World Health Organization (WHO) added tetanus
toxoid vaccine in its Expanded Program on Immunization (EPI) in the year
1974 [1]. Almost 15 year later, by 1989, only a quarter (27%) of
pregnant females were receiving the standard doses of tetanus toxoid
[2]. Year 1990 was initially set as target by WHO to achieve the goal of
neonatal tetanus elimination, defined as less than one case per 1000
live births per year in all districts of a country; it was later
extended to 1995. By the end of 1999, there were 57 countries that had
yet not achieved this goal [3].
In the year 2000, WHO, United Nations Children’s Fund
(UNICEF) and United Nations Population Fund (UNFPA) partnered to
re-launch their efforts to achieve the goal of neonatal tetanus
elimination. As neonatal tetanus depends mainly on tetanus immunization
of the mother during pregnancy, the goal of elimination of maternal
tetanus was also added to this initiative which was rechristened
"Maternal and Neonatal Tetanus Elimination Program" (MNTE), and year
2005 was set as the cut-off year to achieve this goal [3]. However, 19
countries are yet to achieve this goal [4]. India was one of the last
few countries to be declared free of maternal and neonatal tetanus on
15th May, 2015 [5].
Historical Background
In 1960, Schlesinger described tetanus as a dangerous
but rare disease [6]. But this ‘rarity’ of tetanus could be due
to its gross under-reporting at that time. Attention to the massive
burden of tetanus was drawn by Matveev and Sergeeva [7]. They reported
that during the years 1945-53 (in the countries in which the incidence
of tetanus was recorded), there were more than 350 000 cases, of which
nearly one-third died [7].
There were several reasons due to which tetanus, more
so neonatal tetanus, had been neglected historically as a health
problem. One of the main reasons could be that majority of cases
occurred in poor and illiterate populations with limited access to
information about health services and essential obstetric care [8]. As
per Bytchenko [9], neonatal tetanus was neglected by the health services
due to its high cost of treatment, poor outcome, and lack of reliable
epidemiological data. Until 1984, neonatal tetanus was still reported
per 100 000 population, clearly indicating failure to recognize tetanus
as a more important cause of mortality in newborns as compared to other
age groups [10]. The hospital data were also misleading about its real
incidence because the infants were either dying at home or failing to
reach the hospital. Traditional attitudes such as considering neonatal
death as a wish of God and isolation of the mother and child in the
post-partum period were other reasons that correct extent of neonatal
tetanus was not known until late.
Tetanus has existed in Asia for centuries without any
reliable statistics pertaining to its prevalence. The Indian Clinical
Research Advisory Committee in 1946 suggested that there was a pressing
need to study the magnitude of the problem of tetanus. The case fatality
from tetanus as reported from a few states of India in the decade
1951-60 suggested that the case-fatality rate was more than 90% in Goa,
Daman and Diu. Between 1956-62, hospital admissions due to tetanus
increased in India, probably due to improvement in the health
consciousness of the population and in its attitude toward the public
health services [9].
In the 1980s, community-based surveys from India
documented that mortality rates due to neonatal tetanus ranged from less
than 5 to more than 60 per 1000 live births. Tetanus alone was causing
23-72% of all neonatal deaths [11]. There were wide variations in the
different states as well as rural and urban areas of India. Data for
mortality due to neonatal tetanus during 1978-83 shows 5-67 and 0-15
neonatal tetanus deaths per 1000 live births in rural and urban India,
respectively. Highest fatality (67/1000 live births) was in rural Uttar
Pradesh.
Current Scenario
World
Around 49 000 newborns died of neonatal tetanus in
2013 (1% of all neonatal deaths) as compared to around 200 000 deaths
(7% of newborn deaths) in the year 2000. Number of countries that have
not eliminated maternal and neonatal tetanus has come down from 59 in
2000 to 19 in 2016 (Table I). Augmentation of
supplementary immunization activities under MNTE initiative has led to
vaccination of more than 170 million women of reproductive age [4,12].
Deliveries conducted by skilled health personnel have also increased
from 59% in 1990 to 71% in 2014.
TABLE I Countries Which Have Not Eliminated Maternal Neonatal Tetanus by 2016.
|
Country |
Maternal Mortality Ratio*
|
|
1 |
Afghanistan |
396 |
|
2 |
Angola |
477 |
|
3 |
Central African republic |
882 |
|
4 |
Chad |
856 |
|
5 |
Congo (DRC) |
442 |
|
6 |
Equatorial Guinea |
342 |
|
7 |
Ethiopia |
356 |
|
8 |
Guinea |
679 |
|
9 |
Haiti |
359 |
|
10 |
Kenya |
510 |
|
11 |
Mali |
587 |
|
12 |
Nigeria |
814 |
|
13 |
Pakistan |
178 |
|
14 |
Papua New Guinea |
215 |
|
15 |
Philippines |
114 |
|
16 |
Somalia |
732 |
|
17 |
Sudan |
311 |
|
18 |
South Sudan |
789 |
|
19 |
Yemen |
385 |
*UNICEF. Trends in Maternal Mortality 1990 to 2015. Estimates by
WHO, UNICEF, UNFPA, World Bank Group and the United
Nations Population Division. (http://data.unicef.org/corecode/uploads/document6/uploaded_pdfs/corecode/MMR_executive_summary_
final_mid-res_243.pdf.)
Data Source: Sample Registration System, Government of India and
WHO 2015 global summary of vaccine preventable diseases. |
India
In 1988, 11 849 cases of neonatal tetanus were
reported from India while only 492 were reported in 2014 (95.8%
reduction) [13]. India was declared free of maternal and neonatal
tetanus on 15th May, 2015. Andhra Pradesh was the first, and Nagaland
the last Indian state to achieve the elimination goal [3]. Various
factors contributed to its early elimination from Andhra Pradesh, much
before the rest of India [14]. Tetanus toxoid immunization to all
pregnant women was started in 1979 in the State, as compared to 1983 in
rest of the country. Cash incentives were given to cover the costs
associated with institutional deliveries, and there was a high political
commitment for the cause, leading to increased recruitment of auxiliary
nurse midwife (ANMs). Also, there was an increase in village-level
promotional material on vaccination, and 24-hour service provided in
most peripheral health centers (PHCs).
Strategies Which Helped India Achieve Neonatal
Tetanus Elimination
There has been an overall 44% reduction in neonatal
deaths in India between 1990 (13,54,000) to 2012 (7,58,000). But this
reduction has not been uniform across India. While some states have a
single-digit neonatal mortality rate (NMR), others have an NMR more than
30 [15]. India, in particular, faced unique challenges because of its
economic, cultural, and demographic diversities.
A Cochrane systematic review suggests that a two or
three dose course of tetanus toxoid to pregnant mothers provides
protection against neonatal deaths [16]. Tetanus vaccination of pregnant
women was included in India’s National Immunization Policy in the year
1983. According to NFHS-3 data (2005-06), around 82% of pregnant women
registered for antenatal care were receiving second dose of tetanus
toxoid or booster [17].
Neonatal tetanus had decreased significantly in
developed countries even before tetanus toxoid vaccine was being given
during pregnancy [10]. The main factors responsible were safe delivery
practices and cord care. Moreover the TT2 coverage had remained steady
in India, and had rather decreased in 2013 [14]. It indicates that other
factors have also played an important part in elimination of maternal
and neonatal tetanus from India. Many program have been introduced in
India in the last 25 years to address maternal and newborn health (Table
II) [15].
Table II Maternal and Child Health Programs in India
|
Year of launch |
Health program |
|
1992 |
Child Survival and Safe Motherhood (CSSM) |
|
1997 |
Reproductive Child Health-I (RCH-I) |
|
2005 |
Reproductive Child Health-II (RCH-II)
|
|
2005 |
National Rural Health Mission (NRHM) |
|
2013 |
Reproductive, Maternal, Newborn, Child and Adolescent Health
(RMNCH+A)
|
|
2013 |
National Health Mission (NHM) |
|
2014 |
India Newborn Action Plan (INAP) |
Though the dose and schedule for tetanus vaccination
has remained same in each of these programs, it is probably the focus on
integrating the reproductive health services and a goal-directed
approach that has helped India to eliminate MNT. Under the’Child
Survival and Safe Motherhood Program’, emphasis was laid on training of
traditional birth attendants and strengthening of first referral units
so that they deal better with high-risk obstetric emergencies [18]. The
‘Reproductive and Child Health’ programs stressed on 24 hour delivery
services at PHCs and referral facilities, and training of MBBS doctors
in emergency obstetric management, to improve skilled birth attendance.
Policy decisions were made to permit health workers to use drugs in
emergency situations to reduce maternal mortality [19]. Government of
India launched Janani Suraksha Yojna (JSY) in 1995 offering conditional
cash transfers. This led to a quantum increase in institutional
deliveries from 26% (NFHS-1, 1992-93) to 72.9% (Coverage Evaluation
Survey, 2009). National Rural Health Mission (NRHM) introduced several
other interventions for maternal and neonatal health in 2005 [3]:
• Village health and nutrition days were started
to increase coverage of TT-containing vaccines in children and
pregnant females;
• All skilled birth attendants were trained for
3-weeks;
• Peripheral health centers were enabled to
provide round the clock maternal and neonatal care services;
• Facility-based neonatal care (FBNC) was
strengthened. Newborn care corners were set up in maternity
facilities; Special neonatal care units were started in district
hospitals; and Newborn stabilization units were established at first
referral units;
• More than 8.9 million accredited social health
activists (ASHAs) were employed to augment the use of health
facilities;
• Skilled birth attendants were given free
disposable delivery kits for distribution to pregnant women; and
• Institutional deliveries were promoted, more so
in pregnant females of lower socio-economic status.
This program was supplemented by Janani Shishu
Suraksha Karyakram (JSSK) in 2011. Under this program, free maternity
services and newborn care were provided by all government health care
institutions. Both the mother and her newborn are entitled to get free
diagnostic services, free drugs including blood transfusion, free diet,
and free referral transport with drop back facility [20]. An
observational study published in 2012 [21] showed that institutional
deliveries increased by 42.6% after implementation of the JSY scheme,
including those among lower socioeconomic strata. With increase in safe
delivery practices, maternal mortality as well as incidence of neonatal
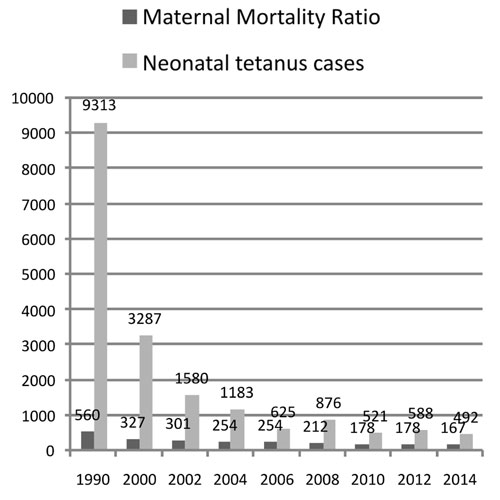
tetanus cases have declined (Fig. 1). Intensive
communication program promoting 5 cleans (clean hands, delivery
surfaces, instruments for cutting the umbilical cord, cord tie and
caring of the umbilical cord) have also contributed to the increase in
safe deliveries [3]. Incentives for ASHAs were also increased in 2012.
 |
|
Fig. 1 Neonatal tetanus cases and
maternal mortality ratio, India (1990-2014).
|
Another strategy used for neonatal tetanus
elimination was the use of a high-risk approach in certain
high-incidence states of India, like Rajasthan. Under this approach,
supplementary immunization activities were conducted in these states to
vaccinate >80% of all women of childbearing age with three properly
spaced doses of TT vaccine and the promotion of antenatal care with
clean delivery practices [3].
In addition to this, the Ministry of Health and
Family Welfare (MoHFW) has been intensifying the routine immunization by
conducting campaigns like special immunization weeks and Mission
Indradhanush.
Sustaining Maternal And Neonatal Tetanus Elimination
Unlike measles and polio which are amenable to
eradication, it is impossible to eradicate tetanus as the tetanus spores
cannot be completely removed from the environment [12]. Therefore, we
need to make sustained efforts to maintain the tetanus elimination
status.
Strategies which need strengthening are discussed
below [22]:
Routine immunization (RI) coverage: The routine
immunization in India is a part of the NRHM and is administered by the
MoHFW. The vaccination coverage statistics of India are far from
satisfactory. According to the WHO, the coverage of DTP3 and TT2 of
India in 2013 was 83% and 61%, respectively [13]. According to Coverage
Evaluation Survey 2009 conducted by UNICEF, the most common reasons for
partial or no immunization were that the people did not realize the need
for vaccination and also did not know about the vaccines [23]. In order
to sustain maternal and neonatal tetanus elimination status in India,
routine immunization coverage will have to be strengthened. This can be
done by augmenting IEC activities, ensuring adequate cold chain
facilities, deployment of adequate number of medical and paramedical
personnel for immunization, ensuring vaccine safety, monitoring for
adverse events following immunization (AEFIs), and surveillance of
vaccine preventable diseases (VPDs). There is also a need for adequate
training of health personnel for immunization program.
Poor performing districts should be identified and
corrective strategies should be determined. Mission Indradhanush was
launched in 2014 with a goal to vaccinate all children up to two years
of age and pregnant women with all the available vaccines under
universal immunization program [24]. The MoHFW identified high focus
districts in the country which have the highest number of partially
immunized and unimmunized children. Of these, around 40 per cent
districts are in just four states – Uttar Pradesh, Bihar, Madhya
Pradesh, and Odisha. Special immunization drives will be conducted in
these districts to improve routine immunization coverage. More than 20
lakh children were fully vaccinated during phase 1.
Innovation and achieving self-sufficiency in vaccine
production will also go a long way in strengthening RI in India.
Supplementary immunization activities:
Supplementary immunization must complement and not replace routine
immunization. It helps to increase coverage of routine immunization as
well as for catch-up vaccination of unimmunized children. It is one of
the pillars of disease elimination; the other two pillars being routine
immunization and surveillance.
Surveillance: Regular audits of all neonatal
deaths should be done. Continued surveillance of neonatal tetanus cases
is paramount to keep the disease burden in check.
Institutional delivery: More number of ANMs and
ASHAs will have to be trained and regularly incentivized to mobilize
pregnant women to register for antenatal care and safe delivery
practices. Public awareness about government health schemes like JSY and
JSSK and their implementation should be reviewed regularly.
WHO has advised certain strategies to sustain the
MNTE status in India (Box 1) [12]. Unless and until
sustained efforts are made to increase vaccination coverage and safe
deliveries, MNTE status could be difficult to maintain in India.
|
Box 1
WHO Guidelines for Sustaining Maternal and Neonatal Tetanus
Elimination Status [12] |
|
1. To discuss and review annually the
elimination status with main stakeholders including State
immunization officers, data managers, partners, and others as
identified by MoHFW.
2. Maintain the high TT coverage and further
augment it in areas with poor coverage.
3. Increase the rates of booster dose
coverage of children as per national immunization schedule to
ensure life-long protection.
4. Deliveries by skilled birth attendants
should be increased further and neonatal illnesses should be
managed in an integrated program under National Rural Health
Mission.
5. Surveillance.
|
1. Keja K, Chan C, Hayden G, Henderson RH. Expanded
programme on immunization. World Health Stat Q. 1988;41:59-63.
2. Roper MH, Vandelaer JH, Gasse FL. Maternal and
neonatal tetanus. Lancet. 2007;370:1947-59.
3. Maternal and neonatal Tetanus Elimination:
Validation survey in 4 States in India, April 2013. Wkly Epidemiol Rec.
2014;89:177-88.
4. World Health Organization. Maternal and Neonatal
Tetanus (MNT) Elimination. Available from:
http://www.who.int/immunization/diseases/MNTE_initiative/en/index4.html.
Accessed July 25, 2016.
5. India is declared free of maternal and neonatal
tetanus. BMJ. 2015;350:h3092.
6. Schlesinger BE. Proceedings of a Symposium on
Immuni-zation in Childhood. London: Livingstone; 1960. P.73.
7. Matveev KI, Sergeeva TI. Peace-time epidemiology
of tetanus in the USSR and in foreign countries. Zh Mikrobiol Epidemiol
Immunobiol. 1959;30:134-42.
8. Maternal and Neonatal Tetanus Elimination
Initiative. Pampers UNICEF 2010 campaign launch. Available from:
http://www.unicef.org/corporate_partners/files/APPR
OVED_MNT_Report_05.06.10.pdf. Accessed April 25, 2016.
9. Bytchenko B. Geographical distribution of tetanus
in the world, 1951-60. A review of the problem. Bull World Health Organ.
1966;34:71-104.
10. Stanfield JP, Galazka A. Neonatal tetanus in the
world today. Bull World Health Organ. 1984;62:647-69.
11. Basu RN, Sokhey J. A baseline study on neonatal
tetanus in India. Pak Pediatr J. 1982;6:184-97.
12. Maternal and Neonatal Tetanus Elimination:
Validation survey in 4 States and 2 union territories in India, May
2015. Wkly Epidemiol Rec. 2015;90:589-608.
13. WHO vaccine-preventable diseases: monitoring
system. 2015 global summary. Available from: http://apps.who.int/immunization_monitoring/globalsummary/countries?
countrycriteria%5Bcountry%5D%5B%5D=IND&commit =OK. Accessed May 02,
2016.
14. Bairwa M, Sk S, Rajput M, Khanna P, Malik JS,
Nagar M. India is on the way forward to maternal and neonatal tetanus
elimination! Hum Vaccines Immunotherap. 2012;8:1129-31.
15. Ministry of Health & Family Welfare. Government
of India. INAP: India Newborn Action Plan. September 2014. Available
from: http://www.newbornwhocc.org/INAP_ Final.pdf. Accessed May
02, 2016.
16. Demicheli V, Barale A, Rivetti A. Vaccines for
women for preventing neonatal tetanus. Cochrane Database Syst Rev.
2015;7:CD002959.
17. National Family Health Survey-3, India. Available
from: http://rchiips.org/nfhs/pdf/India.pdf. Accessed May 04,
2016.
18. Singh M, Paul VK. Maternal and child health
services in India with special focus on perinatal services. J Perinatol.
1997;17:65-9.
19. Ministry of Health & Family Welfare. Child Health
Programme in India. Available from: http://mohfw.nic.in/WriteReadData/l892s/6342515027file14.pdf.
Accessed May 04, 2016.
20. Ministry of Health and Family Welfare (MOHFW).
Government of India. State of India’s Newborns 2014. Available from:
http://www.newbornwhocc.org/SOIN_ PRINTED%2014-9-2014.pdf. Accessed
May 04, 2016.
21. Gupta SK, Pal DK, Tiwari R, Garg R, Shrivastava
AK, Sarawagi R, et al. Impact of Janani Suraksha Yojana on
institutional delivery rate and maternal morbidity and mortality: an
observational study in India. J Health Popul Nutr. 2012;30:464-71.
22. World Health Organization. Achieving and
Sustaining Maternal and Neonatal Tetanus Elimination. Strategic Plan
2012–2015. Available from: http://apps.who.int/immuni
zation_monitoring/MNTEStrategicPlan_E.pdf. Accessed May 04, 2016.
23. Ministry of Health & Family Welfare. Government
of India. Coverage Evaluation Survey 2009. Available from:
https://nrhm-mis.nic.in/SitePages/Pub_Coverage Evaluation.aspx#.
Accessed May 04, 2016.
24. Ministry of Health & Family Welfare. Government of India. Mission
Indradhanush. Available from:
http://www.missionindradhanush.in/about.html. Accessed May 4, 2016.

