|
|
|
Indian Pediatr 2012;49: 62-64
|
 |
Infantile Systemic Hyalinosis |
|
Prabhas Prasun Giri, Rajesh Raushan, Apurba Ghosh and *Priyankar Pal
From the Departments of Pediatric Medicine, and *Pediatric Rheumatology, Institute of Child Health, Kolkata 17, India.
Correspondence to:
Dr Prabhas Prasun Giri, C-1, ANANDAN, 173,Sarat Ghosh Garden Road,
Email:
[email protected]
Received: May 6, 2010;
Initial review: June 11, 2010;
Accepted: September 27, 2010.
|
Infantile systemic hyalinosis is a rare disorder characterized by widespread deposition of hyaline. They usually present with skin lesions, joint contractures, and intractable diarrhea. We report a 2 year 4 month old boy with growth retardation, typical facial appearance, gingival enlargement, generalized stiff skin, joint contractures, and intermittent diarrhea. Skin biopsy revealed deposition of hyaline.
Key words: Hyalinosis, Skin involvement.
|
|
Infantile systemic hyalinosis (ISH) is a rare,
progressive, fatal autosomal recessive condition [1].
Till 2009, fewer than 20 patients with ISH were
reported and all of them died in early childhood, mainly due to severe diarrhea, pulmonary infections, or septicemia. It is characterized by widespread deposition of hyaline material in many tissues such as skin, gastrointestinal tract, adrenals, skeletal muscles, gingiva and other loci [2-4]. We report a case of infantile systemic hyalinosis.
Case Report
A 2 year 4 months old boy presented with history of skin lesions on the face, ear, neck and the perianal regions since the age of 6 months. The skin lesions were progressively increasing in size and number. His parents noticed that he experienced discomfort on being handled and had difficulty in moving his limbs. Over the last one year, he gradually developed severe joint contractures in most of the large and small joints. He also started having recurrent episodes of diarrhea. There was no history of similar illness in any family member; elder sister aged 6 year was normal.
On examination, the child had normal developmental milestones, coarse facies , anteverted nose, and low set ears. He was short for age (height 75 cm, -2SD). His weight was 8.5 kg (-2SD).He was unable to stand or sit without support. Oro-dental examination revealed gingival hypertrophy.There were severe contractures in bilateral ankle, knee, hip, wrist, elbow, shoulder and small joints of hands and feet.
Cutaneous examination revealed the presence of multiple, skin-colored and pink papules of variable sizes over his ear lobes, inside his ear, around his nose, and on the nasolabial folds, chin, and mouth. They were clustered together and confluent at the nose, ear lobules, and chin (Fig. 1). The trunk and limbs were spared. He had multiple, pearly, grouped papules on the dorsum of the neck and in the perianal region . There was rectal prolapse. Overall, the skin was not thickened, but showed hyperpigmented areas over the metacarpophalangeal joints and the malleoli.
 |
Fig. 1 Multiple skin colored and pink papules coalescing to form hyperpigmented plaques over nose, chin and forehead. |
Hematological and biochemical investigations were normal except for a borderline low calcium level. Chest X-ray was normal. Skeletal radiographs revealed a wide anterior fontanel, thick vertebral bodies, and diffusely demineralized long bones with evidence of healed fractures.There was coxa vara with genu varum. ECG, echocardiography,USG whole abdomen, and MRI brain was normal. A skin biopsy taken from the neck lesions showed mild hyperkeratotic epidermis with thinning and flattening of the rete ridges at places.Papillary dermis was edematous and there was a pink homogeneous acellular material throughout the dermis-suggestive of hyaline (Fig. 2).
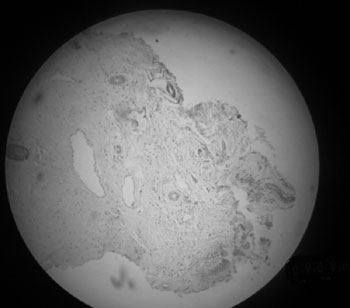 |
Fig. 2 Skin biopsy showing deposition of hyaline. |
The child was diagnosed as a case of infantile systemic hyalinosis and treated with oral calcium,d-penicillamine and supportive therapy . Orthopedic splints were applied for the contractures and physiotherapy started. On follow up, the child is clinically stable without appearance of new skin lesions and diarrhea has also subsided.
Discussion
Infantile systemic hyalinosis (ISH) is linked to a disorder of synthesis of glycosaminoglycan with resulting abnormality in collagen synthesis.The gene locus has been found on Chromosome 4q21. There are mutations in the CMG2/ANTXR2 gene [5]. However, the pathogenesis of hyalinosis syndromes is unclear. Ultra-structurally an apparent increase in the amount of collagen type VI is suggested to account for the clinical features of inflexible skin and the limitation of joint movement [6]. ISH has been mostly linked to mutations in the von Willebrand factor A (v WA) domains in the CMG2 gene.
Our case had characteristic clinical features of ISH including joint contractures, and diverse degrees of bone involvement [7]. Diarrhea is ascribed to protein losing enteropathy due to thickening and hyaline infiltration of the intestinal walls. Visceral involvement is associated with feeding problems, malnutrition,repeated chest infections and fatal outcome usually within 2 years of life due to sepsis with renal, respiratory or heart failure [8].
Histology was characterstic and showed deposition of an amorphous, eosinophilic hyaline material. Juvenile hyaline fibromatosis is another disorder similar to ISH with same genetic and histological features but with lesser joint and visceral involvement. Usually the skin is not thickened and there is multiple large nodules and tumours . Clinical features appear after one year and slowly prog-ress. There is usually no diarrhea, chest infection and growth retardation. Survival is usually prolonged beyond 30 years.
No specific treatment is available for ISH. Early surgical excision is recommended by some authors for those lesions that either present a significant cosmetic problem or produce some degree of functional impairment. However, excision may be followed by recurrences. Spontaneous regression has been reported in some cases, but long-term regression is unlikely and tumors continue to increase in size and number. Intralesional steroid injection may reduce the size of early lesions. Capsulotomy of joints may show some temporary, beneficial effect. Gingival overgrowth may be treated with partial gingivectomy. Oral D-penicillamine has been used in some cases with apparent improvement in joint mobility and flexibility.Therapeutic trials with dimethyl sulfoxide,ketotifen and calcitriol have been given in individual cases. Genetic counselling should be done as there is 25% chance of development of disease in future offsprings.
Contributors: All authors contributed to literature search, patient care and drafting the manuscript.
Funding: None; Competing interests: None stated.
References
1. Büyükgebiz B, Öztürk Y, Arslan N, Özer E. A rare cause of protein-losing enteropathy and growth retardation in infancy: infantile systemic hyalinosis. Turk J Pediatr. 2003;45: 258-60.
2. Landing BH, Nadorra R. Infantile systemic hyalinosis: report of four cases of a disease, fatal in infancy, apparently different from juvenile systemic hyalinosis. Pediatr Pediatr Pathol. 1986;6:55-79.
3. Al-Mubarak L, Al-Makadma A, Al-Khenaizan S. Infantile systemic hyalinosis presenting as intractable infantile diarrhea. Eur J Pediatr. 2009;168:363-5.
4. Dhingra M, Amladi S, Savant S, Nayak C. Juvenile hyaline fibromatosis and infantile systemic hyalinosis: Divergent expressions of the same genetic defect? Indian J Dermatol Venereol Leprol. 2008;74:371-4.
5. Rahman N, Dunstan M, Teare MD, Hanks S, Edkins SJ, Hughes J, et al. The gene for juvenile hyaline fibromatosis maps to chromosome 4q21. Am J Hum Genet. 2002;71:975-80.
6. Huang YC, Xiao YY, Zheng YH, Jang W, Yang YL, Zhu XJ. Infantile systemic hyalinosis: a case report and mutation analysis in a Chinese infant. Br J Dermatol. 2007;156:602-4.
7. Mancini GMS, Stojanov L, Willemsen R. Juvenile hyaline fibromatosis: clinical heterogeneity in three patients. Dermatology. 1999;198:18-25.
8. Urbina F, Sazunic I, Murray G. Infantile systemic hyalinosis or juvenile hyaline fibromatosis? Pediatr Dermatol. 2004;21:154-9.
|
|
|
 |
|

