|
|
|
Indian Pediatr 2012;49: 985-986
|
 |
Tracheobronchopathia Osteochondroplastica in a
5-year-old Girl
|
|
Clemax Couto Sant´Anna, Paulo Pires-de-Mello*, Maria de Fátima Morgado*
and
Maria de Fátima Pombo March
From the Faculty of Medicine of Federal University of
Rio de Janeiro and *Respiratory Endoscopy Department of Instituto
Fernandes Figueira. Rio de Janeiro, RJ. Brazil.
Correspondence to: Clemax C Sant´Anna, R Cinco de
Julho 350 ap. 604 – Copacabana, 22051-030.
Rio de Janeiro, RJ. Brazil. Email:
[email protected]
Received: February 14, 2012;
Initial review: March 02, 2012;
Accepted: July 23, 2012.
|
Tracheobronchopathia osteochondroplastica (TO) is considered an orphan
disease with exceptional occurrence in children. We report a 5-year-old
female child who was referred to us with chronic cough and recurrent
pneumonia. After several investigations, bronchoscopy showed multiple
nodules in the tracheobronchial lumen, whose distribution was consistent
with TO. The patient was followed for four years, with no change in the
pattern of the disease.
Key words: Tracheobronchopathia osteochondroplastica,
Recurrent pneumonia.
|
|
Tracheobronchopathia osteochondroplastica
(TO), also known as tracheopathia chondro-osteoplastica or
tracheopathia osteoplastica, is a rare chronic disease of
undetermined etiology. It stems from osteocartilaginous metaplasia
and is characterized by an bronchoscopic finding of multiple
subepithelial nodules that project into the tracheobronchial lumen
and does not affect the lungs or other organs. The nodules may be
present from the larynx to the peripheral bronchi in the
anterolateral tracheal wall. In general, the posterior wall is
spared. This peculiarity is exclusive of this disease and allows the
exclusion of other differential diagnoses. TO is often an endoscopic
finding and its prevalence in bronchoscopic studies is estimated to
range from 1:125 to 1:6000 [1-3]. To date, less than 400 cases have
been reported in the literature, and only four were in children
[1,2,4].
Diagnosis can be made from the typical endoscopic
finding of the disease, dispensing biopsy [1,5,6]. Biopsy, when
done, shows ossification or calcification of the bronchial submucosa
[6].
Case Report
A 5-year-old female child with chronic cough and
a history of chronic cough and recurrent pneumonia since age 3 years
was referred to us. The first episode consisted of right upper lobe
pneumonia that progressed to pneumatocele, resulting in a permanent
cicatrical atelectasis. The other respiratory infection episodes in
the following year were also interpreted as pneumonia but were
based, apparently, on a radiographic image that had persisted since
the first episode: chronic atelectasis of the left lower lobe and
adhesive atelectasis in the right lung. Further examination showed
no signs of atopy. Her pulmonary auscultation was normal. The child
was HIV seronerative and had a normal immunoglobulin profile.
Tuberculin skin test was 6 mm. At the time she was treated as an
outpatient and the disease course was favorable, despite frequent
coughing and two more episodes of respiratory infection and cervical
adenitis treated with antibiotics. At age seven years, she underwent
rigid bronchoscopy, which showed widespread nodular mucosal
irregularity extending from trachea into bronchial tree; irregular
mucosa, intensely friable when touched by the instrument. The left
lower lobe bronchus was not obstructed. Bronchial aspirate was
negative for bacteria (including acid-alcohol-fast bacilli and M.
tuberculosis) and yeasts. The findings were consistent with TO.
Biopsy of bronchial mucosa, which did not include cartilage,
evidenced a nonspecific, chronic inflammatory process with intense
lymphoid hyperplasia in the lamina propria and prevalence of
neutrophils. Outpatient care consisted of occasional courses of
antibiotics and respiratory physiotherapy. At age 8 years,
spirometry was normal. The patient responded well, with occasional,
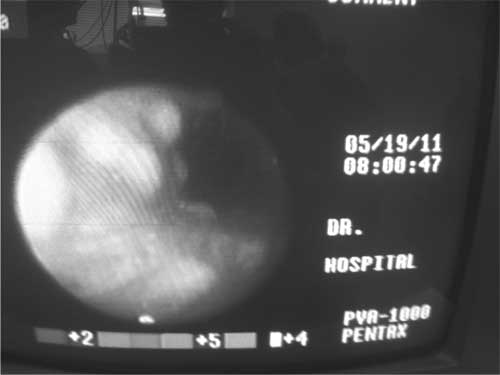
mild respiratory infections. After four years, flexible bronchoscopy
showed similar findings (Fig. 1). The patient is now
11 years old, continues to be followed as an outpatient and has a
favorable course.
 |
|
Fig.1 Nodular mucosal irregularity
of trachea observed on flexible bronchoscopy.
|
Discussion
The present case is relevant because of the
rarity of this disease in children. Moreover, TO lesions did not
deteriorate after four years of follow-up. The disease may remain
stable for a long time or progress insidiously for many years. Rapid
progression leading to tracheal obstruction is singular [2,7].
The clinical findings vary. TO may be mistaken
for asthma because of the wheezing caused by decreased bronchial
diameter. TO may also cause chronic cough [5], dyspnea and
hemoptysis [6] but most patients are asymptomatic [1,6].
This patient had chronic atelectasis of the left
lower lobe, consequent of recurrent pneumonia. Atelectasis could be
explained by obstruction of the bronchial lumen by TO nodules since
their promotion of secretion retention established the vicious cycle
of atelectasis and pneumonias. The patient did not have asthma,
which could be considered an associated condition. However, her
wheezing episodes could be attributed to the partial obstruction of
the bronchial tree by multiple nodules [2,5,7].
The tracheal and bronchial nodules bled easily
and were soft, similar to other reports [1,5]. Since the nodules
bled easily during endoscopy, the tissue collected for biopsy during
the two endoscopic examinations was more superficial. Hence, the
nodules contained no cartilage, only nodular neutrophilic
arrangements [5]. This result ruled out other diseases like
tuberculosis, hypertrophy of bronchial associated lymphoid tissue,
sarcoidosis, etc.
There is no specific treatment for TO. When there
is evidence of bronchial infections, the patient should be treated
with antibiotics, as presently done. The present patient was never
prescribed inhaled corticosteroids, even though they have already
been used for TO treatment in some case series [6,7].
Acknowledgments: Drs. Barbara Almeida and
Eliane Castelo Branco from Clementino Fraga Filho Universitary
Hospital (UFRJ) and Dr. Roberta Gonçalves Silva from IPPMG - Federal
University of Rio de Janeiro. Rio de Janeiro, Brazil.
Contributors: CS´A: drafted and edited the
manuscript; MFM and PPM were involved in endoscopic procedure and
documentation of the case report. MFPM: interpreted the results and
drafted the manuscript. All authors held final responsibility for
the decision to submit for publication.
Funding: None; Competing interests:
None stated.
References
1. Chroneau A, Zias N, Gonzalez AV, Beamis Jr JF.
Tracheobronchopathia osteochondroplastica: an underrecognized
entity? Monaldi Arch Chest Dis. 2008;69:65-9.
2. Lazor R, Cordier JF. Tracheobronchopathia
osteochondro-plastica. Orphanet encyclopedia, June 2004. Available
at http://www.orpha.net/data/patho/GB/uk-TO.pdf. Accessed on 27
January, 2012.
3. Wilks S. Ossific deposits on larinx, trachea
and bronchi. Trans Pathol Soc London. 1857;8:88.
4. Simsek PO, Oxcelik U, Demirkazik F, Unai OF,
Diclehan O, Aslan A, et al. Tracheobronchopathia
osteochondro-plastica in a 9-year-old girl. Pediatr Pulmonol.
2006;41:95-7.
5. Willms H, Wiechmann V, Sack U, Gillissen A.
Tracheobronchopathia osteochondroplastica: a rare cause of chronic
cough with haemoptysis. Cough. 2008;4:4.
6. Ryu JH, Maldonado F, Tomassetti S. Idiopathic
tracheopathies. Eur Resp Mon. 2011;54:187-200.
7. Pinto JA, Silva LC, Perfeito DJP, Soares JS.
Ostheochondroplastic tracheobronchopathy: report on 2 cases and
bibliographic review. Braz J Otorhinolaryngol. 2010;76:789-93.
|
|
|
 |
|

