
(SD): 86.9 (39) months vs 41 (32.9) months; P=0.002] (Table
I).
 |
|
Fig.1 Study flow chart.
|
TABLE I Demographic Characteristics of Children With and Without Anemia
|
Cases (n=152) |
Controls (n=152) |
|
Gender (M:F) |
1.33 |
1.23 |
|
#Age (mo) |
41 (32.9) |
86.9 (39.0) |
|
WAZ |
-1.06 (0.92) |
-0.93 (0.96) |
|
#HAZ |
-1.41 (0.87) |
-1.12 (0.95) |
|
WHZ |
-0.47 (1.36) |
-0.12 (1.51) |
|
MAC (cm) |
15.20 (1.63) |
16.63 (1.85) |
|
*Hemoglobin (g/dL) |
7.71 (1.80) |
12.2 (0.74) |
|
All value in mean (SD); WAZ: weight for age z score; HAZ: height
for age z score; WHZ: weight for height z score; MAC: midarm
circumference. *P=0.001; #P<0.01. |
Increased prevalence of IgA-TTG was found among
anemic children, as compared to non-anemic controls (16 vs 3;
P=0.007). Endoscopy was conducted in 18 children (15 anemic), of
which normal villous pattern was seen in 3 controls and 5 with anemia
Marsh Grade I and grade IIIb findings were seen in 6 and 2, respectively
of the anemic children. Two anemic children had giardiasis. After UGI
endoscopy and biopsy, six (3.9%) children with moderate or severe anemia
and none of the control group were diagnosed as celiac disease (P=0.013).
Among 92 children with moderate anemia, one (1.08%) patient had celiac
disease while among 59 children with severe anemia 5 (8.5%) had celiac
disease. There was a significant difference between the mean (SD)
hemoglobin level between patients with celiac disease and patients
without celiac disease [6.38 (1.13) g/dL vs 7.77 (1.80) g/dL;
P=0.029]. Subgroup analysis between anemic patients with or without
celiac disease is mentioned in Table II.
TABLE II Comparison of Anemic Patients With or Without Celiac Disease
|
Celiac disease
(n=6) |
No celiac disease
(n=146) |
|
Wasting |
0 |
16 (11%) |
|
Stunting |
0 |
30 (20.5%) |
|
#Hemoglobin (g/dL) |
6.4 (1.13) |
7.8 (1.80) |
|
*Severe anemia |
5 (83.3%) |
54 (37%) |
|
Moderate anemia |
1 (16.6%) |
92 (63%) |
|
*P=0.02; All value in no (%) except #hemoglobin in mean (SD).
|
Discussion
This cross-sectional study showed that celiac disease
accounted for 8.5% and 3.9% of children with severe and moderate to
severe iron deficiency anemia, respectively at a tertiary-care hospital
outpatient setting in Northern India.
Studies in children with iron-deficiency anemia are
limited [1,8,9]. A study by Ertekin, et al. [9] among Turkish
children had similar results with a mean hemoglobin level significantly
lower in IDA patients with CD than in those without CD [9]. Moreover,
those with severe anemia had higher odds of having CD.
As prevalence of anemia in India children 6 months-59
months is 58.4% [2], there is a greater chance of missing those children
with celiac disease presenting atypically as anemia. Early
identification of these subclinical cases in childhood assumes greater
importance since these patients are at risk of malignancy and mortality
in later life and morbidity like the presence of unsuspected nutritional
deficiencies.
The major limitation of this study is that being a
hospital-based study results obtained in this study might not be
representative of the whole population. The sample size was inadequate
to find other clinical predictors of celiac disease in anemic children.
Not doing IgA levels to screen for IgA deficiency, non-evaluation of
occult blood loss in stool, and controls not being age matched are other
study limitations. No loss to follow-up and outcome assessment using
endoscopy are the strengths of the present study.
We conclude that anemic children, especially those
presenting with severe anemia have significantly higher likelihood of
having CD. Physicians treating children with severe anemia may consider
screening them for celiac disease. We recommend community-based studies
to confirm these findings.
Contributors: MN: Study conception and manuscript
writing; RN: Data collection, analysis and manuscript writing; DS: Study
conception, and critical review of manuscript for intellectual content;
ASP, VM and MK: Study related procedures (data collection), their
interpretation and critical inputs into manuscript.
Funding: None; Competing interests: None
stated.
|
What This Study Adds?
Severely anemic patients have
higher chances of having associated celiac disease.
|
References
1. Kavimandan A, Sharma M, Verma AK, Das P, Mishra P,
Sinha S, et al. Prevalence of celiac disease in nutritional
anemia at a tertiary care center. Indian J Gastroenterol. 2013;33:114-8.
2. National Family Health Survey-4, 2015-16: India
Fact Sheet. Ministry of Health and Family Welfare. Available from:
http://rchiips.org/NFHS/pdf/NFHS4/India.pdf. Accessed April 2, 2017.
3. Hill ID, Dirks MH, Liptak GS, Colletti RB, Fasano
A, Guandalini S, et al. Guideline for the Diagnosis and Treatment
of Celiac Disease in Children: Recommen-dations of the North American
Society for Pediatric Gastroenterology, Hepatology. J Pediatr
Gastroenterol Nutr. 2005;40:1-19.
4. World Health Organization: Department of Nutrition
for Health and development; Haemoglobin concentration for the Diagnosis
of Anaemia and Assessment of Severity. Geneva, WHO, 2011.
(WHO/NMH/NHD/MNM/11.1). Available from: http://apps.who.int/iris/bitstream/
10665/101179/1/WHO_NMH_NHD_EPG_14.1_eng. pdf. Accessed December 27,
2016.
5. World Health Organization: Serum Ferritin
Concentrations for the Assessment of Iron Status and Iron Deficiency in
Populations. Vitamin and Mineral Nutrition Information System. Geneva,
World Health Organization, 2011. (WHO/NMH/NHD/MNM/11.2). Available from:
http://www.who.int/vmnis/indicators/serum_ferritin.pdf. Accessed
December 27, 2016.
6. Bainton DF, Finch CA. The diagnosis of iron
deficiency anemia. Am J Med. 1964;37:62-70.
7. Marsh MN, Crowe PT. Morphology of the mucosal
lesion in gluten sensitivity. Baillieres Clin Gastroenterol.
1995;9:273-93.
8. Kalayci AG, Kanber Y, Birinci A, Yildiz L,
Albayrak D. The prevalence of coeliac disease as detected by screening
in children with iron deficiency anaemia. Acta Paediatr. 2005;94:678-81.
9. Ertekin V, Tozun MS, Küçük N. The prevalence of
celiac disease in children with iron-deficiency anemia. Turk J
Gastroenterol. 2013;24:334-8.
|
|
|
 |
|

