|
|
|
Indian Pediatr 2009;46: 133-136 |
 |
Comparative Effectiveness of Tepid Sponging
and Antipyretic Drug Versus Only Antipyretic Drug in the
Management of Fever Among Children: A Randomized Controlled
Trial |
|
S Thomas, C Vijaykumar, R Naik, PD Moses* and B
Antonisamy**
From the Department of Child Health Nursing, *Child
Health Department and **Department of Biostatistics,
Christian Medical College, Vellore, India.
Correspondence to: Dr Prabhakar D Moses, Professor and
Head of Child Health Unit III, Christian Medical College Hospital, Vellore
632 004, Tamil Nadu, India.
E-mail: [email protected]
Manuscript received: November 23, 2006;
Initial review completed: January 29, 2007;
Revision accepted: April 21, 2008. |
|
Abstract
Objective: To compare the effectiveness of tepid
sponging and antipyretic drug versus only antipyretic drug among febrile
children.
Design: Randomized controlled trial.
Setting: Tertiary care hospital.
Participants: 150 children 6 mo – 12 yr age with
axillary temperature ³ 101ºF.
Intervention: Tepid sponging and antipyretic drug
(Paracetamol) (n=73) or only antipyretic drug (Paracetamol) (n=77).
Main outcome measures: Reduction of body
temperature and level of comfort.
Results: The reduction of body temperature in the
tepid sponging and antipyretic drug group was significantly faster than
only antipyretic group; however, by the end of 2 hours both groups had
reached the same degree of temperature. The children in tepid sponging and
antipyretic drug had significantly higher discomfort than only antipyretic
group, but the discomfort was mostly mild.
Conclusion: Apart from the initial rapid
temperature reduction, addition of tepid sponging to antipyretic
administration does not offer any advantage in ultimate reduction of
temperature; moreover it may result in additional discomfort.
Keywords: Antipyretic drug, Fever, Hydrotherapy, Paracetamol, Tepid
sponging.
|
|
Fever is a common
childhood problem faced by health care personnel including doctors, nurses
and others in both hospital and community settings. However, the nursing
management of fever in children is often not based on research and remains
inconsistent in practice(1,2). Several methods have been recommended to
reduce fever in children, which include tepid sponging, fanning, alcohol
sponging and antipyretics. However, controversy surrounds the use of tepid
sponge for reduction of fever. The effectiveness of tepid sponging as a
treatment alongside antipyretic varies between studies, with some finding
that it is of no benefit(3) and others suggesting that it is helpful(4).
There is dearth of related studies in India. Therefore, we conducted a
study to compare the effectiveness of tepid sponging and antipyretic drug
versus only antipyretic drug in the management of fever among children.
Methods
The study was conducted at Child Health Department of
Christian Medical College, Vellore, a tertiary care hospital in South
India. The study subjects were children in the age group of 6 months – 12
years, who presented with fever (axillary temperature
³101ºF).
Children who had received antipyretic drug within 4 hours before or those
with active seizure or clinically unstable were excluded. A written
informed consent was obtained from the parents. A minimum sample of 60 in
each group had a 90% power of detecting a difference of 0.40° F mean
change between the baseline and the last follow up and with a follow up
correlation of 0.70 and the level of significance at 5% (two sided).
The children were then randomized by using a random
number table to receive tepid sponging and antipyretic drug or only
antipyretic drug. The initial temperature checking time was considered as
0 minutes. If the child belonged to the group of tepid sponging and
antipyretic group, syrup/tablets paracetamol 10 mg/kg was administered and
was sponged for 15 minutes. Tepid sponging procedure was as follows:
Required articles: 5 sponge towels, a steel/enamel basin, Mackintosh, 2
bath towels, thermometer, bath thermometer and tap water (room temperature
–0.5°C). After washing hands and checking the temperature of the child, a
long mackintosh was spread under the patient. After assuring privacy the
dress was removed and the child covered with top sheet. A sponge was then
used to dab over the face and neck without touching the eyes and kept at
the edge of the basin. A second sponge was used to dab one arm starting
from the acromion process and proceeding laterally till the fingers and
then medially reaching the axilla. The sponge cloth was left in the
axillary pit. The same was done for the other arm. For the legs, a sponge
cloth was used to dab from the groin proceeding laterally till the feet
and then medially reaching the groin. The sponge cloth was kept on the
fold of the groin. The abdomen and back were dabbed with the first sponge
kept at the edge of the basin. The procedure was completed in 15 minutes,
when the child was dabbed dry. At 15 minutes point, temperature was
checked and if it continued to be >101° F, sponging was administered for
another 15 minutes. Later temperature was checked at 30, 45, 60, 90 and
120 minutes. Children in the only antipyretic drug group received only
paracetamol (10mg/kg) at 0 minutes and subsequently temperature was
monitored at similar intervals. The level of discomfort of children was
also assessed at the same time points in terms of 3 criteria–crying,
restlessness and irritability. It was scored and the total score was
converted into percentage and was interpreted as mild, moderate and severe
discomfort.
The reduction of body temperature between the treatment
groups was analysed using the analysis of covariance method adjusting for
the baseline temperature. The level of discomfort was also subjected to
statistical tests of significance. STATA software was used for the
statistical analysis of the data.
Results
One hundred and fifty children were studied, 73 in the
tepid sponging and antipyretic drug group and 77 children in the only
antipyretic drug group. The baseline characteristics are shown in
Table I. Males outnumbered females in both the groups by an
approximate ratio of 2:1. Majority of children in both the groups had
respiratory diseases like upper respiratory tract infection, pneumonia
etc. A higher number of children in both groups had their initial body
temperature between 101° F – 103° F.
TABLE I
Baseline Characteristics of the Study Children
|
Variable |
Tepid sponging and
antipyretic drug group
(N=73) |
Only antipyretic
drug group
(N=77) |
| |
n |
% |
n |
% |
| Age |
| 6 months–2 years |
30 |
41.1 |
30 |
38.9 |
| 3 years – 6 years |
28 |
38.4 |
32 |
41.6 |
| 7 years – 12 years |
15 |
20.5 |
15 |
19.5 |
| Sex |
| Male |
46 |
63.0 |
53 |
68.8 |
| Female |
27 |
37.0 |
24 |
31.2 |
| Initial body temperature |
| 101ºF–102ºF |
28 |
38.4 |
38 |
49.3 |
| 102ºF–103ºF |
32 |
43.8 |
28 |
36.4 |
| 103ºF–104ºF |
13 |
17.8 |
11 |
14.3 |
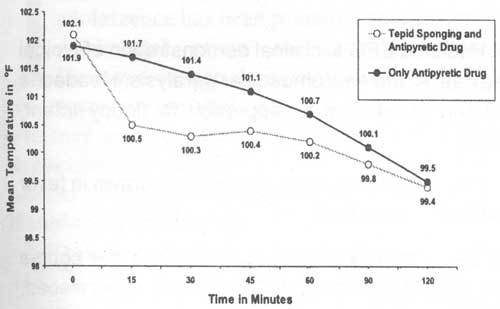
The mean temperature of both groups at different time
intervals is depicted in the graph (Fig.1). It shows a rapid
reduction of temperature in the tepid sponging and antipyretic group at 15
minutes. Only antipyretic group had slow but sustained reduction in
temperature.
 |
|
Fig. 1 Mean temperature of the Tepid
sponging and antipyretic drug group and Only antipyretic drug group
at different time intervals. |
The comparative effectiveness of the two methods was
assessed based on the analysis of covariance. The results indicate that
there is a difference in mean temperature over time between the treatment
methods after adjusting for the initial temperature as covariate. The
analysis of covariance confirms the rapid reduction of temperature in the
combined tepid sponging and antipyretic group as shown in Fig.1.
However, by the end of 2 hours both groups had reached the same degree of
temperature. There was no difference in ultimate reduction of temperature
between the two groups.
The level of discomfort was higher in tepid sponging
and antipyretic group than only antipyretic group. It was compared by
using a chi-square test and the result showed a statistically significant
value (P<0.001). The discomfort in the tepid sponging group was
mostly mild.
Discussion
Administration of tepid sponging for fever has been
practised for years. Formally and informally, healthcare personnel have
voiced opinion for and against the practice of tepid sponging and
questioned its relative effectiveness compared to other methods.
A number of studies have been done to compare the
efficacy of these methods. Some of them had shown that tepid sponging with
antipyretic drug is more effective than only antipyretic drug(5,6), while
others concluded that there was no difference in temperature
reduction(3,4). We observed that administration of tepid sponging and
antipyretic drug resulted in rapid temperature reduction in the initial
15-30 minutes as compared to antipyretic drug alone; however, by the end
of 2 hours both groups had reached the same degree of temperature. There
was no difference in ultimate reduction of temperature between the two
groups.
Children in the tepid sponging and antipyretic group
had a higher level of discomfort than only antipyretic group, although the
discomfort was only mild in most cases. These findings are supported by
Sharber(4), but certain other studies did not find any significant
difference, although they used different criteria for assessing
discomfort(6,7). Our findings are also supported by Cochrane Evidence
Update. which states: "In trials where all children received paracetamol,
those who were treated with tepid sponging in addition to paracetamol were
more likely to be clear of fever at 1 hour (relative risk 11.76 (3.39 to
40.79), 2 trials, 125 children). Shivering and goosebumps were more common
with tepid sponging (relative risk 5.09 (1.56 to 16.60); 3 trials, 145
children)(8).
Based on our findings and review of literature(9,10),
we conclude that apart from the initial rapid temperature reduction,
addition of tepid sponging to antipyretic administration does not offer
any advantage in ultimate reduction of temperature and may result in
additional discomfort.
Contributors: All authors contributed to concept,
design, literature search, data collection and drafting the manuscript.
PDM stands as guarantor.
Funding: None.
Competing interests: None stated.
|
What is Already Known?
• Fever reducing measures in children include
antipyretic administration and tepid sponging (hydrotherapy).
What This Study Adds?
• Apart from the initial rapid temperature
reduction, addition of tepid sponging to antipyretic administration
does not offer any advantage in ultimate reduction of temperature;
it may result in additional discomfort. |
References
1. Watts R, Robertson J, Thomas G. Nursing management
of fever in children a systematic review. Int J Nurs Pract 2003; 9: 1-8.
2. Gildea JH.When fever becomes an enemy. Pediatr Nurs
1992; 18: 165-167.
3. Newman J. Evaluation of sponging to reduce
temperature in febrile children. Can Med Assoc J 1985; 132: 641-642.
4. Sharber J. The efficacy of tepid sponge bathing to
reduce fever in young children. Am J Emerg Med 1997; 15: 188-192.
5. Barton LL, Friedman AD. Efficacy of sponging vs.
acetaminophen for reduction of fever. Pediatr Emerg Care 1990; 6: 255-257
6. Mahar AF, Allen SJ, Milligan P, Suthumnirund S,
Chotpitayasunondh T, Sabchareon A, et al. Tepid sponging to reduce
temperature in febrile children in a tropical climate. Clin Pediatr
(Phila) 1994; 33: 227-231.
7. Agbolosu NB, Broadhead RL, Brauster D, Graham SM.
Efficacy of tepid sponging versus paracetamol in reducing temperature in
febrile children. Annals Trop Pediatr 1998; 18: 335-336.
8. Meremikwu M, Oyo-Ita A. Physical methods for
treating fever in children. Cochrane Database Syst Rev 2003; 2: CD004264.
9. Crocette M, Moghbeli N, Serwint J. Fever phobia
revisited: Have parental misconceptions changed? Paediatrics 2001; 107:
1241-1246.
10. Krantz C. Childhood fever: developing evidence based anticipatory
guidance tool for parents. Pediatr Nurs 2001; 27: 567-571. |
|
|
 |
|

