|
The probability of having a malformed child
appears to be 2 to 3 times greater in epileptic women who receive
diphenylhydantion early in pregnancy than in women who have no
history of a convulsive disorder(1). We report an unusual cardiac
malformation in a neonate born to a mother on phenytoin.
G, a 21-year-old primigravida was a known
epileptic on anticonvulsant medication (phenytoin 100 mg twice a
day) for 3 years prior to conception. She conceived spontaneously
and was taking the drug all through her pregnancy. The pregnancy
was otherwise uncomplicated and she delivered a male baby at 32
weeks of gestation after a prolonged rupture of membranes for 30
hours. The baby weighed 1600 g at birth and did not require
resuscitation. Examination showed a preaxial polydactyly on the
right hand, hypospadias, precordial activity and a grade III
systolic murmur in the left parasternal area. The baby was pink
and all pulses were well palpable. The systolic/diastolic pressure
was 73/41 mm of Hg with a mean arterial pressure of 51 mm of Hg.
He was started on tube feeds on day 1. Chest X ray on day 1 was
unremarkable. The baby showed unusual weight gain and poor
peripheral circulation on second day of life and progressed to
cardiogenic shock on day 3. On day 3, chest radiograph showed
increased vascularity and cardiomegaly. The shock progressed in
spite of inotropic support and ventilation and the baby died on
day 5 of life due to cardiogenic shock, and renal failure.
Postmortem examination of the baby revealed type I truncus
ateriosus, large ventricular septal defect, absent ductus
arteriosus, large atrial septal defect and an absent right
coronary artery(Fig. 1).
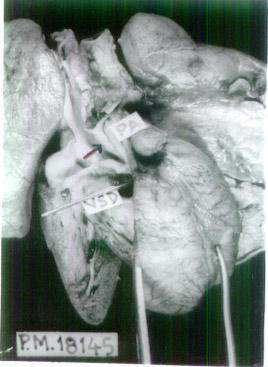 |
| Fig. 1.
Postmortem dissection of the heart with type I truncus
arteriosus (arrow) and ventricular septal defect (VSD). |
The features of fetal hydantoin syndrome
include craniofacial anomalies, prenatal and postnatal growth
deficiencies, mental retardation and limb defects. Less frequently
observed abnormalities include microcephaly, ocular defects,
cardiovascular anomalies, hypospadiasis, and umbilical and
inguinal hernias(2).
Cardiac anomalies are the most life
threatening, though cleft lip and cleft palate are the most common
malformations(3). The incidence of congenital heart disease in an
infant exposed to phenytoin in utero is four times greater
than the infants not exposed to this medication. Ventricular
septal defect is the most common cardiac anomaly and the other
reported ones are patent ductus arteriosus, coarctation of aorta,
pulmonary and aortic stenosis, pulmonary atresia, and tetralogy of
Fallot(4). To the best of our knowledge truncus arteriosus with
absent ductus and absent coronary artery has never been reported
in association with phenytoin exposure in utero. The other
anomalies i.e., ventricular septal defect, atrial septal
defect, polydactly and hypospadiasis seen in the index child are
well known manifestations of fetal hydantoin syndrome.
Should phenytoin be discontinued in pregnant epileptic women?
The answer probably is "No" as almost every available
antiepileptic drug has been associated with congenital
malformation. Since the effects of the drug are dose dependent it
is prudent to use them with regular drug monitoring and with
downward adjustment of the dose when necessary(5). Supplementation
with folic acid might also be considered.
Srinivas Murki,
Sourabh
Dutta,
Mahesha V,
Division of Neonatology, Department of Pediatrics
and Department of Pathology, PGIMER,,
Chandigarh 160 012, India.
E-mail: [email protected]
1. Monson RR,
Rosenberg L, Hartz CH, Shapiro S, Heinonen OP, Slone D.
Diphenylhydantoin and selected congenital malformations. NEJM
1973; 289: 1049-1052.
2. Hill RM,
Verniaud WM, Horning MG, McCulley LB, Morgan NF. Infants exposed
in utero to antiepileptic drugs. Am J Dis Child 1974; 127:
645-653.
3. Speidel BD,
Meadow SR. Maternal epilepsy and abnormalities of the fetus and
newborn. Lancet 1972; 2: 839-843.
4. Swartjes JM,
Van Geijn HP. Pregnancy and epilepsy. Eur J Obstet Gynecol
Reprod Biol 1998; 76: 3-11.
5. Shillingford AJ, Weiner S.
Maternal issues affecting the fetus. Clin Perinatol 2001; 28:
31-70.
|
