|
|
|
Indian Pediatr 2016;53: 1107-1108 |
 |
Percutaneous
Transhepatic Angioplasty for Portal Vein Cavernous
Transformation after Choledochal Cyst Surgery
|
|
Wenjun Shen, *Jianjun Luo, Shan Zheng and Xianmin
Xiao
From Department of Pediatric surgery, Childrenís
Hospital of Fudan University and *Department of Interventional
Radiology, Zhongshan Hospital of Fudan University, Shanghai, China.
Correspondence to: Dr Wenjun Shen,
Lane 399 Wanyuan Road Minhang District, Shanghai, China201102.
Email: [email protected]
Received: September 02, 2015;
Initial Review: October 20, 2015;
Accepted: October 04, 2016.
|
Background: Cavernous transformation of the
portal vein rarely occurs after a choledochal cyst surgery. Case
characteristics: A 7-year-old boy with a history of a choledochal
cyst surgery was admitted with recurrent oral and nasal bleeding over
next two years. After excluding coagulopathies and hematopathies, we
treated him with percutaneous transhepatic angioplasty. Outcome:
The flow of the portal vein recovered immediately after balloon
dilation. The patientís symptoms were relieved, and no recurrence or
complications occurred. Message: Stenosis and cavernous
transformation of portal vein can be successfully managed by
percutaneous transhepatic angioplasty.
Keywords: Complications, Hematomasis, Portal Hypertension.
|
|
C
avernous transformation of the portal vein
(CTPV), known as portal cavernoma, is caused by stenosis or obstruction
of the portal vein. This condition leads to spontaneous bypass across
the stenosis, which sustains blood flow and liver function. Most cases
of CTPV in children are caused by neonatal septicemia, and umbilical and
intra-abdominal infections. However, CTPV has been rarely reported after
choledochal cyst surgery. The traditional treatment for CTPV is surgery.
We report a case of successful treatment of a CTPV by percutaneous
transhepatic angioplasty.
Case Report
A 7-year-old boy was admitted to our center with
recurring oral and nasal bleeding. Physical examination revealed
splenomegaly and an abdominal scar, and ultrasound examination showed
extrahepatic portal vein stenosis (Fig. 1). The boy had a
history of a choledochal cyst treated by Roux-en-Y hepatoenterostomy 6
years previously. The patient had no signs of fever or jaundice during
the early follow-up period, and ultrasound examination findings were
normal for 6 months after the operation. Over a period of next 4 years,
his spleen size started increasing, platelet counts decreased, and he
developed gastro-intestinal bleeding. Gastroscopy revealed moderately
severe varicose veins in the gastric fundus and distal esophagus; barium
meal examination showed signs of venous beading at the bottom of the
esophagus, indicating a spontaneous portosystemic shunt (Fig.
1). Enhanced computed tomography (CT) indicated splenomegaly and the
dilation of the portal and splenic vein (Fig. 1). Color
doppler ultrasound showed main portal vein diameter from 4.4 to 7.8 mm
and a flow velocity of 11.0 cm/s. The diameter of the right portal, left
portal, and splenic vein were 7.2, 5.0, and 9.3 mm, respectively.
Three-dimensional CT reconstruction provided direct visualization of the
severe stenosis of the main portal vein.
 |
|
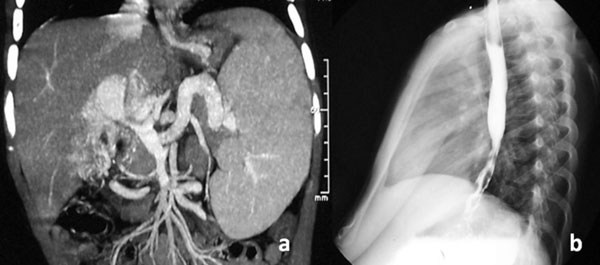
Fig. 1 Enhanced computed tomography
showing severe stenosis of the main portal vein (white arrow)
and dilation of the splenic vein and coronary vein (a); and
Barium swallow showing venous beading at the bottom of the
esophagus indicating a dilated venous shunt (b).
|
We treated the patient with percutaneous transhepatic
angioplasty. The right portal vein was successfully accessed under
ultrasound monitoring, and a 5F sheath was subsequently inserted. A 4F
elbowed catheter was advanced upstream into the superior mesenteric vein
with the help of a guide wire. Digital subtraction angiography confirmed
the presence of portal vein stenosis and pericholecystic collaterals
coursing towards the liver. After the main portal vein was dilated three
times with a Cordis 10-40-mm balloon at 14 atm, it was recanalized and
the collateral vessels disappeared as blood flowed into the liver again
(Web Fig. 1).
The blood flow of the portal vein was immediately
restored. The size of the spleen below the costal margin decreased from
5 to 2 cm within 5 days after the therapy, and the platelet count
normalized. One month after the therapy, CT and ultrasound examinations
showed that the stenosis had been dilated to 4.8 mm with a rising flow
velocity of 62.5 cm/s in the patent portal vein. The stenosis continued
to expand to 5.1 mm within 3 months after the therapy. After 6 months of
warfarin administration, the portal vein remained patent over a
follow-up period of 2 years.
Discussion
Postsurgical complications of choledochal cysts
usually include cholangitis, biliary stone formation, anastomotic
stricture formation, and malignancy. Portal vein stenosis and CTPV are
rare. CTPV is characterized by the presence of collaterals in the
vicinity of the occluded blood vessels. Conditions such as inflammation,
tumor metastasis, regional compression parasite infestation, and chronic
liver disease can lead to occlusion of the portal vein, which then leads
to CTPV [2,3]. However, CTPV may also be found in association with
extrahepatic bile duct stenosis by choledochal varices. Jaundice and
fever are common clinical manifestations. The common bile duct is
extraluminally compressed and laminated in such cases [1]. Pre-operative
ultrasound examination and operative exploration excluded this condition
in the present case (Fig. 1).
Choosing the optimal surgical approach in CTPV is
challenging. Simple disconnection may not effectively reduce the
pressure, with chances of regeneration of collateral circulation and
rebleeding [4]. Creation of a distal splenorenal shunt is the most
commonly performed selective portal decompression procedure in children,
but exposure of the shunt during the portacaval procedure is difficult.
The minimum diameter required for splenic vein anastomosis is 6 mm. A
superior mesenteric vein to intrahepatic left portal vein (Rex) shunt
was recently used to bridge the thrombosis after liver transplantation,
but the vascular condition in present case was highly complex [5].
Transjugular intrahepatic portosystemic shunt (TIPS) reduces the portal
vein pressure gradient to clinically insignificant levels in the short
term, but frequent shunt dysfunction and encephalopathy have precluded
it from being the first-line treatment. Real-time ultrasound-guided
percutaneous transhepatic inter-ventional therapy has the advantages of
minimal invasion, high efficiency, and high reproducibility [6]. It is
widely applied in treatment of portal hypertension, tumor compression,
tumor embolus, and tumor thrombus.
Interventional therapy for post-operative portal vein
occlusion has been used after liver transplantation [7]. Interventional
therapy has now become the first-line treatment for vascular
complications after liver transplantation. Thrombolysis in the
intrahepatic portal vein and angioplasty in the extrahepatic portal vein
through a splenic vein route are often successfully performed [8].
In conclusion, interventional therapy for portal vein
stenosis and CTPV following intra-abdominal surgeries may be an
effective therapeutic option.
Contributors: WS and JL: patient management and
wrote the manuscript; ZS and XX: revised the manuscript.
Funding: None; Competing interests: None
stated.
References
1. Gabriel P, Herve B, Jacques F, Frederic P,
Marianne G, Stanislas C, et al. Biliary obstruction caused by
portal cavernoma: A study of 8 cases. J Hepatol. 1996;25:58-63.
2. Webb LJ, Sherlock S. The etiology, presentation
and natural history of extra-hepatic portal venous stenosis. Q J Med.
1979;48:627-9.
3. De Gaetano AM, Lafortune M, Partiquin H, De Franco
AAB. Cavernous transformation of the portal vein: Patterns of
intrahepatic and splanchnic collateral circulation detected with Doppler
sonography. Am J Roentgenol. 1995;165:1151-55.
4. Galloway JR, Henderson JM. Management of variceal
bleeding in patients with extrahepatic portal vein thrombosis. Am J
Surg. 1990;160:122-7.
5. Bambini DA, Superina R, Almond PS, Whitington PF,
Alonso E. Experience with the Rex shunt (mesenterico-left portal bypass)
in children with extrahepatic portal hypertension. J Pediatr Surg.
2000;35:13-1.
6. Woodrum DA, Bjarnason H, Andrews JC. Portal vein
venoplasty and stent placement in the nontransplant population. J Vasc
Interv Radiol. 2009;20:593-9.
7. Carnevale FC, Borges MV, Moreira AM, Cerri GG,
Maksoud JG. Endovascular treatment of acute portal vein thrombosis after
liver transplantation in a child. Cardiovasc Intervent Radiol.
2006;29:457-61.
8. Bertram H, Pfister ED, Becker T, Schoof S.
Transsplenic endovascular therapy of portal vein stenosis and subsequent
complete portal vein thrombosis in a 2-year-old child. J Vasc Interv
Radiol. 2010;21:1760-4.
|
|
|
 |
|

